Journal Name: International Journal of Cancer and Treatment
Article Type: Research
Received date: 25 October, 2019
Accepted date: 22 November, 2019
Published date: 27 November, 2019
Citation: Sayed SAM, Aabdin AM, Abo-Shanab MAA, Noma M (2019) Prevalence of NCDS and Their Risk Factors in Khartoum State, Sudan. Int J Cancer Treat Vol: 2, Issu: 2 (52-63)
Copyright: © 2019 Sayed SAM. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Objectives: The objective of this study is to determine the prevalence and risk factors associated with Non-communicable diseases in two administrative units of Khartoum State, Sudan. (prevalence of risk factor for NCDs will change the meaning, we determine the prevalence of NCDs and then the prevalence of their risk factors).
Methods: A cross-sectional study was conducted in two administrative units of Khartoum State between December 2018 and March 2019, among 132 participants selected using multi-stage sampling technique.
Results: Our findings revealed that NCDs prevalence of 24/100,000 population. Of the fifteen risk factors associated to NCDs in the two administrative units, seven were statistically associated (p < 0.05) to NCDs, and were age and gender of the participants, the participants’ profession, educational level, physical activities, follow-up visits and having meals outside home.
Conclusion: In conclusion NCDs were public health priorities with particular attention to diabetes and hypertension to avoid premature deaths.
Keywords: Diabetes mellitus, Hypertension, Non-communicable diseases, Prevalence, Risk Factors.0
Abstract
Objectives: The objective of this study is to determine the prevalence and risk factors associated with Non-communicable diseases in two administrative units of Khartoum State, Sudan. (prevalence of risk factor for NCDs will change the meaning, we determine the prevalence of NCDs and then the prevalence of their risk factors).
Methods: A cross-sectional study was conducted in two administrative units of Khartoum State between December 2018 and March 2019, among 132 participants selected using multi-stage sampling technique.
Results: Our findings revealed that NCDs prevalence of 24/100,000 population. Of the fifteen risk factors associated to NCDs in the two administrative units, seven were statistically associated (p < 0.05) to NCDs, and were age and gender of the participants, the participants’ profession, educational level, physical activities, follow-up visits and having meals outside home.
Conclusion: In conclusion NCDs were public health priorities with particular attention to diabetes and hypertension to avoid premature deaths.
Keywords: Diabetes mellitus, Hypertension, Non-communicable diseases, Prevalence, Risk Factors.0
Introduction
According to World Health Organization (WHO), Non-communicable diseases (NCDs) also, are multifactorial including genetic, physiological, environmental and behavioral factors [1]. 41 million deaths worldwide occurred yearly due to NCDs of which 15 million between 30 to 69 years; over 85% of these premature deaths occurred in low- and middle-income countries. The four leading killers accounting for 80% of all premature NCD deaths were cardiovascular diseases (17.9 million death/year), cancers (9.0 million), respiratory diseases (3.9 million), and diabetes (1.6 million). The risk of dying from NCDs increases with tobacco use, physical inactivity, the harmful use of alcohol and unhealthy diets. Due to the high importance of NCDs in the sustainable development, the WHO goal 3 related to health, includes a target of one third reduction of premature mortality from NCDs by 2030 [1]. This tremendous challenge require national policies framed within effective, cost effective affordable and feasible interventions.
Regarding the socioeconomic impact of NCDs, there is a close relation between poverty and NCDs. People at lower socioeconomic position get sicker and die earlier than people at higher social class. This is due to many reasons such as improper diet and poor access to health services [2]. A systematic analysis carried on age-sex specific mortality for 282 causes of death in 195 countries and territories revealed that non-communicable diseases, as a leading cause of deaths, contributed by 73.4% to the total deaths in 2017 [3].
In Sudan, the proportional mortality rate ranked cardiovascular diseases as first accounting for 28% of the total deaths, followed by cancers (6%), chronic respiratory diseases (3%) and diabetes (2%). Overall, NCDs in Sudan account for 52% of all deaths. The risk of premature death between 30-70 years in Sudan was reported to 26% with a gender variation between males (28%) and females 24% [4].
In Sudan, published articles [5, 6] revealed a prevalence of hypertension ranging from 27.6% to 35.7%. Abdalla EAM et al. reported that diabetes mellitus among 236 adults was 18.6% with no significant gender difference in the prevalence rate [7].
A multi-country longitudinal study on aging and health [8] revealed a high prevalence of hypertension in all countries (China, Ghana, India, Mexico, Russia and South Africa) ranging from 14.1% in Ghana to 40.8% in Russia. Followed by self-reported arthritis with a prevalence ranging from 7% in Mexico to 27.2% in Russia. The prevalence of selfreported asthma was 7.7% in India, whereas in the remaining countries the prevalence was < 5%. The prevalence of both self- reported and algorithm based chronic lung diseases were lowest in Ghana 0.5% and 3% respectively, and highest in Russia 13.7% and 21.4% respectively. The adjusted prevalence of self- reported depression varied from 0.3% in China to 13.9% in Mexico. Whereas, the algorithm based indicated a low prevalence of depression in China (2.1%) and a high prevalence in India (18.5%).
Population-based cross-sectional study conducted in Brazil revealed that the prevalence of having at least one chronic disease is 45.1% in the age group of ≥ 18 years [9], while in adults aged ≥ 35 years the reported prevalence of NCDs is 22.8% varying from 22.0% in urban areas to 24.0% in rural settings [10]. In those aged ≥ 60 years, an overall prevalence of NCDs of 31.7% was published [11]. Of the four NCDs of concerned were; hypertension ranked first (26.0%), followed by diabetes mellitus (8.0%), stroke (1.9%) and chronic obstructive pulmonary disease (COPD, 1.0%). In India, NCDs accounted for 60% of all deaths which represented one third of the total deaths as confirmed by an Indian author who reported a prevalence of NCDs of 29.0% [12,13].
NCDs remain a challenge even in displaced populations. A 2015 study [14] on thirteen displaced camps in Kurdistan Region of Iraq involved 8360 participants. The results revealed that one-third of households interviewed had at least one member who had one or more of the four common NCDs which are: hypertension (19.4%), musculoskeletal conditions (13.5%), Diabetes mellitus (9.7%) and cardiovascular disease (CVD, 6.3%). In another study involving non-camp Syrian refugees aged ≥ 18 years, Rehl et al. found that 21.8% of study population suffered from at least one NCD and 44.7% reported NCD co-morbidities; Hypertension and diabetes prevalence were respectively 14.0% and 9.2% [15]. The prevalence of NCDs and use of health services was implemented in Gaza Strip on a sample of 760 households totalizing 5192 individuals; the findings revealed that 12.7% of the participants harbored at least one NCD [16].
