Journal Name: International Journal of Endocrinology Research
Article Type: Research
Received date: 07 February, 2019
Accepted date: 23 February, 2019
Published date: 28 February, 2019
Citation: Aljabri KS, Alnasser IM, Facharatz, Bokhari SA, Alshareef MA, et al. (2019) The Association between Hypothyroidism and Chronic Renal Failure in Patients with Type 2 Diabetes Mellitus. Int J Endocrinol Res Vol: 2, Issue: 1 (09-12).
Copyright: © 2019 Aljabri KS, et al. This is an openaccess article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Background and objective: Hypothyroidism is often associated with kidney diseases. The present retrospective study was conducted to find out the association between hypothyroidism and Chronic Renal Failure (CRF) and Type 2 Diabetes Mellitus (T2DM) in Saudi community based hospital.
Design: We analyzed retrospectively 1286 participants whom are between the ages 20 to 96 years. All patients were from the population of the Primary health centre at King Fahad Armed Forces Hospital, Jeddah, Saudi Arabia. All data were collected on the basis of a review of electronic medical data. Participants were defined as having type 2 diabetes mellitus (T2DM) according to self-report, clinical reports, use of anti-diabetic agents or HbA1c (≥6.5). All patients in the present study fulfilled the revised National Kidney Foundation criteria for the diagnosis of chronic renal failure (CRF). The total number of cohort was separated on basis of age values into four groups: <40 years, 40-49 years, 50-59 years and ≥60 years.
Results: 1286 subjects with T2DM were included. There were 346 cases (26.9%) males and 940 cases (73.1%) were females with mean age 55.4±12.3. There were 66 cases (5.1%), 736 cases (57.2%) and 241 cases (18.7%) with CKD, HTN and hypothyroidism respectively. The mean HbA1c was 8.1±2.2 where as he means TSH and FT4 value were 3.7±7.2 mIU/l and 15.1±2.9 pmol/l respectively. Among cases of CRF with T2DM, hypothyroidism was found in 21 cases (38.1%), p=0.005. Males were more prevalent than females, 61.9% vs 38.1% respectively, p<0.0001. Male gender, age, HTN, presence of hypothyroidism and HbA1c were associated with higher likely hood of CRF, (OR=5.4; 95% Confidence Interval [CI]=3.1, 9.4), p<0.0001), (OR=1.1; 95% CI=1.03, 1.1), p<0.0001), (OR=3.1; 95% CI=1.5, 6.4), p=0.002), (OR=3.5; 95% CI=1.9, 5.4), p<0.0001) and (OR=1.2; 95% CI=1.1, 1.3), p=0.003) respectively. The prevalence of hypothyroidism in cases of CRF IN T2DM was higher across all age groups and were more prevalent in the seventh decade (24.2% vs 4.7%) compared to cases with no CRF.
Conclusion: We conclude that despite the limitations of this hospital-based retrospective study, hypothyroidism is highly prevalent in cohort of Saudis with CRF and T2DM. The majority of our patients were males. These two observations remain to be validated by population-based studies.
Keywords
Hypothyroidism, Chronic renal failure, Type 2 Diabetes.
Abstract
Background and objective: Hypothyroidism is often associated with kidney diseases. The present retrospective study was conducted to find out the association between hypothyroidism and Chronic Renal Failure (CRF) and Type 2 Diabetes Mellitus (T2DM) in Saudi community based hospital.
Design: We analyzed retrospectively 1286 participants whom are between the ages 20 to 96 years. All patients were from the population of the Primary health centre at King Fahad Armed Forces Hospital, Jeddah, Saudi Arabia. All data were collected on the basis of a review of electronic medical data. Participants were defined as having type 2 diabetes mellitus (T2DM) according to self-report, clinical reports, use of anti-diabetic agents or HbA1c (≥6.5). All patients in the present study fulfilled the revised National Kidney Foundation criteria for the diagnosis of chronic renal failure (CRF). The total number of cohort was separated on basis of age values into four groups: <40 years, 40-49 years, 50-59 years and ≥60 years.
