Journal Name: International Journal of Cancer and Treatment
Article Type: Research
Received date: 27 August, 2018
Accepted date: 30 August, 2018
Published date: 03 September, 2018
Citation: Niyonzima J P, Matabelle L B, Ntasumbumuyange D, Rulisa S (2018) Cervical Cancer Prevention Knowledge and Attitudes: Survey of Midwives and Nurses in Rwanda. Int J Cancer Tremnt. Vol: 1, Issu: 1 (30-34).
Copyright: © 2018 Niyonzima J P. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Objective: The plan for cervical cancer control in Rwanda includes expansion of cervical cancer screening via Visual Inspection with Acetic Acid (VIA) into all health clinics and District Hospitals. The initial step of cervical cancer screening is conducted by nurses and midwives within the context of routine health care visits, and positive cases are referred to colposcopy clinics. The aim of this study is to evaluate knowledge, awareness, attitudes and practices of midwives and nurses regarding cervical cancer prevention.
Methods: A descriptive cross-sectional study was conducted among midwives and nurses working in four hospitals in Kigali City. The study included one tertiary hospital, Centre Hospitalier Universitaire de Kigali (CHUK), and three secondary level hospitals, Muhima, Kibagabaga and Masaka. During a 3-month period, from October 2016 to December 2016 self-administered questionnaires were distributed to nurses and midwives in the department of obstetrics and gynecology at each hospital. The questionnaire comprised 50 true or false questions. This study was conducted with an exhaustive approach. After filling in the hard copy, data entry was done using Epidata3.1 and was exported to SPSS 23 for statistical analysis.
Results: A total number of 587 midwives and nurses were present at selected hospitals during the study period. Among them 527(89.7%) participated in the study and filled in the questionnaire completely. Most of midwives could identify symptoms and risk factors for cervical cancer, however some misidentified IUD (39.1%), poor personal hygiene (35.5%) and use of herbal remedies (19.5%) as risk factors for cervical cancer. Midwives and nurses working at CHUK had better knowledge of symptoms and risk factors of cervical cancer than those working in district hospitals. A quarter of respondents thought HPV vaccine was dangerous for a person’s health. About 90% of midwives and nurses would recommend a screening program in their community though only 32.9% of female respondents had ever been screened for cervical cancer themselves. However, there was no statistical difference in knowledge of preventive methods between screened participants and those who had not been screened.
Conclusion: This study showed good knowledge of symptoms and risk factors of cervical cancers in obstetric and gynecologic nurses and midwives at the hospitals studied. However, there are still many misconceptions about risk factors for cervical cancer. If midwives and nurses were sensitized and their knowledge improved, they could play a pivotal role in the fight against cervical cancer since they are the primary health care providers to most of Rwandan population.
Keywords
Acetic acid, Human papilloma virus, Intrauterine device, Human immunodeficiency virus, Lugol’s iodine.
Abstract
Objective: The plan for cervical cancer control in Rwanda includes expansion of cervical cancer screening via Visual Inspection with Acetic Acid (VIA) into all health clinics and District Hospitals. The initial step of cervical cancer screening is conducted by nurses and midwives within the context of routine health care visits, and positive cases are referred to colposcopy clinics. The aim of this study is to evaluate knowledge, awareness, attitudes and practices of midwives and nurses regarding cervical cancer prevention.
Methods: A descriptive cross-sectional study was conducted among midwives and nurses working in four hospitals in Kigali City. The study included one tertiary hospital, Centre Hospitalier Universitaire de Kigali (CHUK), and three secondary level hospitals, Muhima, Kibagabaga and Masaka. During a 3-month period, from October 2016 to December 2016 self-administered questionnaires were distributed to nurses and midwives in the department of obstetrics and gynecology at each hospital. The questionnaire comprised 50 true or false questions. This study was conducted with an exhaustive approach. After filling in the hard copy, data entry was done using Epidata3.1 and was exported to SPSS 23 for statistical analysis.
Results: A total number of 587 midwives and nurses were present at selected hospitals during the study period. Among them 527(89.7%) participated in the study and filled in the questionnaire completely. Most of midwives could identify symptoms and risk factors for cervical cancer, however some misidentified IUD (39.1%), poor personal hygiene (35.5%) and use of herbal remedies (19.5%) as risk factors for cervical cancer. Midwives and nurses working at CHUK had better knowledge of symptoms and risk factors of cervical cancer than those working in district hospitals. A quarter of respondents thought HPV vaccine was dangerous for a person’s health. About 90% of midwives and nurses would recommend a screening program in their community though only 32.9% of female respondents had ever been screened for cervical cancer themselves. However, there was no statistical difference in knowledge of preventive methods between screened participants and those who had not been screened.
