Journal Name: International Journal of Immunological Research and Reviews
Article Type: Research
Received date: 16 August, 2019
Accepted date: 17 September, 2019
Published date: 24 September, 2019
Citation: Aref MI, Metwally MM, Abomohamed NM, Mosa MF, Wahab AEAE (2019) Autophage Activity Assessment in Response to Hyperlipidemic Stats in Rheumatoid Patients with Anti-rheumatoid Drugs. Int J Immunol Res Rev Vol: 1, Issu: 1 (01-05).
Copyright: © 2019 Aref MI. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Introduction
Background: Dyslipidemia is the common complication in rheumatoid arthritis R.A patient, subsequently increased cardio vascular diseases CVD risk. Dyslipidemia is the net result between positive intake of lipids and clearance by autophage cells.
Objective: The aim of this work was to evaluate the effect of autophages function as clearance of dyslipidemia in active rheumatoid arthritis (RA) treatment.
Patients and methods: This study was carried out at Agouza Police Hospitals. Analysis of data from one hundred and twenty individuals admitted whose age ranging between 40-65 years for healthy and patient with Rheumatoid arthritis attending the outpatient clinic and the inpatient department of Rheumatology, and divided into four groups:
Group 1: Thirty healthy volunteers as a negative control.
Group 2: Thirty patients early discovered without medication had either moderate or high disease activity (DAS-28 >3.2) as a positive control.
Group 3: Thirty patients treated by combined therapy (immune suppressive+immune-stimulant) were going in remission or had low disease activity (DAS-28<3.2).
Group 4: Thirty patients treated by an immune suppressive medication (methotrexate) were going in remission, or had low disease activity (DAS-28<3.2).
Results: There was a significant increase of cholesterol in patients treated groups 2, 3, 4, in comparison to negative control group. There was significant increase of LDL in positive control and immune suppressive medication groups while decreased in combination therapy group. which showed significant increase in HDL. There was significant increase of disease activity (DAS-28) in groups positive control and patients treated groups. The auto phage function showed significant increased in all groups and this could be secondary increase of phagocytosis through the action of cytokines and defect of digestion secondary to therapeutic drugs.
Conclusion: Methotrexate, one of the essentially used immunosuppressive drugs in rheumatoid arthritis (RA), is completely responsible for dyslipidemia.
Keywords
Autopage Function, Clearance Hyperlipidemia, Concern of Anti-Rheumatoid drugs.
Introduction
Background: Dyslipidemia is the common complication in rheumatoid arthritis R.A patient, subsequently increased cardio vascular diseases CVD risk. Dyslipidemia is the net result between positive intake of lipids and clearance by autophage cells.
Objective: The aim of this work was to evaluate the effect of autophages function as clearance of dyslipidemia in active rheumatoid arthritis (RA) treatment.
Patients and methods: This study was carried out at Agouza Police Hospitals. Analysis of data from one hundred and twenty individuals admitted whose age ranging between 40-65 years for healthy and patient with Rheumatoid arthritis attending the outpatient clinic and the inpatient department of Rheumatology, and divided into four groups:
Group 1: Thirty healthy volunteers as a negative control.
Group 2: Thirty patients early discovered without medication had either moderate or high disease activity (DAS-28 >3.2) as a positive control.
Group 3: Thirty patients treated by combined therapy (immune suppressive+immune-stimulant) were going in remission or had low disease activity (DAS-28<3.2).
Group 4: Thirty patients treated by an immune suppressive medication (methotrexate) were going in remission, or had low disease activity (DAS-28<3.2).
Results: There was a significant increase of cholesterol in patients treated groups 2, 3, 4, in comparison to negative control group. There was significant increase of LDL in positive control and immune suppressive medication groups while decreased in combination therapy group. which showed significant increase in HDL. There was significant increase of disease activity (DAS-28) in groups positive control and patients treated groups. The auto phage function showed significant increased in all groups and this could be secondary increase of phagocytosis through the action of cytokines and defect of digestion secondary to therapeutic drugs.
Conclusion: Methotrexate, one of the essentially used immunosuppressive drugs in rheumatoid arthritis (RA), is completely responsible for dyslipidemia.
Keywords
Autopage Function, Clearance Hyperlipidemia, Concern of Anti-Rheumatoid drugs.
Introduction
Rheumatoid arthritis (RA) is a chronic autoimmune disease with joint inflammation and autoantibody production. RA remains a heterogeneous syndrome in terms of clinical expression and long-term course, and different pathogenic pathways are likely to be differently activated in different patients or at least in different phases of the disease. The relative contribution of B lymphocytes appears greatly variable, as inferred at least by the existence of a seropositive and a zero-negative subtype of RA [1].