Results: 1286 subjects with T2DM were included. There were 346 cases (26.9%) males and 940 cases (73.1%) were females with mean age 55.4±12.3. There were 66 cases (5.1%), 736 cases (57.2%) and 241 cases (18.7%) with CKD, HTN and hypothyroidism respectively. The mean HbA1c was 8.1±2.2 where as he means TSH and FT4 value were 3.7±7.2 mIU/l and 15.1±2.9 pmol/l respectively. Among cases of CRF with T2DM, hypothyroidism was found in 21 cases (38.1%), p=0.005. Males were more prevalent than females, 61.9% vs 38.1% respectively, p<0.0001. Male gender, age, HTN, presence of hypothyroidism and HbA1c were associated with higher likely hood of CRF, (OR=5.4; 95% Confidence Interval [CI]=3.1, 9.4), p<0.0001), (OR=1.1; 95% CI=1.03, 1.1), p<0.0001), (OR=3.1; 95% CI=1.5, 6.4), p=0.002), (OR=3.5; 95% CI=1.9, 5.4), p<0.0001) and (OR=1.2; 95% CI=1.1, 1.3), p=0.003) respectively. The prevalence of hypothyroidism in cases of CRF IN T2DM was higher across all age groups and were more prevalent in the seventh decade (24.2% vs 4.7%) compared to cases with no CRF.
Conclusion: We conclude that despite the limitations of this hospital-based retrospective study, hypothyroidism is highly prevalent in cohort of Saudis with CRF and T2DM. The majority of our patients were males. These two observations remain to be validated by population-based studies.
Keywords
Hypothyroidism, Chronic renal failure, Type 2 Diabetes.
Introduction
Diabetic nephropathy (44.73%) was the leading cause of End-Stage Renal Failure (ESRF) [1-3]. Hypothyroidism often associated with kidney diseases through reduction in cardiac output and renal blood flow and finally the Glomerular Filtration Rate (GFR) which results in an elevation in the serum levels of creatinine and a reduction in its clearance [4-10]. Many case reports and small case series documented increased levels of serum creatinine with hypothyroidism [4-8]. The importance of understanding the impact of thyroid dysfunction on renal function is highlighted by studies indicating hypothyroidism is common in patients with estimated glomular filtration rate (eGFR) <60 ml/ min per 1.73 m2 [11,12]. The prevalence of hypothyroidism increased from 7% to 17.9% in individuals whose GFR has decreased from ≥90 mL/min to 60 mL/min [11]. In addition, previous studies have suggested an increased prevalence of hypothyroidism in patients with ESRD requiring maintenance dialysis [11-13].
Although numerous hypothesis for contributing factors, like altered iodine metabolism, decreased peripheral sensitivity to hormones, and autoimmune thyroiditis, the exact underlying mechanisms linking advanced Chronic Renal Failure (CRF) and primary thyroid dysfunction remain unclear [11].
Thus, the present retrospective study was conducted to find out the association between hypothyroidism and CRF in patients with type 2 diabetes mellitus (T2DM) in Saudi community-based hospital.
Methods
We analyzed retrospectively 1286 participants between the age 20 to 96 years. Patients were from the population of the Primary health centre at King Fahad Armed Forces Hospital, Jeddah, Saudi Arabia. Data were collected on the basis of a review of electronic medical data. Participants were defined as having T2DM according to self-report, clinical reports, use of anti-diabetic agents or HbA1c (≥6.5) [14]. High performance liquid chromatography was used for HbA1c analysis and was expressed as a percentage. Patients with Thyroid Stimulating Hormone (TSH) above the normal range of TSH and low Free Thyroxine (FT4) for our laboratory reference, history of hypothyroidism and taking thyroid replacement therapy were included as cases oh hypothyroidism. Patient who are pregnant were excluded. The reference range values of TSH 0.22-4.2 MIU/L, Free T4 12.0-22.0 pmol/L. Serum FT4 were estimated by radioimmunoassay and Serum TSH was estimated by Immunoradiometric assay. All patients in the present study fulfilled the revised National Kidney Foundation criteria for the diagnosis of CRF [15]. The total numbers of cohort were separated on basis of age values into four groups: <40 years, 40-49 years, 50-59 years and ≥60 years.