The African continent also paid tribute to NCDs. WHONon communicable Diseases (NCDs) Country profiles of 2018 reported that for all deaths in Nigeria and Uganda 29 and 33 people out of 100 lost their lives because of NCDs [4]. A population-based cross-sectional survey using WHO STEPS survey instrument indicated that in Tanzania the prevalence of hypertension ranged from 16.0% to 17.0%, whereas in Uganda it ranged between 19.0% and 26.0%. In both countries’ hypertension was more prevalent in urban than in rural population. The prevalence of diabetes mellitus (DM) and other NCDs was low with a prevalence of 1 to 4% for DM [17, 18]. The Malawi National NCDI Poverty Commission reported that in 2017, diabetes, cardiovascular diseases, cancer, and chronic lung diseases account for 38% of the NCDs burden. These findings were consolidated in 2018 review which revealed that the prevalence of cardiovascular diseases was 8.9%, asthma prevalence was 5.0% and the prevalence of diabetes ranged between 2.3% and 5.7% and all types of cancers incidence rate was 156 cases/100,000 population [19, 20]. In the Democratic Republic of Congo, Mawaw P M et al [21] showed that the prevalent NCDs were hypertension (18.2%), diabetes (11.7%) and cardiovascular diseases (3.2%). A study conducted in Ethiopia revealed that the reason for the visits due to NCDs represented 29.7% of the records. The prevalence of cardiovascular diseases was 18.8% and of diabetes mellitus 13.1% [22]. A systematic review [23] of five hospital-based studies from eastern Ethiopia revealed a prevalence of CVD was 7.2% and 2.4% for hypertensive heart diseases among all age groups.
The risk factors associated to non-communicable disease are multifactorial. Ahmed Reza Hosseinpoor et al. reviewed 2002-04 World health survey Data from the 41 countries that had available data about NCD risk factors, and relevant socioeconomic and demographic variables. Their findings showed that angina, asthma, arthritis and depression prevalence were inversely associated to wealth and education, on the contrary the prevalence of diabetes showed a strong association with wealth and education [24].
A meta-analysis analysis in Japan estimated the excess risks on deaths and life expectancy based on data from the National Health and Nutrition Survey and epidemiological studies. The findings revealed that tobacco smoking accounted for 29,000 deaths [95% CI: 115,000-154,000], high blood pressure 104,000 deaths (95% CI: 86,000- 119,000) and physical inactivity 52,000 deaths, [95% CI: 47,000-58,000] [25].
A cross-sectional study from India revealed that the prevalence of daily smoking was respectively 6.6% in urban and 12.29% in rural participants. The prevalence of low physical activity of 38.9% in urban participants was lower (14.2%) in rural; the prevalence of low fruit and vegetables consumption in urban area was 92.7% and 96.4% in rural area. The prevalence of raised blood pressure in urban and rural areas were 29.1% and 15.4% respectively [26]. Another cross-sectional study in Ibadan (Nigeria) using the WHO Stepwise approach [27] to assess the risk factors of NCDs among 606 civil servants indicated that the prevalence of smoking, harmful use of alcohol, low physical activity, insufficient fruit and vegetables intake, obesity were respectively 6.5%, 7.8%, 62.2%, 69.7%, 57.3%. In the same country, Agaba EL et al. implemented a survey of non-communicable diseases and their risk factors among university employees by using WHO Stepwise approach [28]. Of 883 participants of the University of Jos (Nigeria), the most common NCD risk factors reported were inadequate intake of fruit and vegetables (94.6%), physical inactivity (77.8%), obesity (26.7%), alcohol use (24.0%) and cigarette smoking (2.9%).
In Sudan, Ghebreselasie D.T. [29] reported the prevalence of smoking in males of 18.4% and 0.3% in females; alcohol consumption in males was 3.9%, physical inactivity in both genders was 75.0% and adequate consumption of fruits and vegetables was prevalent in 72.9% of the study population. History of NCDs was statistically associated (p < 0.05) to cigarette/tobacco use, as well as physical activity and educational level with a p-value of respectively 0.003 and 0.011.
Our study attempted determine the prevalence and risk factors associated with non-communicable diseases in two administrative units (Alshohada/Soba and Al Jabal) of Khartoum State.
Materials and Methods
Participants:
A community-based cross-sectional study was conducted. The research was implemented in two administrative units of Khartoum State, namely “Alshohada & Soba” and “Al Jabal” with a total population of 552,955 people, 51.1% are living in “Alshohada & Soba” and 48.9% in “Al Jabal “as per Sudan Census Bureau of Statistics (http://cbs.gov.sd/). The population of “Alshohada & Soba” is distributed in 33,608 households and 270,662 inhabitants of “Al Jabal” live in a total of 32,537 households.
Sample size and sampling techniques
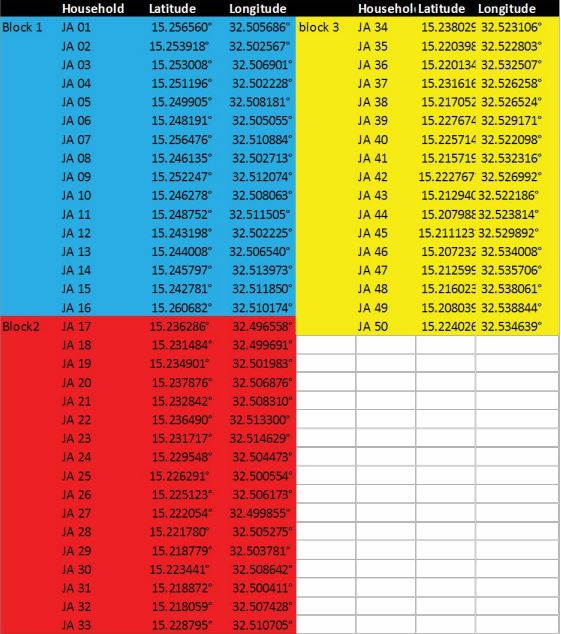
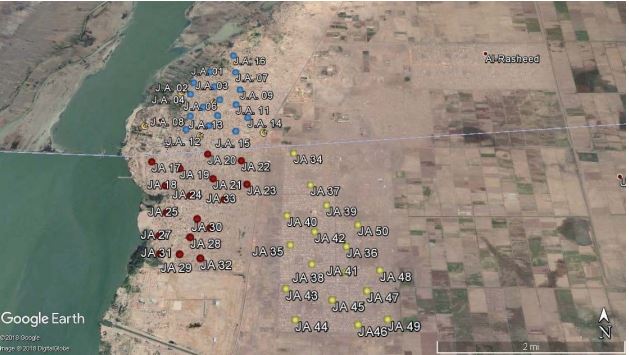
A multistage sampling technique was used to select the study participants.
Dose response model divided into four types- LinearQuadratic Model, Generalized Equivalent Uniform Dose, TCP Models, NTCP Models.