Conclusion: This study showed good knowledge of symptoms and risk factors of cervical cancers in obstetric and gynecologic nurses and midwives at the hospitals studied. However, there are still many misconceptions about risk factors for cervical cancer. If midwives and nurses were sensitized and their knowledge improved, they could play a pivotal role in the fight against cervical cancer since they are the primary health care providers to most of Rwandan population.
Keywords
Acetic acid, Human papilloma virus, Intrauterine device, Human immunodeficiency virus, Lugol’s iodine.
List of Abbreviation
- CHUK: Centre Hospitalier Universitaire de Kigali
- HPV: Human Papilloma Virus
- HIV: Human Immunodeficiency Virus
- IUD: Intrauterine device
- IRB: Institutional Review Board
- VIA: Visual Inspection with Acetic acid
- VILI: Visual Inspection with Lugol’s iodine
- WHO: World Health Organization
Introduction
Cervical cancer ranks fourth among cancer in women worldwide and is the second most common in women aged 15-44years old [1-9]. Almost all cases of cervical cancers arise from infection with human papilloma virus (HPV). This infection can progress to neoplasia or clear spontaneously depending on other host factors. Worldwide, there were an estimated 528,000 new cases of cervical cancer in 2012 with 266,000 deaths from cervical cancer. Seventy percent of these deaths occurred in developing countries [1-8]. Cervical cancer represents 22.5% of all cancers in women of Sub-Saharan Africa.
Among Rwandan population of 11millon, 2.72 million are women aged 15years or older. This group is at risk of developing cervical cancer [1]. Nearly a thousand women are diagnosed with cervical cancer each year and there are 700 deaths attributed to cervical cancer every year. This makes cervical cancer the most common cancer in women in the country [1]. Rwanda also has a higher incidence of cervical cancer at 49 per 100,000women, compared to the East African region at 34.5 per 100,000. This is much higher than the worldwide incidence of 16 per 100,000 women.
Cervical cancer is preceded by a long latency with recognizable precancerous lesion. Because of this long latency period, cervical cancer screening during this time can be very effective identifying and addressing precancerous lesions. There are multiple different techniques available for screening, dependent on resources available, including cytology, HPV tests, Visual inspection with Acetic acid (VIA), and Visual inspection with Lugol’s iodine (VILI). This makes screening an effective means of prevention of cervical cancer even in low resource countries since precancerous lesions can be managed expectantly or treated safely and inexpensively in outpatient setting. The disparity between developing countries and high-income countries in cervical cancer diagnosis and related deaths is mainly due to low uptake of screening in developing countries [3-12].
The World Health Organization (WHO) recommends the involvement of all health care providers in cervical cancer prevention. Primary prevention involves: avoiding exposure to HPV infection as well as vaccination against HPV, and secondary prevention involves screening [4]. The first step to achieve this goal is to make sure that health care providers have appropriate knowledge and attitudes about cervical cancer and its prevention. They should be able to explain the value and mode of preventive methods of cervical cancer to diverse communities in unbiased way. Very often, nurses and midwives are the first and/or only health care provider a patient may encounter, so their knowledge and attitudes in this area are extremely important.
In 2010, the Rwandan government launched a training program for healthcare providers in the “screen and treat” approach. This utilizes VIA screening and immediate cryotherapy of the cervix for suspicious precancerous lesions. The program targeted women between 30 and 50 of age [1]. In 2011 the Ministry of Health initiated a national cervical cancer campaign with administration of HPV vaccine for all girls 11-12 years old for HPV vaccine. After 2 years 227,246 girls had completed all three doses of HPV vaccine [5]. The Rwanda Demographic Health Survey (DHS) 2010 showed that 21% of Rwandan women aged 25-49 years were sexually active by age 18 and 3% of women and men have had sex by age 15. This makes primary and secondary prevention efforts a cornerstone in the fight against cervical cancer since early sexual debut (< 20years) is one of the risk factors for cervical cancer.