Statistical Analysis
Continuous variables were described using means and standard deviations. Univariate analysis of baseline demography both between groups, were accomplished using unpaired t-test and Chi square test were used for categorical data comparison. Regression analysis was performed to assess for Odd Ratio (OR). P value <0.05 indicates significance. The statistical analysis was conducted with SPSS version 23.0 for Windows.
Results
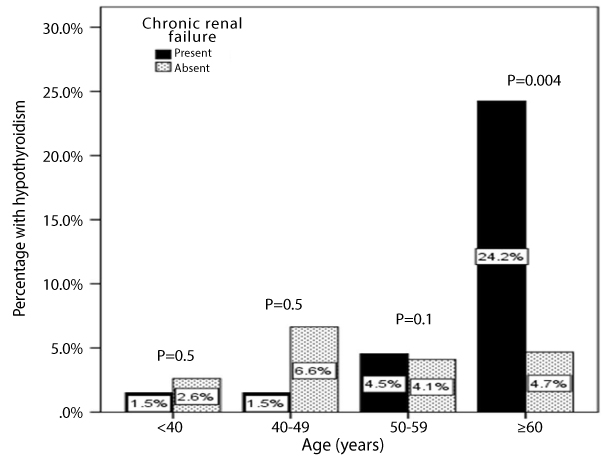
1286 subjects with T2DM were included. There were 346 cases (26.9%) males and 940 cases (73.1%) were females with mean age 55.4±12.3, table 1. There were 66 cases (5.1%), 736 cases (57.2%) and 241 cases (18.7%) with CKD, HTN and hypothyroidism respectively. The mean HbA1c was 8.1±2.2 where as he mean TSH and FT4 value were 3.7±7.2 mIU/l and 15.1±2.9 pmol/l respectively. Among cases of CRF with T2DM, hypothyroidism was found in 21 cases (38.1%), p=0.005, table 1. Males were more prevalent than females, 61.9% vs 38.1% respectively, p<0.0001. Table 2 showed the odd ratio of risk factors for patients with CRF and T2DM. Male gender, age, HTN, presence of hypothyroidism and HbA1c were associated with higher likely hood of CRF, (OR=5.4; 95% Confidence Interval [CI]=3.1, 9.4), p<0.0001) , (OR=1.1; 95% CI=1.03, 1.1), p<0.0001), (OR=3.1; 95% CI=1.5, 6.4), p=0.002), (OR=3.5; 95% CI=1.9, 5.4), p<0.0001) and (OR=1.2; 95% CI=1.1, 1.3), p=0.003) respectively. Figure 1 illustrated the frequency of hypothyroidism in different age groups for patients with T2DM with and without chronic renal failure. The prevalence of hypothyroidism in cases of CRF IN T2DM was higher across all age groups and were more prevalent in the seventh decade (24.2% vs 4.7%) compared to cases with no CRF.
Table 1: Characteristic of patients with type 2 diabetes with and without chronic renal failure [mean ± standard deviation or number (%)].
| Parameters | Total | Chronic renal failure | P value | ||
|---|---|---|---|---|---|
| Present | Absent | ||||
| Numbers | 1286 | 66 (5.1) | 1120 (94.9) | ||
| Age (years) | 55.4 ± 12.3 | 64.7 ± 10.9 | 54.9 ± 12.2 | <0.0001 | |
| Gender | Male | 346 (26.9) | 42 (63.6) | 304 (24.9) | <0.0001 |
| Female | 940 (73.1) | 24 (36.4) | 916 (75.1) | ||
| Hypothyroidism | 241 (18.7) | 21 (38.1) | 220 (18.0) | 0.005 | |
| Hypertension | 736 (57.2) | 56 (84.8) | 680 (55.7) | <0.0001 | |
| HbA1c | 8.1 ± 2.2 | 9.1 ± 2.6 | 8.1 ± 2.2 | <0.0001 | |
| TSH (mIU/l) | 3.7 ± 7.2 | 3.5 ± 3.3 | 3.7 ± 7.3 | 0.8 | |
| FT4 (pmol/l) | 15.1 ± 2.9 | 15.4 ± 2.7 | 15.1 ± 2.9 | 0.5 | |
| Serum creatinine (μmol/L) | 69.2 ± 26.1 | 145.3 ± 54.3 | 65.1 ± 15.1 | <0.0001 | |
Table 2: Regression analysis for odd ratio of risk factors for patients with chronic renal failure and type 2 diabetes.