Liner Quadratic model
1. At first level the two localities (administrative level 2) which administratively constitute Khartoum were all included in the study. Al Khartoum locality comprise six administrative units, one administrative unit “Alshohada & Soba” was randomly selected. In “Jabal Awliya” locality divided in four administrative units, Al Jabal (with urban and rural mode of living) was selected.
2. At second level, in each of the two selected administrative units, 50 households spatially distributed were included in the study under the assumption that in every one of the households selected one case of NCD will be available. When no case of NCD was found in a selected household, it was systematically replaced by the nearest household. This led to an estimated sample size of at least 100 participants (50 households x 2 administrative units).
3. At third level, in each of the household selected participants experiencing at least one NCD were included in the study after obtaining his/her verbal well informed consent.
Inclusion and exclusion criteria
• Were included in the study, the residents of “Alshohada & Soba” and “Al Jabal” harboring a non-communicable disease, regardless their gender and age; for the participants below < 15 years the questionnaire was addressed by the care giver present at the time of the data collection.
• Were excluded from the all residents from other administrative units of Khartoum State and the residents of the two selected administrative units who refused to participate in the study.
Data Collection and analysis
A standardized interviewer-administrated questionnaire, pre-tested, primarily developed in English, was administrated in Arabic by the researcher. The data collected included the socio-demographic characteristics of the study participants (age, gender, residence, occupation, household size), the type of NCD, its duration, comorbidity and factors associated to the NCD including the lifestyle of the participants and the management of the NCD.
The data collected were computerized through a template developed in Epi-Info7 and analyzed through the statistical package for social sciences (SPSS 23). The data were summarized numerically (mean, standard deviation, median) and graphically (frequency tables for estimating prevalence and graphics). Association between categorical variables were through chi-square tests (Pearson Chisquare, Fischer Exact Test and Likelihood Ratio). A multilogistic regression analysis was performed to assess the relationship between NCDs and its related risk factors. All statistical tests were considered as statistically significant when p < 0.05.
Results
Characteristics of the study participants
This research was conducted in two administrative units of Khartoum State. 54.5% (72/132) of the participants lived in Alshohada & Soba and the remaining 45.5% (60/132) where from Al Jabal. Females were predominant (55.3%, 73/132). The age of the participants ranged from 4 to 90 years with a median age of 56.5 years. 70.8% (92/132) of the participants were married; 44.7% (59/132) were housewives, 37.9% (50/132) were working and 17.4% (32/132) were not. 86.2% (112/130) were educated and the remaining 13.8% (18/130) did not attend a school. Their respective household size varied from 2 to 14 members with a median of 6 members.
Table 1: Prevalence (case/100000 population) of NCDs in Alshohada & Soba and Al Jabal (n=132).
| Non-communicable disease | Number and prevalence of NCDs per administrative unit | |||||
|---|---|---|---|---|---|---|
| Alshohada & Soba | Prev* | Al Jabal | Prev | Total | Prev | |
| Diabetes mellitus | 22 | 7.79 | 22 | 8.13 | 44 | 7.96 |
| Hypertension | 16 | 5.67 | 15 | 5.54 | 31 | 5.61 |
| Diabetes & Hypertension | 19 | 6.73 | 9 | 3.33 | 28 | 5.06 |
| Asthma | 2 | 0.71 | 6 | 2.22 | 8 | 1.45 |
| Diabetes mellitus & Cardiovascular disease | 4 | 1.42 | 0 | 0.00 | 4 | 0.72 |
| Diabetes mellitus & Cardiovascular disease & Hypertension | 2 | 0.71 | 2 | 0.74 | 4 | 0.72 |
| Cardiovascular disease | 2 | 0.71 | 1 | 0.37 | 3 | 0.54 |
| Osteoarthritis | 0 | 0.00 | 3 | 1.11 | 3 | 0.54 |
| Cancer | 1 | 0.35 | 1 | 0.37 | 2 | 0.36 |
| Rheumatoid Arthritis | 1 | 0.35 | 1 | 0.37 | 2 | 0.36 |
| Hyperthyroidism | 1 | 0.35 | 1 | 0.00 | 1 | 0.18 |
| Hyperthyroidism | 1 | 0.35 | 1 | 0.00 | 1 | 0.18 |
| Cardiovascular disease & Hypertension | 1 | 0.35 | 1 | 0.00 | 1 | 0.18 |
| Total | 72 | 26 | 60 | 22 | 132 | 24 |
*Prevalence calculated as number of cases of NCDs divided by 100,000 total population.
Distribution and prevalence of non-communicable diseases (NCDs) in two localities of Khartoum State
Chronic Diseases reported by the study population
The two most frequent NCDs reported were Diabetes mellitus and Hypertension affecting respectively 33.0% (44/132) and 23.5% (31/132) of the participants. 21.1% (28/132) of participants with diabetes also had hypertension. 22.1% (29/132) suffered from one single NCD or at least one comorbid disease.
Prevalence of non-communicable diseases Alshohada & Soba and Al Jabal
The overall prevalence of the NCDs in the two administrative units surveyed was 24/100,000 population. It ranged from 22/100000 population in “Al Jabal” to 26/100000 population in “Al shohada and Soba”.
Diabetes Mellitus was the most prevalent (8/100000) NCD in the two administrative units. This prevalence was the same in “Al shohada & Soba: and “Al Jabal” with a prevalence of respectively 7.79/100,000 and 8.13/100,000 (table 1).
Hypertension ranked second in term of prevalence, it affected 6 persons per 100,000 population. This burden is equal in the two administrative units.
Twenty-eight participants reported comorbid diabetes mellitus and hypertension, this represented an average of 5 per 100,000 total population. This average varied across the two administrative units with 7 persons affected out of 100,000 population in “Alshohada & Soba” and 3 persons/100,000 in “Al Jabal.”
Risk factors associated with Non-Communicable Diseases.
Practices of the study participants towards treatment and follow-up for NCDs
Adherence to treatment by the study participants
Of 132 participants, the majority (93.9%, 124/132) replied that they were under treatment, with higher percentage (97.2%) in Alshohada & Soba compared to Al Jabal (90.0%), with no statistical significance (p=0.14). Most (72.6%, 90/124) of the participants were under treatment for more than 5 years and only 8.1% (10/124) were under treatment for less than 1 year. 19.4% (24/124) of those were under treatment between 1-4 years. The participants were asked to provide the type of treatment they were using. The question offered three options which were namely medical, traditional herbal medicine or combined treatment. 91.9% (114/124) of the participants were under medical treatment and the remaining 8.1% (10/124) were under combined treatment (medical and traditional). In “Alshohada & Soba” 54.4% and 80.0% of the participants were respectively under medical and combined treatment; whereas in “Al Jabal” those under medical treatment or combined were respectively 45.6% and 20.0%. The differences recorded between the two administrative units and the type of treatment were not statistically significant (p=0.107); this indicated that the type of treatment was equally used in both administrative units.