Rwanda has 625physicians, 8327 nurses and240 midwives. They work throughout 2 teaching hospitals, 4 referral hospitals, 5 regional hospitals, 41 district, and 442 health centers [6]. Often, women of childbearing age only seek medical care surrounding birth events. Midwives and nurses who come in contact with these mothers could play an important role in sensitizing patients about cervical cancer prevention if these activities were integrated into the scope of their daily work. Although the WHO cervical cancer prevention recommendations are part of the training for midwives and nurses, their knowledge, attitudes, and practices toward cervical cancer and its prevention are not well known. This study was designed to assess the knowledge, attitudes and practices of midwives and nurses in Kigali, Rwanda surrounding cervical cancer and its prevention.
Materials and Methods
A descriptive cross-sectional study was conducted among midwives and nurses working in four hospitals in Kigali City. One tertiary hospital CHUK and three secondary level hospitals: Muhima, Kibagabaga and Masaka. This study was reviewed by the Institutional Review Board (IRB) at University of Rwanda, College of Medicine and Health Sciences. Before starting, the study was presented to and approved by each hospital administration. During a 3-month period, from October 2016 to December 2016, self-administered questionnaires were distributed in the department of obstetrics and gynecology CHUK, Muhima, Kibagabaga and Masaka hospitals. The questionnaire was comprised of 50 true or false questions.
This is study was conducted with an exhaustive approach. Midwives and nurses were recruited during the morning staff meetings and those who did not attend that day were recruited in next staff meeting. On average we visited each hospital 4 times. Participants agreed to participate by signing a written consent. After filling in the hard copy, data entry was done using Epidata3.1 and was exported to SPSS 23 for statistical analysis. Chi square test was used for statistical significance.
Results
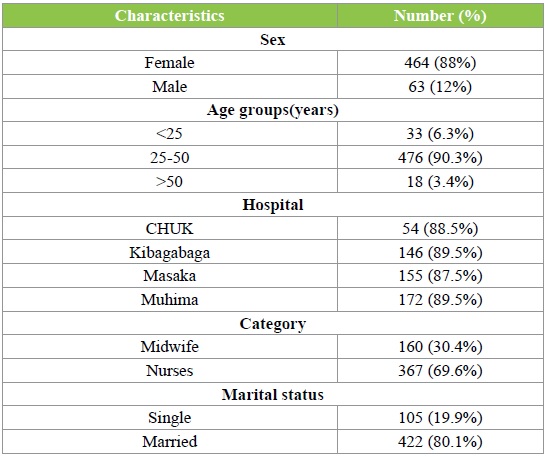
Study population (Table 1)
A total number of 587 midwives and nurses were present at selected hospitals during the study period, of which 527 (89.7%) participated in the study and completed the questionnaire. Muhima and Kibagabaga hospitals had the highest participation rate (89.5%), followed by CHUK (88.5%) and Masaka hospital 87.5%. 88% were female and the majority were between 25 to 50 years of age (90.3%). Most of the participants were married (80.1%) and there were 367 (69.6%) nurses and 160 (30.4%) midwives.
Table 1: Demographics of respondents.
Knowledge of symptoms and risk factors of cervical cancer (Table2)
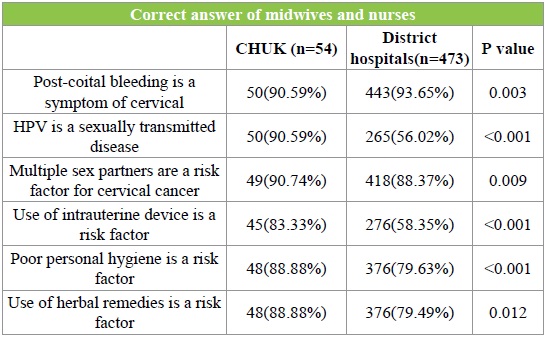
Post-coital bleeding was identified as a symptom of cervical cancer by 93.5% of participants while 76.5% recognized that HPV infection was present in more than 50% of cervical cancers. Only 59.5% knew HPV was sexually transmitted. 47% thought cervical cancer was most common in women in their twenties, 70% thought it could be diagnosed at early stage because of obvious symptoms and 94.1% believed that it is possible to detect precancerous lesions. 206 nurses and midwives (39%) incorrectly identified intrauterine device (IUD) as a risk factor for cervical cancer, as well as poor personal hygiene (35.4%) and use of herbal remedies (19.5%). Infection with HIV, multiple sex partners, cigarette smoking, and early coitus were correctly recognized as risk factors of cervical cancer by 300 (56.9%), 467 (88.7%), 298 (56.7%) and 439 (83.3%) respectively. (Table 2) Midwives and nurses working at CHUK had better knowledge of symptoms and risk factors of cervical cancer than those working in district hospitals (P < 0.001). Specifically, they had improved knowledge about the mode of transmission of HPV and fewer incorrectly identified the use of IUD and poor personal hygiene as risk factors for cervical cancer. (Table 3).