| Parameters | Odd Ratio | P value |
|---|---|---|
| Male gender | 5.4 (3.1-9.4) | <0.0001 |
| Age (years) | 1.1 (1.03-1.1) | <0.0001 |
| Hypertension | 3.1 (1.5-6.4) | 0.002 |
| Hypothyroidism | 3.5 (1.9-5.4) | <0.0001 |
| HbA1c | 1.2 (1.1-1.3) | 0.003 |
Figure 1: Age category groups and hypothyroidism in patients with type 2 diabetes with and without chronic renal failure.
Discussion
In patients with CRF and T2DM, we found that hypothyroidism occurred in 38% with males predominant (61.9% vs. 38.1%). T2DM is the most common chronic metabolic disease which its incidence is increasing rapidly [16]. Moreover, diabetic nephropathy is one of the main chronic complications in T2DM and is currently the most common cause for ESRD [17].
Hypothyroidism is associated with reduction in GFR and increase in serum creatinine in more than half of the adults [18]. Thyroid hormones could directly affect the glomerular function, tubular secretory and absorptive capacities. As a consequence, there are alterations in clinically important renal parameters such as GFR and the urinary albumin creatinine ratio [18,19].
Multiple studies revealed an increased prevalence of hypothyroidism in T2DM. Moreover, earlier studies confirmed that hypothyroidism was not a rare disorder in CRF patients [12,20,21]. A meta-analysis of 61 studies reported the adjusted pooled prevalence of hypothyroidism in T2DM patients was 10.2% [22]. The data of 14,623 adult participants from the third National Health and Nutrition Examination Survey revealed that the prevalence of hypothyroidism was 23.1% [12]. Moreover, Bajaj S, et al. [2] showed that the prevalence of hypothyroidism was found in 57.1% and significantly associated with CRF (OR=3.5).
Our studied population was older than previously reported (64.7±10.9 years) [24]. Moreover, the prevalence of hypothyroidism increased with age [24]. In addition, the incidence of hypothyroidism is up to 4/1000 females and 1/1000 males. It was reported that hypothyroidism is found in 6–8% of women and 3% of men [25].
In contrary to other reports, we found that there was no significant difference in the TSH and free T4 levels among patients with and without CRF [26-28]. It was hypothesized that serum creatinine to be higher in hypothyroid than euthyroid patients due to increasing of vascular resistance, intra-renal vasoconstriction and endothelial dysfunction through a reduction in nitric oxide in hypothyroidism [4,8,29].
We aimed to identify the prevalence of hypothyroidism in CRF with T2DM patients in primary health care setting. Furthermore, due to the retrospective nature of this study, the observed population reflects a selected yet comprehensive group of patients rather than the general population. Our study could be limited by the question of clustering of cases within the study region and the effect that might have on our estimates, in addition, the current study population may appear limited in size and therefore may underestimate the true prevalence of hypothyroidism in CRF with T2DM patients. In addition, the study shares the limitations of all retrospective studies.
We conclude that despite the limitations of this hospitalbased retrospective study, hypothyroidism is highly prevalent in cohort of Saudis in CRF with T2DM patients. The majority of our patients in our finding were predominantly males. These two observations remain to be validated by population-based studies. In the absence of registry data, larger cooperative studies involving diverse population samples from multiple centers could help to provide further information on the true prevalence of hypothyroidism.
Acknowledgement
The author would like to thank all colleagues from the Department of primary care for helping in data collection.
Conflict of interests
The authors declare no conflict of interests.
There are no references