Journal Name: International Journal of Cancer and Treatment
Article Type: Research
Received date: 08 January, 2019
Accepted date: 22 January, 2019
Published date: 30 January, 2019
Citation: Zawam H, Salama R, Gaber M, Naseef C (2019) Factors Affecting the Outcome of Febrile Neutropenia in Patients with Hematologic Malignancies. Int J Cancer Tremnt Vol: 2, Issu: 1 (01-06).
Copyright: © 2019 Zawam H. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Background: Febrile neutropenia (FN) is one of the most serious complications in patients (pts) with hematological malignancies. The prompt initiation of empirical antibiotics within 1 hour of fever has led to reduction of mortality and improvement of survival. Several risk assessment guidelines have been adopted to identify pts as low and high risk of complications. We conducted this single institution study to determine specific risk factors that may affect the outcome in pts with FN. Aim: To identify specific factors that may affect the response to treatment in pts with febrile neutropenia. Methods: During the period of 1st of April 2014 until the end January 2015, pts with hematological malignancies who presented to clinical oncology department and developed FN during management were enrolled in this prospective analysis. At the onset of fever, pts underwent complete physical examination, in addition to blood culture, urine and stool culture. Computer tomography of the chest and paranasal sinuses and serial galactomannan (GM) test were requested in cases with uncontrolled fever or suspected invasive fungal infection (IFI). Polymerase chain reaction analysis of bacteria and fungi from the blood and Broncho alveolar lavage were performed in selected cases. The data were analyzed using chi-square test. Results: One hundred and thirty-five (135) pts were identified and analyzed. The mean age was 38.5 years (range 14-76). 51% had acute myeloid leukemia, 36% acute lymphoblastic leukemia (ALL), non-Hodgkin’s lymphoma, chronic lymphocytic leukemia, and multiple myeloma were diagnosed in 7%, 4%, and 2% respectively. According to Multinational Association for Supportive Care in Cancer (MASCC) index, 80 pts (60%) were categorized as high MASCC score (<21), while 55 pts (40%) had low MASCC score (>21). Blood culture was negative in 114 pts (84%), while it was positive in 21 pts (16%). Gram negative bacteria constituted 60% of cases, while gram positive were 40%. Serial test was positive in 24 pts only (17%), 88 pts (65%) did not receive antifungal agent. Fluconazole was used as antifungal prophylaxis in the majority of pts (n=95) (71%), of those who did not receive fluconazole (n=40), only 15 pts (37.5%) developed IFI and were classified according to 2008 European organization for research and treatment of cancer/invasive fungal infections cooperative group and the national institute of allergy and infectious diseases mycoses study group (EORTC/MSG) Consensus; 12 pts had probable fungal infections, 2 pts had possible fungal infections and 1 patient had definitive fungal infection. The choice between first line antibiotics (ceftazidime, maxipime, imipenem) or antifungal had no impact on the recurrence of FN attacks (P<0.08 and p<0.23 respectively). In terms control of fever on 1st line antibiotics, there was statistically significant difference in favor of low risk MASCC score (p<0.001), change of antibiotics due to uncontrolled fever was required in 62 pts (45%), there was a significant difference between effervescence and low/ high MASCC score (P<0.001). With respect to first antifungal used, a significant correlation was observed between low/ high MASCC score and control on first antifungal therapy (P<0.006). In the present study, 16 pts (12%) only were diabetics, there was no significant correlation between diabetes and uncontrolled fever, prolonged neutropenia. Prolonged FN (>7days) was observed in 40 of pts, the use of corticosteroids, and non-administration of granulocyte colony stimulating factor (G-CSF) were the predominant risk factors (P<0.001, P<0.002 respectively). In terms of mortality, only pts with high MASCC score(n=11) (8%) had the worst outcome compared to low score(n=1) (P<0.0001). Summary/Conclusion: There are multiple factors that may affect the outcome of pts with FN and it should be taken in considerations during management of FN such as MASCC score, previous use of corticosteroid and G-CSF administration during FN.