Anti-diabetic and hypertensive drugs were the most frequently used by the participants with respectively 63.7% (79/124) and 51.6% (64/124). 19.4% (24/124) of the participants were under other medications such as chemotherapy, carbimazole, statin, salbutamol, thyroxin, warfarin, and vitamins.
The participants were asked to address the question related to the adherence to treatment. Firstly 52.4% (65/124) reported to have forgotten at least once to take his/her treatment and 47.6% (59/124) had never forgotten to take it. Secondarily, 76.6% (95/124) of the participants were taking always their treatment as prescribed by their treating doctor.
(76.6% of the participants take their treatment regularly as prescribed by their treating doctors, for example they did not increase or reduce the doses)
Adherence to follow up as prescribed by the treating doctor
The participants were asked if “they have a regular follow up visit for their condition by their treating Doctor”. More than half (52.3%, 69/132) always had regular visits, 9.8% (13/132) never visit their treating physician for follow -up and 37.9% (50/132) visited their treating doctor only when necessary (Only when they feel the need and /or suffered from their condition).
Sixty participants provided their reasons for not having regular follow up. The predominant (53.3%, 32/60) reason was the participant assumed that the follow-up visit was not a necessity, followed up by “being too busy” with 16.7% (10/60). Financial constraints and others (including long waiting time to see the doctor, home follow-up) ranked equally third with 15.0% (9/60).
Physical activities of the study participants
Of the 132 participants, 37.1% (49/132) reported to practice physical exercises with walking as the predominant exercise. 62.9% (83/132) did not practice any physical activity. In working place, 60.8% (31/51) of the participants sat for more than 2 hours at work and 55.3% (73/132) sat at home for > 2 hours. In recording those who sat for > 2 hours at work or at home as an unhealthy and as healthy those who replied they sat < 1 hour at home or work and those who sat 1-2 hours at work or home, table 4.6 revealed that 64.4% (85/132) of the participants had an unhealthy sitting time either at work or at home.
In each of the two administrative units, the proportion of participants with an unhealthy sitting time at work or home was higher (70.8% in Alshohada & Soba vs 56.7% in Al Jabal) than those who had a healthy sitting time (29.2% vs 43.3%). However, there was no statistically significant association (p= 0.091) between administrative unit and time spent in sitting at workplace/home. A statistically significant association (p= 0.028) was found between the sitting time spent at workplace/home and gender.
Dietary habits of the study participants
Food intakes
Fruit daily consumption was reported as to be “always” by 43.2% (57/132) of the participants, 54.5% (72/132) consumed fruits “occasionally” and 2.3% (3/132) “never” had fruits. In the overall fruits was consumed “always” by 43.2% of the participants and “occasionally/never” by 56.8%. The daily consumption of vegetables was reported as “always” by 65.9% (87/132) on the participants, 33.3% (44/132) had vegetables “occasionally” and one participant (0.8%) never ate vegetables. In conclusion, the daily consumption of vegetables was “always” for 65.9% of the participants and “occasionally/never” for the remaining 34.1% (45/132) participants.
]The food intakes in a week were recorded through four variables which were namely having assida/kisra (meal made with sorghum/ millet/ maize), rice, red meat and salty foods. Each of those variables was recorded as ‘always”, “Once a week/occasionally” and “never”. Regarding assida/ kisra, most (70.5%, 93/132) of the participants had it “once a week/occasionally”, 18.9% (25/132) ate always assida/ kisra, and 10.6% (14/132) never ate assida/kisra. Rice was consumed once a week by 83.3% (110/132) of the participants, 7.6% (10/132) daily and 9.1% (12/132) never had rice.
The frequency of regular (always) consumption of salty foods in a week was higher (71.4%, 20/28) in “Al Jabal” than in “Alshohada & Soba” (28.6%, 8/28) where 60.2% (59/98) “never” consumed processed salty foods. The frequency of consumption of salty foods was statistically different (p=0.004) between the administrative units. The frequency of the foods was not statistically associated (p > 0.05) with the gender of the participants.
Having meals outside home in a week was recorded as “always”, “occasionally” for the participants who replied either once a week or occasionally and “never”. Having meals occasionally was reported by 69.7% (92/132) of the participants, 10.6% (14/132) had meals outside and 19.7% (26/132) had never ate outside home in a week. Of the 26 participants who reported never eat outside home, 50.0% lived in “Alshohada & Soba” and the remaining 50% resided in “Al Jabal”. The observed differences between frequency of having meals outside home and the administrative area of residence was not statistically significant (p= 0.158). The chi-square for trend of 2.638 indicated a not statistically difference (p=0.267) between gender and having meals outside.
Soft drink consumption collected as “always”, “once a week”, “occasionally” and “never” was recorded as healthy soft drink habit when participants answered “never” and those who replied either “once a week”, “occasionally” or “always” were recorded as having unhealthy habits towards soft drinks. 50.8% (67/132) reported having a healthy habit towards soft drinks.
Healthy juice drink habits were compared with unhealthy juice drink behavior. Participants who replied “drinking always juice without sugar” and those who answered that they “never drink juice with sugar” were coded as having a healthy juice drinking habits and those who answered by any other response to drinking juice without sugar or with sugar had their replies coded as an unhealthy juice drinking habits. In the overall, the majority (85.6%, 113/132) of the participants had an unhealthy habit towards drinking juice and only 14 participants out of hundred (19/132) had a healthy habit.
Regarding consumption of sweets, cakes and ice cream in a week, 78.8% (104/132) had an unhealthy habit and 21.2% (28/132) had healthy habits towards sweets.
86.4% reported to consume tea, 60.6% took coffee, smokers of cigarettes at the time of interview represented 5.3% and 1.5% reported that they used to have alcohol.
