Journal Name: International Journal of Cancer and Treatment
Article Type: Case Report
Received date: 01 August, 2019
Accepted date: 03 October, 2019
Published date: 07 October, 2019
Citation: Kumar HK, Vengadakrishnan P.R, Ganesharaja S (2019) Mucoepidermoid Carcinoma of Tongue Base - A Rare Case Report. Int J Cancer Treat Vol: 2, Issu: 2 (11-14).
Copyright: © 2019 Kumar HK. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Mucoepidermoid carcinoma (MEC) is the most common malignant, locally-invasive tumour of the salivary glands, and accounts for approximately 35% of all malignancies of the major and minor salivary gland. Mucoepidermoid carcinoma of tongue are not common. Presenting a 39-year-old male patient who reported with ulcer in the left lateral border of tongue. Biopsy from the ulcer revealed Mucoepidermoid carcinoma grade II and was staged cT2N0M0. He underwent wide local excision with primary closure. Post-operative histopathology revealed Mucoepidermoid carcinoma- Intermediate grade. He received adjuvant radiation to the post- operative bed TD 60Gy.
Key words: Mucoepidermoid carcinoma, wide local excision, Adjuvant radiation.
Abstract
Mucoepidermoid carcinoma (MEC) is the most common malignant, locally-invasive tumour of the salivary glands, and accounts for approximately 35% of all malignancies of the major and minor salivary gland. Mucoepidermoid carcinoma of tongue are not common. Presenting a 39-year-old male patient who reported with ulcer in the left lateral border of tongue. Biopsy from the ulcer revealed Mucoepidermoid carcinoma grade II and was staged cT2N0M0. He underwent wide local excision with primary closure. Post-operative histopathology revealed Mucoepidermoid carcinoma- Intermediate grade. He received adjuvant radiation to the post- operative bed TD 60Gy.
Key words: Mucoepidermoid carcinoma, wide local excision, Adjuvant radiation.
Introduction
Mucoepidermoid carcinoma (MEC) is the most common malignant, locally-invasive tumour of the salivary glands, and accounts for approximately 35% of all malignancies of the major and minor salivary gland (1a). Mucoepidermoid carcinoma of tongue are not common. Minor salivary glands are scattered in different areas of the oral cavity such as palate, retro molar area, Floor of the mouth, buccal mucosa, lips and tongue. Among patients presenting with intra oral minor salivary gland tumours, 1% of patients present with carcinoma in the tongue. 60% of those presenting with minor salivary gland tumours in tongue are malignant. First case was reported in 1973 (15). MEC of the tongue presents in fifth decade and it is more common in females [1-6].
Over 30-year period, retrospective study of tongue base tumors conducted, total 22 cases were malignant 45% of them diagnosed as MEC [5]. Etiologic factors are not clearly defined. People with low intake of vitamin A and C have high incidence of salivary gland tumours. Cigarette smoking and alcohol consumption in general are not related to salivary gland tumours. But consumption of more than 80 pack year of cigarette smoking may contribute to salivary gland cancers. Prior irradiation is also considered as a risk factor. Investigators have suggested trisomy 5 as a possible precursor event in MEC pathogenesis based on cytogenic studies [7].
The approach to disease management includes a complete physical examination followed by imaging. Treatment strategies are best considered in a multidisciplinary board consultation. The surgical approach should be the first choice followed whenever negative margins are possible and the disease is not disseminated [3]. Depending on the risk assessment or specific lymph nodes involvement adjuvant radiation therapy should be offered within one month. Adjuvant chemotherapy in regional disease could be considered depending on clinical judgment. In cases of disseminated disease, chemotherapy represents first line therapy; the choice of the agents to be taken based on clinical judgment and experience. Prognosis of MEC is a function of the histological grade, adequacy of excision and clinical staging. This rationale has been supported by several other authors who have advocated wide tumor margins as intraoral MEC tends to be more aggressive, with recurrence rate of up to 30%-40% with high-grade lesions [8-14].