Keywords
Febrile neutropenia, Outcome, Risk factor.
Abstract
Background: Febrile neutropenia (FN) is one of the most serious complications in patients (pts) with hematological malignancies. The prompt initiation of empirical antibiotics within 1 hour of fever has led to reduction of mortality and improvement of survival. Several risk assessment guidelines have been adopted to identify pts as low and high risk of complications. We conducted this single institution study to determine specific risk factors that may affect the outcome in pts with FN. Aim: To identify specific factors that may affect the response to treatment in pts with febrile neutropenia. Methods: During the period of 1st of April 2014 until the end January 2015, pts with hematological malignancies who presented to clinical oncology department and developed FN during management were enrolled in this prospective analysis. At the onset of fever, pts underwent complete physical examination, in addition to blood culture, urine and stool culture. Computer tomography of the chest and paranasal sinuses and serial galactomannan (GM) test were requested in cases with uncontrolled fever or suspected invasive fungal infection (IFI). Polymerase chain reaction analysis of bacteria and fungi from the blood and Broncho alveolar lavage were performed in selected cases. The data were analyzed using chi-square test. Results: One hundred and thirty-five (135) pts were identified and analyzed. The mean age was 38.5 years (range 14-76). 51% had acute myeloid leukemia, 36% acute lymphoblastic leukemia (ALL), non-Hodgkin’s lymphoma, chronic lymphocytic leukemia, and multiple myeloma were diagnosed in 7%, 4%, and 2% respectively. According to Multinational Association for Supportive Care in Cancer (MASCC) index, 80 pts (60%) were categorized as high MASCC score (<21), while 55 pts (40%) had low MASCC score (>21). Blood culture was negative in 114 pts (84%), while it was positive in 21 pts (16%). Gram negative bacteria constituted 60% of cases, while gram positive were 40%. Serial test was positive in 24 pts only (17%), 88 pts (65%) did not receive antifungal agent. Fluconazole was used as antifungal prophylaxis in the majority of pts (n=95) (71%), of those who did not receive fluconazole (n=40), only 15 pts (37.5%) developed IFI and were classified according to 2008 European organization for research and treatment of cancer/invasive fungal infections cooperative group and the national institute of allergy and infectious diseases mycoses study group (EORTC/MSG) Consensus; 12 pts had probable fungal infections, 2 pts had possible fungal infections and 1 patient had definitive fungal infection. The choice between first line antibiotics (ceftazidime, maxipime, imipenem) or antifungal had no impact on the recurrence of FN attacks (P<0.08 and p<0.23 respectively). In terms control of fever on 1st line antibiotics, there was statistically significant difference in favor of low risk MASCC score (p<0.001), change of antibiotics due to uncontrolled fever was required in 62 pts (45%), there was a significant difference between effervescence and low/ high MASCC score (P<0.001). With respect to first antifungal used, a significant correlation was observed between low/ high MASCC score and control on first antifungal therapy (P<0.006). In the present study, 16 pts (12%) only were diabetics, there was no significant correlation between diabetes and uncontrolled fever, prolonged neutropenia. Prolonged FN (>7days) was observed in 40 of pts, the use of corticosteroids, and non-administration of granulocyte colony stimulating factor (G-CSF) were the predominant risk factors (P<0.001, P<0.002 respectively). In terms of mortality, only pts with high MASCC score(n=11) (8%) had the worst outcome compared to low score(n=1) (P<0.0001). Summary/Conclusion: There are multiple factors that may affect the outcome of pts with FN and it should be taken in considerations during management of FN such as MASCC score, previous use of corticosteroid and G-CSF administration during FN.
Keywords
Febrile neutropenia, Outcome, Risk factor.