| NCDs | Risk factor | B1 | Wald² | df3 | p-value | OR4 | 95% CI for OR | |
|---|---|---|---|---|---|---|---|---|
| Lower | Upper | |||||||
| Diabetes Mellitus | Intercept | -2.372 | 0.209 | 1 | 0.648 | |||
| Administrative unit | 0.210 | 0.060 | 1 | 0.806 | 1.234 | 0.230 | 6.619 | |
| Gender | -1.447 | 1.919 | 1 | 0.166 | 0.235 | 0.030 | 1.823 | |
| Age in years | 0.023 | 0.567 | 1 | 0.451 | 1.023 | 0.964 | 1.086 | |
| Education | 0.321 | 0.335 | 1 | 0.562 | 1.378 | 0.465 | 4.082 | |
| Marital Status | 0.495 | 0.492 | 1 | 0.483 | 1.640 | 0.411 | 6.538 | |
| Profession | -1.282 | 2.301 | 1 | 0.129 | 0.278 | 0.053 | 1.454 | |
| Household size | -0.097 | 0.266 | 1 | 0.606 | 0.908 | 0.628 | 1.311 | |
| Treatment duration (years) | -0.600 | 0.428 | 1 | 0.513 | 0.549 | 0.091 | 3.317 | |
| Adherence to treatment | -0.956 | 0.856 | 1 | 0.355 | 0.384 | 0.051 | 2.911 | |
| Follow up visits | 0.877 | 1.439 | 1 | 0.230 | 2.405 | 0.573 | 10.084 | |
| Physical exercise | 2.139 | 3.849 | 1 | 0.050 | 8.488 | 1.002 | 71.903 | |
| Vegetables | 0.170 | 0.021 | 1 | 0.884 | 1.185 | 0.121 | 11.570 | |
| Fruits | 0.587 | 0.355 | 1 | 0.552 | 1.799 | 0.260 | 12.419 | |
| Meals outside home | 1.535 | 1.813 | 1 | 0.178 | 4.643 | 0.497 | 43.376 | |
| Sitting (home/work place) | 1.306 | 1.788 | 1 | 0.181 | 3.691 | 0.544 | 25.038 | |
| Hypertension | Intercept | -3.098 | 0.279 | 1 | 0.598 | |||
| Administrative unit | 0.092 | 0.009 | 1 | 0.923 | 1.096 | 0.172 | 6.982 | |
| Gender | -2.489 | 3.493 | 1 | 0.062 | 0.083 | 0.006 | 1.129 | |
| Age in years | 0.071 | 3.855 | 1 | 0.050 | 1.074 | 1.000 | 1.152 | |
| Education | 0.023 | 0.001 | 1 | 0.971 | 1.023 | 0.297 | 3.524 | |
| Marital Status | 0.648 | 0.712 | 1 | 0.399 | 1.911 | 0.424 | 8.608 | |
| Profession | -2.306 | 5.135 | 1 | 0.023 | 0.100 | 0.014 | 0.732 | |
| Household size | -0.141 | 0.478 | 1 | 0.489 | 0.868 | 0.582 | 1.296 | |
| Treatment duration (years) | -0.700 | 0.478 | 1 | 0.489 | 0.497 | 0.068 | 3.607 | |
| Adherence to treatment | -0.493 | 0.200 | 1 | 0.655 | 0.611 | 0.071 | 5.289 | |
| Follow up visits | 1.583 | 4.076 | 1 | 0.044 | 4.871 | 1.047 | 22.658 | |
| Physical exercise | 2.757 | 5.365 | 1 | 0.021 | 15.760 | 1.528 | 162.522 | |
| Vegetables | 0.977 | 0.648 | 1 | 0.421 | 2.657 | 0.246 | 28.668 | |
| Fruits | 0.642 | 0.359 | 1 | 0.549 | 1.900 | 0.233 | 15.516 | |
| Meals outside home | 1.603 | 1.788 | 1 | 0.181 | 4.969 | 0.474 | 52.105 | |
| Sitting (home/work place) | 0.562 | 0.290 | 1 | 0.590 | 1.754 | 0.227 | 13.565 | |
Table 2a: Logistic regression estimating the fifteen risk factors associated to four NCDs.
Relationship between non-communicable diseases and their associated factors
The NCDs reported by the study participants were regrouped in five categories namely diabetes mellitus (35.2%, 43/122), hypertension (23.0%, 28/122), diabetes mellitus associated to hypertension (23.0%, 28/122), cardiovascular disease associated to diabetes mellitus and hypertension (9.8%, 12/122) and other NCDs (9.0%, 11/122). The other NCDs included asthma, osteoarthritis, cancer, rheumatoid arthritis, hyperthyroidism and hypothyroidism. A logistic regression analysis was performed to estimate the risk factors associated to the NCDs above listed in taking as a reference group the fifth category (other NCDs).
Diabetes mellitus: table 2a revealed that none of the fifteen risk factors was statistically associated (p > 0.05) to the condition. However, physical activity highly contributed to the model by 8.5 times ([95 % CI: 1.002-71.903], p=0.050) as well as having meals outside home (OR=4.643, [95 % CI: 0.497-43.376], p=0.178), time of sitting at workplace/home (OR=3.691, [95 % CI: 0.544-25.038], p=0.181) and adherence to follow up of medical visits (OR=2.405, [95 % CI: 0.573- 10.084], p=0.230). Consumption of fruits contributed to the model by 1.8 times ([95 % CI: 0.260-12.419], p= 0.552) and marital status by 1.6 times ([95 % CI: 0.411-6.538], p= 0.483). Other risk factors contributing to the model for > 1 time to the model were consumption of vegetables, administrative unit of residence and education as indicated by table 2a.
Hypertension: a statistically significant association was found between hypertension and physical activity which contributed by 16 times ([95 % CI: 1.528-162.522], p= 0.021); other statistically significant risk factors were profession (p=0.023) and adherence to follow up visit (p=0.044) contributing to explain the status of hypertension in the study population by respectively < 1 time [95% CI: 0.014-0.732] and 5 times [95% CI: 1.047-22.658]. Despite a not statistically significant association with hypertension, having meals outside home contributed to explain the hypertension by 5 times ([95% CI: 0.474-52.105], p=0.181) and consuming vegetables contribute by 3 times ([95% CI: 0.246-28.668], p=0.421). Education, age in years, administrative unit, time of sitting at home/work place, consuming fruits, marital status contributed to model by more than 1 time.
Diabetes associated to hypertension: the two conditions were statistically associated with profession and education with a p-value of respectively 0.001 and 0.045. Despite a not statistically significant association, with an increasing contribution of respectively 6.8 to 9.9 times, physical activity (OR=6.830, [95% CI: 0.622-74.932], p= 0.116) treatment duration, consumption of vegetables and having meals outside home (OR=9.873, [95% CI: 0.824-118.305], p= 0.071) explained the association of diabetes and hypertension. Whereas, the time of sitting at home/workplace contribute by 4 times (OR: 3.984, 95% CI: 0.488-32.509], p=0.197). Table 2b displayed the other risk factors contributing for < 2 times.
Cardiovascular Disease associated to diabetes mellitus and Hypertension.
The highly statistically significant contributor associated to these three conditions was having meals outside home contributing for 63 times ([95% CI: 3.786-1063.733], p=0.004). Another statistically significant risk factor was gender (p=0.020) and its coefficient of contribution of -4.169 indicated that males might be more likely to have the association of the three conditions. Table 2b revealed an increasing contribution ranging from 2 times to 5.2 times for treatment duration, education, time of sitting (home/work place), fruit consumption, adherence to treatment, physical activity and marital status.