Tumours involving the salivary glands represent a diverse group. With the better understanding of pathological processes and the use of IHC and gene translocation studies, there have been changes in the nomenclature of salivary gland pathology. The current WHO classification does not take into account the recent tumour types and is being revised [4]. Here we present a case of Mucoepidermoid carcinoma of base of tongue.
A 39 years old male who is a known tobacco chewer and alcoholic presented with ulcer in the left lateral border of tongue which was extending from the level of left lower 1st molar up to the posterior third of the tongue measuring 2.5x2.5cm. Examination of the neck revealed left level IB sub-centimetric soft node. Patient had no comorbidities. Biopsy was performed and reported as Mucoepidermoid carcinoma grade II.
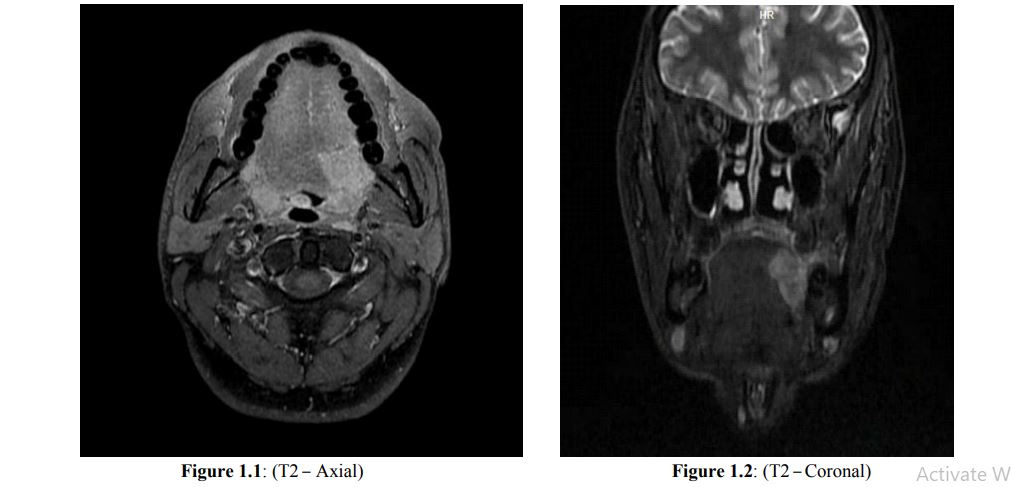
MRI scan showed hyper intense area with good contrast enhancement seen involving the left side of tongue involving posterior third of tongue and adjacent posterior aspect of anterior two thirds of tongue measuring 2.1x1.8x2.3cm in T2 Sequence (Figure1.1 & 1.2). Lesion extends up to midline but does not cross the midline.
Patient was diagnosed as non-metastatic Mucoepidermoid carcinoma of tongue cT2N0M0. Based on these clinic-radiological findings, history and pathological findings, he was planned for wide local excision of the lesion after multi-disciplinary board discussion.
Surgery
Under general anaesthesia patient underwent wide excision of the left lateral tongue and tissue sent for frozen section. Frozen section showed all margins negative for tumour. Additional deep margins were taken and wound was closed with primary closure. Neck Node dissection was deferred as Lymph nodes metastasis are not common in (MEC) and there were no clinically significant nodes cervical nodes on deep palpation.
Post-op histopathology showed 4x3x2cm specimen showing sub mucosal nodule measuring 2x1.8x1cm showing features suggestive of Mucoepidermoid carcinoma intermediate grade with depth of invasion of 6mm and deeper clearance from inked margin 1mm. Additional deep margin free of tumour. Pathologically staged as pT2Nx.
Case was discussed extensively in multi-specialty board and planned for adjuvant radiation. Although adjuvant radiation is indicated only for high grade tumours, it was considered in this case because in the event of a recurrence the chance of salvage surgery may be difficult and with adjuvant radiation better local control can be achieved.