Introduction
Febrile neutropenia (FN) is one of the most serious complications in patients with hematological malignancies. Prior to the era of empiric antibiotic therapy, infections accounted for most episodes of neutropenic fever and approximately 70 percent of the mortality in neutropenic acute leukemia patients [1]. Prognosis is worst in patients with proven bacteremia with mortality rates of 18% in Gramnegative and 5% in Gram-positive bacteria [2]. Assessment of risk of complications of severe infection should be undertaken at presentation of fever. Risk assessment may determine the type of empirical antibiotics therapy (oral versus intravenous), venue of treatment (inpatients versus outpatients) and duration of antibiotics therapy [3].
A variety of risk models have been studied to identify patients, disease and treatment related factors with risk for developing neutropenia and its associated complications. The Infectious Diseases Society of America (IDSA) [4], the European Society of Medical Oncology (ESMO) [5], the National Comprehensive Cancer Network (NCCN) [6], and the American Society for Clinical Oncology (ASCO) [6] recommend that an assessment of risk (high risk versus low risk) for neutropenic fever-related medical complications should be obtained at the time of the initial assessment of the neutropenic fever episode. The multinational association for supportive care in cancer (MASCC) Risk scoring index accurately identifies those at low risk for complication. The MASCC index was validated in a prospective multinational study where a MASCC score at least 21 was identified as low risk patients with a predictive value of 91%, specificity of 68% and sensitivity of 71% [7].
The aim of the study was to determine various risk factors that could affect the outcome of febrile neutropenia in patients with hematological malignancies.
Patients and Methods
Between first of April 2014 and 31 January 2015, 135 adult patients with hematological malignancies who presented to Kasr Al-Ainy center of clinical oncology, Cairo University, and developed FN during their management were enrolled in this prospective study.
Neutropenia is defined as an absolute neutrophil count (ANC) of less than 500/ μ L or less than 1000 μ L with anticipated decline to less than 500 μ L in the next 48-hour period. Neutropenic fever is a single oral temperature of 38.3 °C (101 °F) or a temperature of greater than 38.0º C (100.4 °F) sustained for more than 1 hour in a patient with neutropenia. Appropriate risk assessment should be done to determine the method of administration of empiric therapy (oral vs IV), duration of antibiotic therapy, and determination of inpatient versus outpatient management.
At the onset of fever, all patients underwent vital signs assessment, complete physical examination, with special focus on skin, mucous membranes, nasal sinuses, site of intravenous access, and peri-anal region. blood culture from the peripheral blood and from central line if present was done in all patients, swab cultures were performed in cases with infected wound.
Computer tomography (CT) of the chest was done on day one in patients with chest symptoms or on day 3 with uncontrolled fever, CT of paranasal sinuses (PNS) was requested in case of pain or tenderness over sinuses, serial galactomannan (GM) test was requested in cases with uncontrolled fever on day 3-5 or suspected invasive fungal infection (IFI). Polymerase chain reaction analysis (PCR) of bacteria and fungi from the blood and or Broncho-alveolar lavage (BAL) were performed whenever possible in patients with persistent fever more than 7 days. All patients were analyzed with respect to their demographic profile, results of different diagnostic methods (blood culture, CT scans, GM test, BAL, PCR for sepsis). Also we analyzed the response to different lines of antibacterial and antifungal agent in addition to risk factors mortality.
All patients started immediate empirical antibiotics within maximum one hour of the onset of fever; 123 patients started 3rd generation cephalosporin (ceftazidime or cefepime) and prophylactic antifungal, if the patients were hemodynamically unstable; carbapenems (Imipenem) were given as first line. It was given in 12 cases. With persistent neutropenia after 3 days; empirical antifungal was added (Amphotericin B). The antibiotics or the antifungal could be changed based on the clinical response and the result of blood cultures and suspected organism.
Statistical Analysis
Descriptive statistical analysis was carried out to assess the patients’ demographics and clinical characteristics. The comparison between the 2 groups and the response was assessed using the Chi-square test. Univariate analysis using Cox regression module was performed to test the power of relation between variables. Differences were considered significant if p value was less than 0.05. All analyses were performed using SPSS statistical software (version 20.0).