In conclusion, the risk factors statistically associated with NCDs in this study were age, gender of the participants, their profession, education level, physical activities, followup visits and having meals outside home (Tables 2a and 2b).
| NCDs | Risk factor | B | Wald | df | p-value | OR | 95% CI for OR | |
|---|---|---|---|---|---|---|---|---|
| Lower | Upper | |||||||
| Diabetes & Hypertension | Intercept | -10.138 | 2.355 | 1 | 0.125 | |||
| Administrative unit | -0.639 | 0.432 | 1 | 0.511 | 0.528 | 0.078 | 3.55 | |
| Gender | -1.837 | 1.653 | 1 | 0.199 | 0.159 | 0.01 | 2.62 | |
| Age in years | 0.108 | 7.483 | 1 | 0.006 | 1.114 | 1.031 | 1.203 | |
| Education | 1.385 | 4.027 | 1 | 0.045 | 3.994 | 1.033 | 15.441 | |
| Marital Status | 0.684 | 0.697 | 1 | 0.404 | 1.982 | 0.397 | 9.887 | |
| Profession | -3.696 | 11.563 | 1 | 0.001 | 0.025 | 0.003 | 0.209 | |
| Household size | 0.032 | 0.023 | 1 | 0.879 | 1.032 | 0.685 | 1.555 | |
| Treatment duration (years) | 1.96 | 2.751 | 1 | 0.097 | 7.101 | 0.7 | 72.003 | |
| Adherence to treatment | -1.363 | 1.194 | 1 | 0.275 | 0.256 | 0.022 | 2.951 | |
| Follow up visits | -0.744 | 0.755 | 1 | 0.385 | 0.475 | 0.089 | 2.544 | |
| Physical exercise | 1.921 | 2.471 | 1 | 0.116 | 6.83 | 0.622 | 74.932 | |
| Vegetables | 2.18 | 2.67 | 1 | 0.102 | 8.843 | 0.647 | 120.773 | |
| Fruits | -0.721 | 0.422 | 1 | 0.516 | 0.486 | 0.055 | 4.285 | |
| Meals outside home | 2.29 | 3.266 | 1 | 0.071 | 9.873 | 0.824 | 118.305 | |
| Sitting (home/work place) | 1.382 | 1.666 | 1 | 0.197 | 3.984 | 0.488 | 32.509 | |
| Intercept | -4.799 | 0.437 | 1 | 0.509 | ||||
Cardiovascular Disease associated to Diabetes Mellitus and Hypertension |
Administrative unit | -2.091 | 2.342 | 1 | 0.126 | 0.124 | 0.008 | 1.798 |
| Gender | -4.169 | 5.443 | 1 | 0.02 | 0.015 | 0 | 0.513 | |
| Age in years | 0.06 | 1.807 | 1 | 0.179 | 1.061 | 0.973 | 1.158 | |
| Education | 0.791 | 0.934 | 1 | 0.334 | 2.206 | 0.443 | 10.986 | |
| Marital Status | 1.651 | 3.205 | 1 | 0.073 | 5.213 | 0.855 | 31.779 | |
| Profession | -3.219 | b | 1 | 0.013 | 0.04 | 0.003 | 0.508 | |
| Household size | -0.541 | 3.802 | 1 | 0.051 | 0.582 | 0.338 | 1.003 | |
| Treatment duration (years) | 0.706 | 0.263 | 1 | 0.608 | 2.025 | 0.136 | 30.091 | |
| Adherence to treatment | 1.503 | 0.908 | 1 | 0.341 | 4.497 | 0.204 | 99.107 | |
| Follow up visits | -1.02 | 0.714 | 1 | 0.398 | 0.36 | 0.034 | 3.844 | |
| Physical exercise | 1.581 | 1.214 | 1 | 0.271 | 4.857 | 0.292 | 80.817 | |
| Vegetables | 0.62 | 0.179 | 1 | 0.672 | 1.859 | 0.105 | 32.805 | |
| Fruits | 1.186 | 0.806 | 1 | 0.369 | 3.273 | 0.246 | 43.587 | |
| Meals outside home | 4.15 | 8.327 | 1 | 0.004 | 63.465 | 3.786 | 1063.733 | |
| Sitting (home/work place) | 0.813 | 0.334 | 1 | 0.564 | 2.254 | 0.143 | 35.556 | |
Table 2b: Logistic regression estimating the fifteen risk factors associated to four NCDs.
Discussion
In this study, the most frequent NCDs reported were diabetes mellitus (33.0%), hypertension (23.5%) and the comorbidity diabetes mellitus associated to hypertension (21.1%, 28/132). 22.1% of the participants suffered from a single NCD or combined two to three NCDs. In the overall, diabetes mellitus prevailed in 8 participants/100,000 total population, hypertension in 6 per 100,000 and the association diabetes mellitus affected 5 persons/100,000 populations. These results were much higher than the results obtained from a previous study conducted by Abdalla EAM et al. [7] revealed in Jabra (Khartoum State, Sudan) where diabetes prevalence was 18.6% lower than ours, elsewhere Our results were the highest in the literature; in South Africa [30] a prevalence of diabetes of 5.0% was reported, in Kenya the prevalence of diabetes mellitus was 2.6% [31] and in Ethiopia, it ranged between 0.5% and 5.3% [23]. In South America, diabetes mellitus prevalence ranged from < 5.0% in Peru to 8.39% in Mexico [32, 33]. Ma D. et al. revealed that diabetes prevalence was 6.9% in Japan, 9.2% in Korea and 13.1% in China [34].
The WHO STEPS conducted in Iran reported than the prevalence of diabetes mellitus in urban area (11.1%) was higher than in rural (7.4%), this result is differ from the present study, the prevalence in urban area (7.79%) was lowest than in rural 8.13% [35].
Regarding hypertension, our prevalence of 23.5% was lower than those already reported by various authors who found a prevalence ranging from 27.6% to 35.7% [5,6,29] On the African continent, a prevalence of 16.5% was reported in South Africa, and 24.8% in Kenya; whereas in South America, a hypertension prevalence of 11.14% was published in Mexico and 15.0%, in Peru. In Asia, the prevalence of hypertension was higher in China (24.5%) than in Korea (17.6%) and in Japan where a prevalence of 15.2% were published [30-34].
Ahmed M.H. et al. [36] reported in Khartoum State and Atabra (North of Sudan) a prevalence of Acute Coronary Syndrome (ACS is a cardiovascular disease) was 5.44% in 496 participants living with diabetes; in our research, cardiovascular disease was associated with diabetes mellitus in 3.0% of our study population. The combination of more than two NCDs was investigated by Alcalde-Rabanal JE et al. [33] in Mexico who reported the complex scenario of obesity, diabetes and hypertension on a sample of 10,326 participants and revealed that 73.0% suffered from diabetes, hypertension and/or overweight/obesity.
In this study, a statistically significant association was found between hours spent sitting at workplace/home and gender (p=0.028) and having salty food (processed food) and residence area (p=0.004).
A limitation of our research could be related to the use of a researcher designed questionnaire instead of using and adapting the WHO stepwise approach to chronic disease risk factor surveillance tool. Nonetheless, the research instrument developed provided data which through a multi logistic regression analysis enabled us to estimate the risk factors associated to one or more NCDs.