Adjuvant Radiation
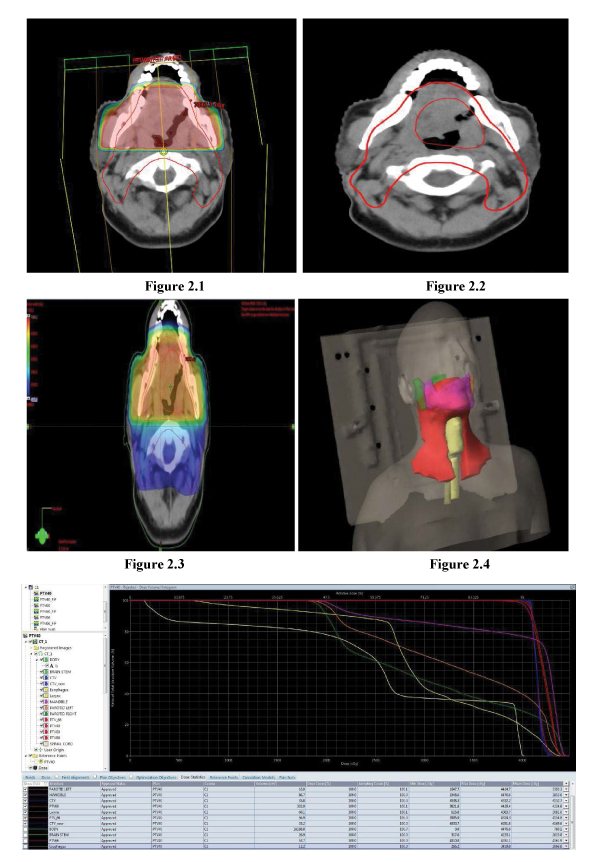
Planning CT scan was done with proper immobilization using thermoplastic mould. 5mm cuts axial CT scan was taken from vertex till carina level. Images were transferred to Varian planning system and image registration with MRI scan. The Post op bed was defined and Clinical Target Volume (CTV) was generated by 1cm margin to Post op bed. Planning Target Volume (PTV) was generated by 1cm margin to CTV. Using 3d conformal technique, he received total dose of 66Gy RT to high risk PTV (Figure2.1) which includes post op bed and probable nodal regions and 60 Gy RT to intermediate risk PTV (Figure.2.2) over a period of 6 weeks. Dose colour wash and 3D view of dose distribution are depicted in (Figure 2.3 & Figure 2.4). Cumulative dose distribution of all OAR’s and all PTV (Low /Intermediate/ High) are shown in Figure 2.5.
Figure2.5: DVH – Dose Distribution
Discussion
MEC of the minor salivary glands is composed histologically of three cell types - mucous cells, epidermoid squamous cells and poorly differentiated intermediate cells that have the ability to differentiate into either mucous producing or epidermoid cells [13]. When the epidermoid element predominates, the histological appearance of the tumour may closely resemble that of squamous cell carcinoma on histological examination, and it is thus classified as a high-grade MEC tumour. The presence of mucin-producing cells within a predominantly cystic architecture is regarded as low-grade MEC tumour. Intermediate- grade tumours are less cystic and show a greater tendency to form large, more irregular nests or sheets of squamous cells and often have a more prominent intermediate cell population.
Diffuse staining with either p63 or CK5/6 is highly specific for MECs. The level of expression of both p63 and CK5/6 varies according to the grade of the tumor. Greater proportion of intermediate and high grade MECs have 3+ to 4+ expression of these markers than the low grade tumors.
The treatment of choice for MECs of minor salivary glands with low to intermediate-grade is a radical surgery alone by wide local excision intraoral, if it can be achieved, with adequate tumour-free margins. High-grade tumours require more aggressive surgery with or without postoperative radiotherapy and chemotherapy [13]. The methods of surgical removal of neoplasm of base of the tongue include Trans mandibular and/or Trans cervical approaches and an intraoral route.
Patients often develop local or regional recurrence and distant metastases. Metastasis is primarily to subcutaneous tissues, lymph nodes, bone and lung. Generally, lymphatic spread can be common in high-grade MEC. Previously, highgrade MEC has been associated with poorer regional control because it frequently infiltrates surrounding structures, recurs, or metastases. Management of the neck and the need to assess it during long-term follow-up of MEC has been emphasised. Neck dissection is not indicated for patients with low grade mucoepidermoid carcinoma.