Results
One hundred and thirty-five (135) patients were identified and analyzed. The mean age was 38.5 years (range 18-76). 86 patients were males and 49 were females. The predominant diagnosis (51%) was acute myeloid leukemia (AML), followed by acute lymphoblastic leukemia (ALL) (36%). Baseline patient’s characteristics are summarized in (Table 1). According to MASCC scoring index, 80 patients (60%) were categorized as high MASCC score (<21), while 55 (40%) had low MASCC score ( ≥21).
Table 1: Baseline patients characteristics.
| Variable | Number | Percentage |
|---|---|---|
Age (years) |
18-76 |
|
Gender |
86 |
64 |
Co-morbidity : DM |
16 |
12 |
Diagnosis AML |
69 |
51 |
MASCC |
80 |
60 |
DM: Diabetes Mellitus, AML: Acute Myeloid leukemia, ALL: Acute Lymphoblastic Leukemia, NHL: Non Hodgkin lymphoma, CLL: Chronic lymphocytic leukemia , MM: Multiple Myleoma, MASCC: multinational association for supportive care in cancer.
Results of different diagnostic modalities
In the present study, the majority of cases (n=114, 84%) had negative blood culture, while only 16% (n=21) had positive culture, gram-negative bacteria constituted 60% of cases, while gram-positive were 40%. The most common gram negative organisms detected by blood cultures were pseudomonas aeruginosa (60 %) followed by Escherichia coli (E. coli) in 40%. Coagulase negative staphylococci (CoNS), methicillin resistant staphylococcus aureus (MRSA), staphylococcus aureus and non-hemolytic streptococci represented the gram positive bacteria encountered in our study, and were detected in 50%, 20%, 20%, 10% respectively. Swab culture was requested in 15 cases only, MRSA was diagnosed in 8 cases with central venous catheter infection, while klebsiella and E. coli were detected form infected wounds in 4 and 3 patients respectively. CT scanning of the chest was done for all patients (n=135), 106 (78%) cases had normal CT findings, while 19 cases (14%) had radiological signs of bacterial infection, eight (6%) and 2 (2%) of patients had radiological signs of fungal infection and pneumocystis pneumonia (PCP) respectively. CT of PNS was performed in 21 (16%) of patients, only 5 cases had radiological signs of fungal infection, while the rest of cases were normal. Serial GM test was requested in 85 cases (63%), only 24 (28%) were positive /rising titre, BAL was performed in 13 patients, only two had positive cultures, the first was positive for pseudomonas aeuroginosa, and the second was positive for mixed candida non-albicans, aspergillus flavus and acinetobacter. PCR for sepsis was done in 5 patients, with only 1case had positive culture for mixed staphylococcus aureus and klebsiella.
Results of antibiotics and antifungal
Third-generation cephalosporins (ceftazidime or cefepime) were administrated as first line antibiotics in 123 patients (91%), while carbapenems (Imipenem) were used as first line antibiotics in 12 (9%) of patients only. Of those who received cephalosporins, 69 patients (56%) had fever subsided, compared to 54 (44%) whose fever was not controlled and were shifted to carbapenems. The majority (n=9, 75%) of cases who received carbapenems as first line had fever control, while 42 out of 54 cases (78%) of those patients who received carbapenems as second line antibiotics had fever subsided.
MASCC score and detection of the organism were the only 2 factors that have significant impact on control of fever with the use of first line antibiotics (Table 2).
Table 2: Factors affecting response to first line antibiotic.
Variable |
Number |
% |
Number of pts received antifungal (52) |
P-value |
|---|---|---|---|---|
Diagnosis AML cases |
69 |
51 |
37 |
0.07
|
MASCC: |
55 |
40 |
24 |
0.001 |
G-CSF usage |
48 |
35 |
21 |
0.001 |
Vancomycin was added to cephalosporins or carbapenems in 34 (25%) of patients with 16 (47%) achieved fever control. The reasons of using vancomycin were documented MRSA in 8 patients, suspected pneumonia in 19 patients, and hemodynamic instability in 7 cases. Linezolid was given in cases of vancomycin intolerance (5 cases).