This study indicated that the risk factors statistically associated with NCDs were age (OR= 1.114, 95% CI: 1.031- 1.203], p= 0.006) in participants suffering from diabetes associated to hypertension, their gender (OR= 0.015, 95% CI: 0.000-0.513], p= 0.020) in participants suffering from the comorbidities cardiovascular disease, hypertension and diabetes, profession in patients living with hypertension (OR= 0.100, 95% CI: 0.014-0.732], p= 0.023) and those with diabetes associated to hypertension (OR= 0.025, 95% CI: 0.003-0.209], p=0.001). Education was statistically associated with the combined association of diabetes mellitus and hypertension (OR= 3.994, 95% CI: 1.033-15.441], p= 0.045). Having a regular follow up visit was statistically associated with the hypertension (OR= 4.871, 95% CI: 1.047-22.658], p= 0.044). Physical activities were statistically associated (OR= 15.76, 95% CI: 1.528-162.522], p= 0.021) in patients with hypertension. Having meals outside home (OR= 63.465, 95% CI: 3.786-1063.733], p= 0.004) was statistically associated and highly contributed with the combination of hypertension, diabetes and cardiovascular disease.
Non-communicable diseases are the results of complex interactions between the genetic make-up of an individual, lifestyle and environmental factors. In Sudan, age, gender, ethnic group, education level, family history of hypertension, family history of diabetes, residence, obesity, smoking, physical activity, salt and sugar intakes, renal problems, and pancreatic disease have been reported as risk factors of NCDs by various authors [5-7,29,36]. In the neighboring Ethiopia, low fruit consumption was reported [37] to account for 11.9% of NCD deaths which occurred in 2013, other risk factors published were alcohol consumption [30, 32].
The differences of NCDs prevalence between this study and the other literature could be due to country differences or due to applying different methodologies.
Conclusion
This study revealed that NCDs ’overall prevalence in AlShohada/Soba and Al Jabal was 24/100000 with higher frequency in AlShohada/Soba unit. Of the fifteen risk factors associated to NCDs in the two administrative units, seven were statistically associated (p < 0.05) with NCDs.
This community-based study demonstrates the urge to consider NCDs a national public health priority with particular attention to diabetes and hypertension. Early detection and prevention of these NCDs as well as their long-term management will decrease the premature death from these chronic diseases. Prevention and control of NCDs appeal collaborative efforts and sustained partnership between all primary health care providers specially the pharmacists who are a corner stone in the prevention and management of NCDs. National actions in Sudan, backed up by a strong political will and engagement will enable the country to achieve the WHO health target and reduce by one third premature deaths related to NCDs.
Acknowledgment
We would like to recognize and acknowledge our study participants whose contributions were crucial to bring our research to a successful end. Our sincere thanks to Mayada Abdarahman Abdin and Israa Giha for their support and guidance throughout this research.
Contribution of the Authors
SAMS: Designed and implemented the research, conducted the statistical analysis and drafted the initial manuscript.
AMAS: Actively involved in field implementation of the research and in computerizing the study data.
MAAA: Actively involved in field data collection.
MN: Approved the research proposal, guided the statistical analysis and proofread the initial and the final manuscript.
All the authors read and approved the final version of the manuscript prior its submission.
Data Availability
The authors declared that if the submitted manuscript is accepted for publication, the data will be deposit in the generalized repository of Dryad.
Supportive information
S1: Figure 1: Sampling frame of households in Soba/Alshohada delineated through Google Earth Pro 7.1.8.3036 (32-bit).
S2: Figure 2: geographical distributions of 50 households selected in Soba/ Ashohada through Google Earth Pro 7.1.8.3036 (32-bit).
S3: Figure 3: Sampling frame of households in Aljabal delineated through Google Earth Pro 7.1.8.3036 (32-bit).
S4: Figure 4: geographical distributions of 50 households selected in Aljabal through Google Earth Pro 7.1.8.3036 (32-bit).
Figure 1: Sampling frame of households in Soba/Alshohada delineated through Google Earth Pro 7.1.8.3036 (32-bit).
Figure 2:geographical distributions of 50 households selected in Soba & Ashohada through Google Earth Pro 7.1.8.3036 (32-bit).
Figure 3: Sampling frame of households in Aljabal delineated through Google Earth Pro 7.1.8.3036 (32-bit).
Figure 4: geographical distributions of 50 households selected in Aljabal through Google Earth Pro 7.1.8.3036 (32-bit).
Source of financing
The research was fully supported by Samah Mohamed Aabdin Sayed in the frame work of the fulfilment of her Master of Sciences in Public and Tropical Health in the University of Medical Sciences and Technology.
Conflict of interest
No conflict of interest.
Ethical clearance
The research proposal was approved by Sumasri Institutional Review Board in the frame work of a communitybased survey. Authorization for the implementation of the research was obtained from each study participants after providing their well-informed consent. The confidentiality of the participants was ensured through the use of anonymous research tool. The participants were reassured that the data collected from them will not be used for any other purpose other than the objectives assigned.