Table 2: Knowledge and awareness of symptoms and risk factors of cervical cancer.
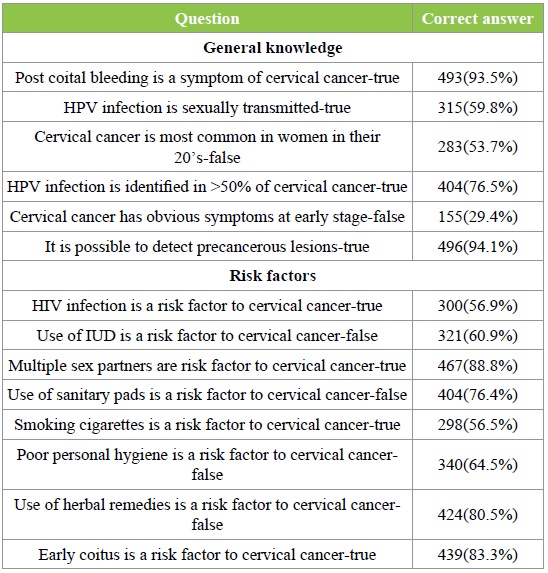
Table 3: Comparison of knowledge between participants working at CHUK and those working at districts hospitals.
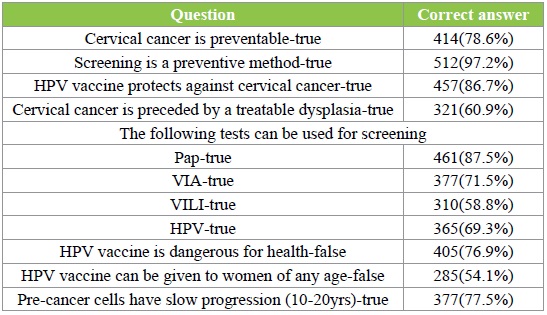
Prevention of cervical cancer (Table 4)
Cervical cancer was identified as a preventable disease by 414 (78.6%) participants and almost all midwives and nurses 512 (97.2%) recognized screening as a preventive method. Pap test was the most widely known method of screening method by 461 (87.5%) respondents and VILI the least known screening method familiar to 310 (58.8%). HPV vaccine was deemed to be protective against cervical cancer by 457 (86.7%), although 122 (23.1%) respondents thought the vaccine to be dangerous for health and 285 (54.1%) participants believed the vaccine could be given to every woman regardless of age. Over 70% of respondents knew the progression from pre-cancer cells to cervical cancer can take up to 20 years, but fewer 321 (60.9%) knew these precancer cells were treatable.
Table 4: Knowledge about cervical cancer prevention.
Attitudes and practices
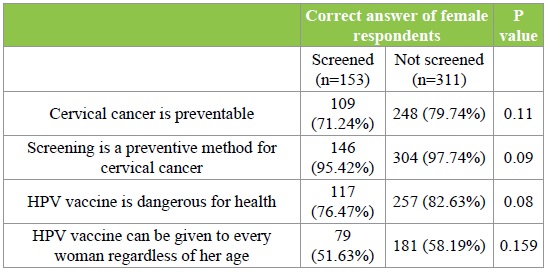
When asked if they would recommend the cervical cancer vaccine, 470 (89.2%) of respondents answered positively. More than half of participants 270 (51.2%) thought their patients had more pressing health issues rather than cervical cancer and 178 (33.8%) agreed that they do not have enough time to talk to their patients about cervical cancer. Although 487 (92.4%) recognized cervical cancer as essential part of women’s health care only 153 (32.9%) of female respondents had ever screened for cervical cancer themselves. (Table 5).However there was no statistical difference in knowledge of preventive methods between participants who had been screened for cervical cancer and those who had not. (Table 6).
Table 5: Attitudes and practice towards cervical cancer.
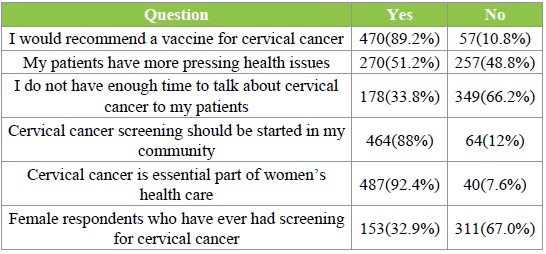
Table 6: comparison between female respondents who had screening of cervical cancer and those who had not.