Fluconazole was used as antifungal prophylaxis in the majority of patients (n=95) (71%), 37 patients (39%) required antifungal therapy. Invasive fungal infections were classified according to 2008 European organization for research and treatment of cancer/invasive fungal infections cooperative group and the national institute of allergy and infectious diseases mycoses study group (EORTC/MSG) Consensus [8].
Probable, possible and proven fungal infections were diagnosed in 12 patient compared to patients for those who did not receive fluconazole prophylaxis compared to those who received it respectively. Among whole patients set, 52 patients received one line of antifungal therapy; 30 patients received amphotericin B, while 22 patients had voriconazole, fever was controlled in 20 patients compared to 14 who received amphotericin B and voriconazole respectively. Change to second line antifungal due to uncontrolled fever was required in 18 patients, voriconazole was administered as second line in 15, while caspofungin was given in 3 patients. With respect to antifungal, only MASCC score and G.CSF use have shown a significant impact on fever control (Table 3).
Table 3: Factors affecting the response to antifungals.
| Variable | Number | Percentage | P value |
|---|---|---|---|
| Diagnosis AML Others † |
69 66 |
51 49 |
0.09 |
| DM Yes No |
16 119 |
12 88 |
0.06 |
| MASCC Low High |
55 80 |
40 60 |
0.001 |
| Type of antibiotics used
Cephalosporins Carbapenems |
123 12 |
91 19 |
0.07 |
| Organism detected
Detected Not detected |
39 96 |
29 71 |
0.04 |
| G-CSF use Used Not used |
48 87 |
35 65 |
0.09 |
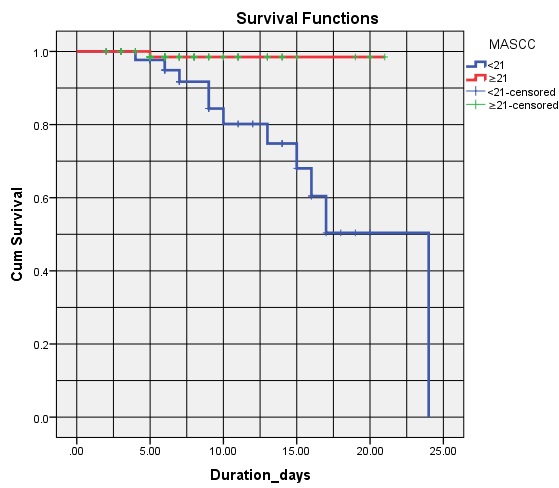
Prolonged FN (>7days) was observed in 54 patients (40%), the use of corticosteroids, and non-administration of G-CSF were the predominant risk factors (P<0.001, P<0.002) respectively. In terms of mortality, only patients with high MASCC score (n=11) (8%) had the worst outcome compared to low score (n=1) (P<0.0001) (Figure 1).
Figure 1: Survival of patients according to MASCC score.
Discussion
It is important to assess the risk of serious complications in patients with neutropenic fever, since this assessment will determine the approach to therapy, including the need for inpatient admission, intravenous antibiotics, and prolonged hospitalization. The IDSA [4] and ASCO [6] defined high-risk neutropenic patients as those with an ANC ≤ 100 cells/ μ L expected to last >7 days or evidence of ongoing comorbid conditions or significant hepatic or renal dysfunction.
The NCCN has developed similar criteria but also includes an intermediate risk category [8]. In the current analysis, we studied patients with hematological malignancies who developed FN during their management, aiming to look for the factors that could be associated with uncontrolled fever on antibiotics or antifungals.
The source of infection is identified in approximately 20 to 30% of febrile neutropenic episodes, often the only evidence of infection is bacteremia, which is documented in 10 to 25% of patients [9]. In our study, 39 out of 135 patients (28.8%) had documented pathogen 21 had positive blood culture, 15 had swab culture, 2 had positive BAL and 1 case had rising PCR.