World Health Organization 2018. World Health Statistics 2018. Monitoring Health for SDGs.[ Ref ]
https://www.who.int/news-room/fact-sheets/detail/ noncommunicable-diseases[ Ref ]
GBD 2017 Causes of Death Collaborators(2018) Global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980–2017: a systematic analysis for the Global Burden of Disease Study 2017. GHM 392: 1736-1788.[ Ref ]
WHO: Non communicable Diseases Country Profiles 2018. ISBN 978-92- 4-151462-0.[ Ref ]
. Awadalla H, Elmak NE, El-Sayed EF, Almobarak AO, Elmadhoun WM, et al. (2018) Hypertension in Sudanese individuals and associated risk factors: the critical intersection between salt and sugar intake. Cardiovasc Diagn Ther 8: 432-438.[ Ref ]
Bushara OS, Noor SK, Ahmed MH (2016) Prevalence of and risk factors for hypertension among urban communities of North Sudan: Detecting a silent killer. J Family Med Prim Care 5: 605-610.[ Ref ]
. Abdalla EAM, Ahmed RF (2017) Epidemiology of diabetes among adults in Jabra area ‘’ block 14’’ in Khartoum state – Sudan: community based study. Int J Community Med Public Health 4:1863-1869.[ Ref ]
Arokiasamy P, Uttamacharya, Kowal P, Capistrant BD, Gildner TE, et al. (2017) Chronic Noncommunicable Diseases in 6 Low- And Middle-Income Countries: Findings From Wave 1 of the World Health Organization’s Study on Global Ageing and Adult Health (SAGE).Am J Epidemiol 1-15.[ Ref ]
Malta DC, Ivata Bernal RT, Marinho de Souza MF, Szwarcwald CL, Guimarães Lima MG (2013) Social inequalities in the prevalence of selfreported chronic non-communicable diseases in Brazil: national health survey 2013. Int J Equity Health 15: 153.[ Ref ]
Kraja F, Kraja B, Mone I, Harizi I, Babameto A, et al. (2016) Self-reported prevalence and risk factors of non-communicable diseases in the Albanian adult population. Med Arch 70: 208-212.[ Ref ]
Zhao C, Wong L, Zhu Q, YangH (2018) Prevalence and correlates of chronic diseases in an elderly population: A community-based survey in Haikou. PLoSONE 13: e0199006.[ Ref ]
WHO: Noncommunicable Diseases country profile 2014. [ Ref ]
Rahman MM, Rahman Md, Tahmin Sajani T, Kawser A (2017) Prevalence of NCDs among Rural Households of Dhamrai Upazila, Dhaka. Anwer Khan Modern Medical College Journal 8: 51-55.[ Ref ]
Cetorelli V, Burnham G, Shabila N (2017) Prevalence of noncommunicable disease and access to health care and medications among Yazidis and other minority groups displaced by ISIS in to the Kurdistan Region of Iraq. Confl Health 11: 4.[ Ref ]
Rehl M, Shoaib M, Ellithy S, Okour S, Ariti C, et al. (2018) Prevalence of non-communicable diseases and access to care among non-camp Syrian refugees in northern Jordan. Confl Health 12: 33.[ Ref ]
Ashour M, Zaid AA (2017) Prevalence of non-communicable diseases and use of health services in Gaza Strip: an analysis of a household survey. The Lancet 390: S36.[ Ref ]
Kavishe B, Biraro S, Baisley K, Vanobberghen F, Kapiga S, et al. (2015) High prevalence of hypertension and of risk factors for non-communicable diseases (NCDs): a population based cross-sectional survey of NCDS and HIV infection in Northwestern Tanzania and Southern Uganda. BMC Medicine 126.[ Ref ]
Guwatudde D, Mutungi G, Wesonga R, Kajjura R, Kasule H, et al. (2015) The epidemiology of hypertension in Uganda: Findings from national non-communicable diseases risk factors survey. PLOS ONE 25: 10.[ Ref ]
Cundale K, Wroe E, Matanje-Mwagomba BL, Muula AS, Gupta N, et al. (2017) Reframing non-communicable diseases and injuries for the poorest Malawians: The Malawi National NCDI Poverty Commission. Malawi Med J 29: 194-197.[ Ref ]
Gowshall M, Taylor-Robinson SD (2018) The increasing prevalence of non-communicable diseases in low-middle income countries: the view from Malawi. Int J Gen Med 11:255-264.[ Ref ]
Mawaw PM, Yav T, Mukuku O, Lukanka O, Kazadi PM, et al. (2017) Prevalence of obesity, diabetes mellitus, hypertension and associated risk factors in mining workers, Democratic Republic of Congo. Pan Afr Med J 28: 282.[ Ref ]
Endriyas M, Mekonnen E, Dana T, Daka K, Misganaw T, et al. (2018) Burden of NCDs in SNNP region, Ethiopia: a retrospective study. BMC Health Serv Res 18: 520.[ Ref ]
Misganaw A, Mariam DH, Ali A, Araya T (2014) Epidemiology of major non-communicable diseases in Ethiopia: A systematic review. J Health Popul Nutr 32: 1-13.[ Ref ]
Hosseinpoor AZ, Bergen N, Kunst A, Harper S, Guthold R, et al. (2012) Socioeconomic inequalities in risk factors for non-communicable diseases in low-income and middle-income countries: results from the World Health Survey. BMC Public Health 2012 12:912.[ Ref ]
Ikeda N, Inoue M, Iso H, Ikeda S, Satoh T, et al. (2012) Adult Mortality Attributable to Preventable Risk Factors for Non-Communicable Diseases and Injuries in Japan: A Comparative Risk Assessment. PLoS Med 9: e1001160.[ Ref ]
Bhagyalaxmi A, Atul T, Shikha J (2013) Prevalence of Risk Factors of Non-communicable Diseases in a District of Gujarat, India. J Health Popul Nutr 31: 78-85.[ Ref ]
Olawuyi AT, Adeoye IA (2018) The prevalence and associated factors of non-communicable disease risk factors among civil servants in Ibadan, Nigeria. PLoSONE 13: e0203587.[ Ref ]
Agaba EI, Akanbi MO, Agaba PA, Ocheke AN, Gimba ZM, et al. (2017) A survey of non-communicable diseases and their risk factors among university employees : a single institution study. Cardiovasc J Afr 28: 377-384.[ Ref ]
Ghebreselasie DT (2016) Risk factors of non-communicable diseases among population in Wad-Medani City, Gezira State, Sudan (2013). Health Care: Current Reviews 4:3.[ Ref ]
http://www.hsrc.ac.za/uploads/pageNews/72/SANHANESlaunch%20edition%20(online%20version).pdf[ Ref ]
Wekesahet FM, Nyanjau L, Kibachio J, Mutua MK, Mohamed SF, et al. (2018) Individual and household level factors associated with presence of multiple non-communicable disease risk factors in Kenyan adults. BMC Public Health 18:1220.[ Ref ]
Heitzingeret K, Montano SM, Hawes SE, O Alarcon J, Zunt JR (2014) A community-based cluster randomized survey ofnoncommunicable disease and risk factors in aperi-urban shantytown in Lima, Peru. BMC Int Health Hum Rights 14:19.[ Ref ]
Alcalde-Rabanal JE, Orozco-Nu ́ñez E, Espinosa-Henao OE, ArredondoLo ́pez A, Alcayde-Barranco L (2018) The complex scenario of obesity, diabetes and hypertension in the area of influence of primary healthcare facilities in Mexico. PLoS ONE 13: e0187028.[ Ref ]
Ma Defu, Sakai H, Wakabayashi C, Kwon JS, Lee Y, et al. (2017) The prevalence and risk factor control associated with noncommunicable diseases in China, Japan, and Korea, J Epidemiol 27:568-573.[ Ref ]
Khorrami Z, Yarahmadi S, Mahdavi Hazaveh AL (2017) Urban-Rural Differences in the Prevalence of Self-Reported Diabetes and its Risk Factors: The WHO STEPS Iranian Noncommunicable Disease Risk Factor Surveillance in 2011. Iran J Med Sci 42: 481-487.[ Ref ]
Ahmed MH, Awadalla H, Elmadhoun MW, Osman M, Noor SK, et al. (2017) Prevalence and Risk Factors for Acute Coronary Syndrome Among Sudanese Individuals with Diabetes: A Population-Based Study. Cardiol Res 8: 184-189.[ Ref ]
Melaku YA, Temesgen AM, Forouzanfar MH (2016) The impact of dietary risk factors on the burden of non-communicable diseases in Ethiopia: findings from the Global Burden of Disease study 2013. Int J Behav Nutr Phys Act 13: 122.[ Ref ]