Traditional cardiovascular risk factors in RA include, lipids. RA is associated with an adverse lipid profile that is conventionally accepted as a risk factor for cardiovascular disease [4]. Lipid profile can be improved to an extent that is clinically meaningful by effectively treating RA without using a lipid lowering agent [5].
Aim of the Work
The aim of this work was to evaluate the effect of autophagias function as clearance of dyslipidemia in two different lines of rheumatoid arthritis treatment.
Subjects and Methods
This study was carried out at of El-Agoza Police Hospitals. Analysis of data from one hundred and twenty individuals whom age ranging between 40-65 years, 84 females (80%), and 36 males (20%). This group included healthy volunteer and patient with Rheumatoid arthritis attending the outpatient clinic and the inpatient department of Rheumatology, Rehabilitation and physical medicine were divided into 4 groups:
Group 1: Thirty healthy volunteers as a negative control.
Group 2: Thirty patients early discovered without medication, and had either moderate or high disease activity (DAS-28>3.2) as positive control.
Group 3: Thirty patients treated by combined therapy of (immune suppressive+ immune-stimulant) and were going in remission or had low disease activity (DAS-28<3.2).
Group 4: Thirty patients treated by immune suppressive medication (methotrexate) and in remission or had low disease activity (DAS-28<3.2).
All patients included in the study met the American College of Rheumatology (ACR) revised criteria for classification of rheumatoid arthritis [6].
Exclusion criteria
Patients and control were excluded from the study when they had
- Tobacco smoking.
- Chronic diseases including hypertension, diabetes or hypercholesterolemia.
Ethical considerations
An informed consent was taken from patients included in the study, and it was approved by the ethical committee of Faculty of Medicine Al-Azhar University.
Classification criteria for RA score-based algorithm: add score of categories A-D; a score of ≥ 6/10 is needed for classification of a patient as having definite RA [6].
Laboratory Investigations
- Erythrocyte sedimentation rate (ESR).
- C-reactive protein (CRP) by auto analyzer, ARCHITECT ER-200.
- Rheumatoid Factor by auto analyzer, ARCHITECT ER- 200.
- Anti-cyclic citrullinated peptide (ACCP) antibodies by ELISA.
- Lipid profile: including total serum cholesterol (SC), low density lipoprotein-cholesterol (LDL-C), high-density lipoprotein-cholesterol (HDL-C) and serum triglyceride level were carried out on auto analyzer Beckman coulter AU 480.
- Estimation of Neutrophil lipid phagocytes by Sudan black stain: The percentage of active engulfing lipids in hundred cells will be calculated digitally.
Method and Principle of Estimation
Principle: Sudan Black stain is slightly basic dye and will combine with acidic groups in compound lipids, and phospholipid [7].
Reagent: Sudan black solution (1 mg per 100 mL buffer phosphate saline). Calcium gluconate 1% was to enhance the penetration of Sudan black into lipid containing cells.
Method:
- The plasma rich cells were used for staining and calculation
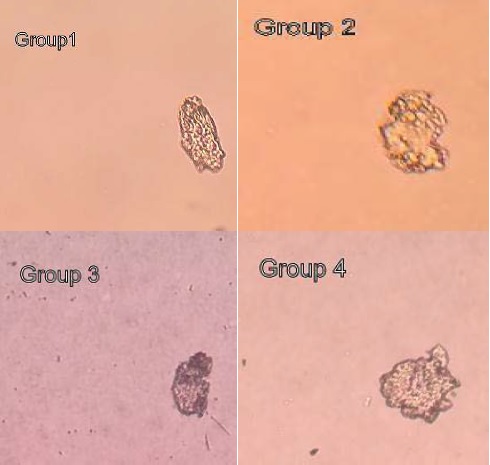
- The stain warmed into 37 °C before use it. Random hundred stained cells of each group were photographed and processing into image Photoshop program (Image j Photoshop program).
- The amount of fat inside the selected cells will calculated by the Image j program. (figure 1)
Figure 1: 7- ASCVD (Atherosclerotic cardiovascular disease 2013) risk calculator from AHA/ACC: Determines 10-year risk of heart disease or stroke.
Statistical Analysis
Recorded data were analyzed using the statistical package for social 0sciences, version 20.0 (SPSS Inc., Chicago, Illinois, USA). Quantitative data were expressed as mean ± standard deviation (SD). Qualitative data were expressed as frequency and percentage.