Discussion
This study was conducted six years after the Rwandan government launched a screening program for cervical cancer which utilizes a “screen and treat” approach. One year after starting that program, the HPV vaccine was also introduced for girls aged 11-12 [1,2]. The purpose of this study was to assess the knowledge of midwives and nurses about cervical cancer and its prevention. The findings of this study show that the level of knowledge of cervical cancer by midwives and nurses in Kigali, Rwanda is comparable to other studies in developing countries, specifically in Sub-Saharan Africa [3,4,10,12,14]. The overall awareness of cervical cancer symptoms and the role of preventive methods were good in this study. Cervical cancer was identified as a preventable disease by 78.6% of participants and almost all midwives and nurses 97.2%recognized screening as a preventive method. Similar results were found in a study done in Ethiopia [3] where 85% of health care workers recognized cervical cancer as a preventable disease and 87% knew screening was important for prevention of cervical cancer. The high level of knowledge among health care workers in Ethiopia could be due to the presence of doctors among the study population.
One of the means to prevent cervical cancer is screening and detection of precancerous lesions. The knowledge of various screening methods was high among the study population; with pap smear being the most known at 87.5%. Previous studies done in Cameroon and Cote d’Ivoire also showed a good knowledge of preventive methods. However, VIA was better known in our study (71.5%) than it was in Cameroon (38%) or Cote d’Ivoire (53.9%) [4-14]. It is likely that knowledge of VIA was higher in our study because it is the most widely available screening test for cervical cancer in Rwanda and the screening done almost exclusively at the hospitals where the survey was performed.
Identifying and avoiding risk factors for cervical cancer is an important aspect in the fight against cervical cancer and women should be educated about those risk factors. In the current study, a high proportion of midwives and nurses identified multiple sex partners (88.8%) and early coitus (88.3%) as risk factors for cervical cancer. In a study conducted in Cote d’Ivoire, 85.5% of midwives similarly identified multiple sex partners as risk factors for cervical cancer and 80.1% recognized early sexual debut as a risk factor [4].
In this study, midwives and nurses working at CHUK had better knowledge of cervical cancer than those working in district hospitals (p < 0.001). Similar results were found in Cote d’Ivoire where midwives working at University hospitals (tertiary level) scored higher on the oncogenic role of HPV than those working in general hospitals (78.4%vs. 63.4%), at the secondary level (p < 0.001) [4]. This result is not unexpected since nurses and midwives working at tertiary level hospitals are specialized and work with gynecologist specialists which likely expose them to more information about cervical cancer. Also, the University hospital setting in general has more teaching and learning opportunities by nature than a secondary level hospital.
Overall, 89.2% of respondents in this study would recommend HPV vaccine, although 23.1% thought the vaccine was not safe. A study performed in Cameroon [14] found that 89% of health care providers recommend the HPV vaccine but 75% thought the vaccine was not safe.14The difference in the perception of safety of the HPV vaccine may be due to the Rwandan respondent’s exposure to immunization programs. Rwanda ranks among some of the highest HPV vaccination rates in developing countries. Only 32.9% of female participants in this study have had cervical cancer screening. Similar low uptake of screening among health care providers was found in other developing countries such as Cote d’Ivoire, Cameroon and India [4,14- 15].
The study strength is that it reached 89.7% of the targeted population and all questionnaires were filled and returned to us. The results accurately represent the knowledge, attitudes and practices of midwives working at the selected hospitals. Limitations to this study are that it did not include nurses and midwives working at private clinics where patients at a higher socioeconomic status consult and may seek screening more often than those in public hospitals. Also, all of the selected hospitals are located in Kigali, an urban area, where all have started screening programs for cervical cancer. Midwives and nurses working in these locations may have better knowledge than those working in rural areas where such programs have not yet been initiated.
Conclusion
This study showed an overall good knowledge of symptoms and risk factors of cervical cancer by midwives and nurses at the hospitals studied. However, there are still misconceptions about risk factors for cervical cancer and the HPV vaccine, as well as limited uptake of cervical cancer screening in this population.
Further studies are needed to assess the barriers to cervical cancer screening among midwives and nurses and why some believe the HPV vaccine is not safe. It would also be useful to assess the knowledge of midwives and nurses working in private clinics and in rural areas of the country. If sensitized and their knowledge improved, midwives and nurses could play a pivotal role in the fight against cervical cancer as the primary health care providers to most of the Rwandan population.
There is no references