Gram-negative bacilli, particularly pseudomonas aeruginosa, were the most commonly identified pathogens in neutropenic patients until the 1980s [10], subsequently, gram-positive bacteria have become the most common pathogens. A number of changes in practice likely account for the trend toward gram-positive infections, including the introduction of central venous catheters, the use of prophylactic antimicrobials that are primarily active against gram-negative pathogenens [11,12].
Gram negative bacteria was more common in our analysis, perhaps due to low number of cases who had indwelling catheters, recent data showed a trend back toward gramnegative bacteria, with the emergence of antibiotic-resistant gram-negative strains despite fluoroquinolone prophylaxis, however, the ratio of gram-positive to gram-negative bacteria as the cause of bacteremia in cancer patients remains at approximately 60: 40 [13].
Although the majority of requested CT scans were normal, we should keep low threshold to order CT scan. Real-time PCR assay in combination with blood culture could improve microbiological documentation of FN, the few number of patients (n=5) who had PCR in our study is explained by the high cost [14].
Another study showed comparable outcome between ceftazidime, and meropenem for clinically defined and microbiologically defined infections, however, meropenem was significantly more effective than ceftazidime in severely neutropenic (<=100 cells/microliter) patients (55% v 43%, respectively), bone marrow transplant patients (73% v 27%, respectively), and patients given antibiotic prophylaxis before study entry (71% v 52%, respectively) [15]. In another trial there was similar efficacy between cefepime and imipenem, an intent-to-treat analysis showed 68% response rate to the imipenem, compared with a 75% response rate to the cefepime (P-value = 0.2) [16].
In our analysis, 56% of patients did not respond to cephalosporins and were shifted to carbapenems , while most of the cases responded to carbapenems either in the first line or second line (75% and 78% respectively), however univariate analysis showed that only MASCC score and detection of the organism were the only factors that affect response to first line antibiotics (0.001 and 0.04 respectively), choice between cephalosporins and carbapenems had no impact on control of fever (P-value =0.07).
The use of G-CSFs in patients with established fever and neutropenia is controversial [17], ASCO [18] and ESMO [19] guidelines suggest that G-CSF be “considered” for patients at high risk for infection-associated complications or who have prognostic factors that are predictive of a poor clinical outcome. High-risk features include expected prolonged neutropenia (>10 day), age >65, uncontrolled primary disease, pneumonia, hypotension, and multi-organ dysfunction (sepsis syndrome), invasive fungal infection, or being hospitalized at the time of the development of fever. In the current study, G-CSF was used in 35% of patients, there was significant impact on control of fever with the first antifungal therapy but not with first line antibiotics, however, these results should be taken cautiously given small number of patients, and lack of solid evidence from large randomized trials.
The incidence of invasive candidiasis and aspergillus’s in patients with hematologic malignancies has varied widely in different studies, likely due to differences in the underlying disease, the duration of neutropenia, and the types of chemotherapy regimens used. Rates of invasive candidiasis and invasive aspergillus’s have ranged from 8% to 24% [20] and from 2% to 28% respectively [21] In our study, 52 patients received antifungal therapy which represent 38.5 5 of the whole patient’s cohort, this higher incidence could be explained by the fact that almost half of the patients were AML, and 40% had prolonged FN.
Only MASCC score and G.CSF administration had significant impact on the response to first line antifungal treatment (P=0.001 and 0.001 respectively), while prior fluconazole and type of antifungal used had no significant impact on control of fever with the use of first antifungal regimen (0.06 and 0.08 respectively). MASCC index may predict the likelihood of death, high risk and low risk had 38% and 2% risk of mortality respectively, however MASCC score has been criticized due to lack of a standardized definition of “burden of febrile neutropenia,” which might be interpreted differently by different clinicians, another important point is that the index does not include duration of neutropenia as a risk factor [22].
In the present analysis, with respect to mortality, only patients with high MASCC score had significant difference compared to low risk.
Conclusion
There are multiple factors that may affect the outcome of patients with FN and it should be taken in considerations during management of FN such as MASCC score, detection of the organism, previous use of corticosteroid and G-CSF administration during FN.
Conflict of Interest
None.
There are no references