The following tests were done
- Independent-samples t-test of significance was used when comparing between two means.
The confidence interval was set to 95% and the margin of error accepted was set to 5%. P-value <0.05 was considered significant.
Results
Table 1 showed a significant increased for CRP in (group 2, 3) compared group 1 while not significant in group 4 compared group 1. ESR, Anti CCP and DAS-28 showed significant increase in groups 2, 3, 4 compared to group 1. RF showed significant increase in groups 2, and 4 compared to (group 1).
Table 1: The statistical analysis of CRP, ESR, RF, anti-CCP and DAS-28.
| Groups | Mean | STD | T-Test | P Value | |
|---|---|---|---|---|---|
| Group 1 | 4.734 | 3.90062 | |||
| CRP | Group 2 | 30.59 | 27.30476 | 3.873 | <0.01 |
| Group 3 | 8.402 | 10.23539 | 3.509 | <0.01 | |
| Group 4 | 5.57 | 3.5343 | 0.6756 | >0.05 | |
| Group 1 | 9.7 | 28.769 | |||
| ESR | Group 2 | 18.7 | 7.6891 | 3.873 | <0.01 |
| Group 3 | 12.6 | 4.42719 | 3.509 | <0.01 | |
| Group 4 | 12.2 | 4.56557 | 3.509 | <0.01 | |
| Group 1 | 10.129 | 7.49566 | |||
| RF | Group 2 | 80.77 | 99.10159 | 3.873 | <0.01 |
| Group 3 | 20.392 | 17.94189 | 1.54898 | >0.05 | |
| Group 4 | 31.718 | 22.83834 | 3.509 | <0.01 | |
| Group 1 | 0.709 | 0.43093 | |||
| Anti-CCP | Group 2 | 68.801 | 79.48804 | 3.873 | <0.01 |
| Group 3 | 29.3 | 28.09527 | 3.21466 | <0.01 | |
| Group 4 | 32.31 | 61.54356 | 3.509 | <0.01 | |
| Group 1 | 0 | 0 | |||
| DAS-28 | Group 2 | 3.74 | 0.22705 | 3.74 | <0.01 |
| Group 3 | 2.15 | 0.65532 | 2.15 | <0.01 | |
| Group 4 | 2.34 | 0.57388 | 3.509 | <0.01 |
Table 2 showed a significant increase of cholesterol in (groups 2-4) compared to group1. The same of HDL-C. While LDL-C increased in groups 2 and 4. compared to group 1. Triglycerides increased in (groups 2, 3)
Table 2: The statistical analysis of cholesterol, LDL-C, HDL-C, triglycerides, autophage index and risk of CVD.
| Group | Mean | STD | T-Test | P Value | |
|---|---|---|---|---|---|
| Group 1 | 181.7 | 31.62998 | |||
| Cholesterol | Group 2 | 222.2 | 50.79764 | 3.509 | <0.01 |
| Group 3 | 219.2 | 46.20197 | 2.4347 | <0.05 | |
| Group 4 | 242.5 | 74.10091 | 3.874 | <0.01 | |
| Group 1 | 96.06 | 37.33356 | |||
| LDL-C | Group 2 | 125 | 52.957 | 3.609 | <0.01 |
| Group 3 | 122.3 | 41.60141 | 0.1105 | >0.05 | |
| Group 4 | 142.0399 | 63.49979 | 3.873 | <0.01 | |
| Group 1 | 48.9 | 14.40255 | |||
| HDL-C | Group 2 | 45.4 | 11.30585 | 3.5 | <0.05 |
| Group 3 | 60 | 16.88523 | 2.903 | <0.05 | |
| Group 4 | 41.6 | 7.29079 | 1.509 | <0.05 | |
| Group 1 | 164.12 | 92.37 | |||
| TGs | Group 2 | 248.5 | 89.64 | 3.446 | <0.01 |
| Group 3 | 207.2 | 52.75 | 3.509 | <0.01 | |
| Group 4 | 216.1 | 70.73 | 0.6756 | >0.05 | |
| Group 1 | 154.9 | 28.769 | |||
| Autophage index | Group 2 | 154.7 | 34.7916 | 2.903 | <0.01 |
| Group 3 | 189 | 28.06738 | 2.903 | <0.01 | |
| Group 4 | 225.5 | 15.11622 | 3.509 | <0.01 | |
| Group 1 | 2.24 | 2.188 | |||
| Risk of CVD | Group 2 | 2.63 | 1.599 | 2.772 | <0.01 |
| Group 3 | 6.18 | 3.473 | 3.509 | <0.01 | |
| Group 4 | 10.25 | 8.5 | 3.873 | < 0.01 |
The auto phages lipids and cardio-vascular disease (CVD) increased in (groups 2-.4) compared to (group 1).