Adjuvant radiotherapy (RT) is recommended for highgrade tumours. We believe that post-operative radiotherapy should be given to patients with high-grade tumours and in those invading or in close resection margins, lymph node metastases, perineural or lymphovascular invasion or both. Treatment with chemotherapy is indicated for patients with metastatic disease and those who are not candidates for salvage surgery or RT. It is generally accepted that, for highgrade MECs, radiotherapy combined with surgery should achieve local control of the disease and good survival rates.
Conclusion
MECs are rare tumours of the salivary glands. No specific guidelines have evolved for the management of these tumours, but surgical excision is mandatory along with a long-term follow-up. In particular, low and intermediate grade MECs of salivary glands tend to have a favourable outcome compared with high-grade MECs that have a greater tendency to recur and metastasize. The clinical stage continues to be both a prognostic factor for overall survival and a predictive factor of distant metastases. Therefore, both correct clinical staging and immunohistochemical findings associated with careful follow-up are important factors in minor salivary gland malignancies, especially high-grade MECs, for appropriate management of these tumours.
Mesolella M, Iengo M, Testa D, A M Di Lullo, G Salzano, et al. (2015) Mucoepidermoid carcinoma of the base of tongue. Acta Otorhinolaryngol Ital 35: 58-61.[ Ref ]
Leong S, Pinder E, Sasae R, Mortimore S (2007) Mucoepidermoid carcinoma of the tongue. Singapore Med J 48: e272-e274.[ Ref ]
Craig Bollig BS, Laura C Huang BA, Ralph Abi-Hachem MD, Oleksandr N. Kryvenko MD, Jason M. Leibowitz (2015) Base of tongue mass. JAMA Otolaryngol Head Neck Surg 141: 935-936.[ Ref ]
Badlani J, Gupta R, Balasubramanian D, Smith J, Luk P, et al. (2018) Primary salivary gland malignancies: a review of clinicopathological evolution, molecular mechanisms and management. ANZ J Surg 88: 152- 157[ Ref ]
Heidelberger KP, Batsakis JG (1973) Mucoepidermoid carcinoma of the tongue. The Journal of Laryngology & Otology 87: 1239-1242.[ Ref ]
de Vries EJ, Johnson JT, Myers EN, Barnes EL Jr, Mandell-Brown M (1987) Base of tongue salivary gland tumors. Head Neck Surg 9: 329-331.[ Ref ]
Gold blatt LI, Ellis GL (1987) Salivary gland tumors of the tongue. Analysis of 55 new cases and review of the literature. Cancer 60: 74-81.[ Ref ]
el-Naggar AK, Lovell M, Killary A, Batsakis JG (1994) Trisomy 5 as the sole chromosomal abnormality in a primary mucoepidermoid carcinoma of the minor salivary gland. Cancer Genetics and Cytogenetics 76: 96-99.[ Ref ]
Bradley PJ (2001) Distant metastases from salivary glands cancer. ORL J Otorhinolaryngol Relat Spec 63: 233-242.[ Ref ]
Cardoso WP, Denardin OV, Rapoport A, Araujo VC, Carvalho MB (2000) Proliferating cell nuclear antigen expression in Mucoepidermoid carcinoma of salivary glands. Sao Paulo Med J 118: 69-74.[ Ref ]
Auclair PL, Goode RK, Ellis GL (1992) Mucoepidermoid carcinoma of intraoral salivary glands. Evaluation and application of grading criteria in 143 cases. Cancer 69: 2021-2030.[ Ref ]
Eversole LR (1970) Mucoepidermoid carcinoma: review of 815 reported cases. J Oral Surg 28: 490-494.[ Ref ]
Eversole LR, Rovin S, Sabes WR (1972) Mucoepidermoid carcinoma of minor salivary glands: report of 17 cases with follow-up. J Oral Surg 30: 107-112. [ Ref ]
Williams JD, Agrawal A, Wakely PE (2003) Mucoepidermoid carcinoma of the lacrimal sac. Annals of Diagnostic Pathology 7: 31-34.[ Ref ]