Discussion
The present study was done on 120 individuals 90 of them have rheumatoid arthritis and 30 were apparent healthy control. Blood tests were done for 4 groups including ESR, CRP, RF and anti-CCP as markers of disease activity and total cholesterol, tri glycerides, HDL, and LDL as a marker of dyslipidemia. The majority of the patients were females and this was attributed to the disease prevalence. In our study, patients with active RA showed dyslipidemia in patients’ groups and had a more marked atherogenic lipid profile compared with the negative control group. This atherogenic lipid profile include significant increased total cholesterol and LDL except (group 3).
The statistical results showed hypercholesteremia in patients with active disease either medication or not. Cholesterol was significant in all groups. These results agreed with Jafri et al. [8] who found that patients with RA exhibited higher TC, LDL, HDL and TG compared to controls. HDL was not significant to all groups except in combined therapy group 3 was significant increased while LDL was significant decreased in group 3. This result could be explaining the mean balk of cholesterol is HDL and not LDL [5]. The therapeutic effects of hydroxychloroquine as immunoactivities on autophagias could be responsible to reducing LDL-C. while has no effect on HDL This result agreed with Desai et al. [9].
The mean value of TGs in all groups were increased in all patients’ groups. So, RA treatment has no effect on TGs. This result could explain the high risk of CVD in RA. However, this result coincides with Rodríguez-Carrao et al. [10].
ESR, CRP and anti-CCP showed significant increase in positive control group (group 2). This approve the selective patient was in active state while not in treated groups. This was due to the action of therapeutic drugs. The activity of RA disease was due to increased circulating immune-complex, complement and subsequence activation of immunological cells and release of proinflammatory and inflammatory cytokines.
The immune-suppression treated group (group 4) has normal ESR due to the action of methotrexate stopping the inflammatory cytokines. The significant increase of ESR was secondary to increase of fibrinogen and beta 2 micro globulins. Those proteins produced in liver secondary to the action of proinflammatory proteins. Methotrexate has a direct action to stop the release of proinflammatory cytokines (IL6-IL1) [11].
DAS-28 score significantly decreased in treated (groups 3,4) compared to positive control group. Methotrexate therapy with or without hydroxychloroquine had a significant decrease in DAS-28 score. The action of Methotrexate (MTX) is a chemotherapeutic drug that is structurally similar to folic acid. MTX inhibits dihydrofolate reductase, an enzyme that reduces folic acid to tetrahydro folic acid. This inhibition interferes with DNA synthesis and cell reproduction. This could relate to stopping the inflammation by blocks the binding of interleukin 1 beta to the interleukin 1 receptor on target cells [12].
Three forms of autophagy are commonly described: macro autophagy, micro autophagy, and chaperonemediated autophagy (CMA). In macro autophagy, expendable cytoplasmic constituents are targeted and isolated from the rest of the cell within a double-membraned vesicle known as an autophagosome, which, in time, fuses with an available lysosome, bringing its specialty process of waste management and disposal; and eventually the contents of the vesicle (now called an autolysosome) are degraded and recycled [13].
Lipophagy is the degradation of lipids by autophagy, the role of lipophagy, however, remains elusive. In lipophagy the target are lipid structures called lipid droplets , spherical “organelles” with a core of mainly triacylglycerols (TAGs) and a unlayered of phospholipids and membrane proteins. In animal cells the main lipophobic pathway is via the engulfment of lipophagy by the phagophore, macro autophagy. Lipophagy was first discovered in mice and published 2009 [14,15].
Autopage is a phagocytic cell supposed to be responsible for clearance of dyslipidemia. This action done by lipophage. So, as external factors regulate its phagocytic function. Inflammatory cytokines which are present in active stage in RA help for phagocytosis and digestion [12].
In immune suppressive drugs as methotrexate suppress phagocytosis. The net results patient autophagy facing balance between immune-stimulant inflammatory mediators and immunosuppressive drugs.
From our results the lipid content in autophagy was significant increase in group 2,3,4.
Conclusion
Methotrexate is immunosuppressive drug is responsible for dyslipidemia.
Recommendations
a) We advise the R.A patient to take immune-stimulant in combination with methotrexate or anti-lipidemic drugs used in combination with methotrexate in R.A patient especially in active state.
b) Anti-lipidemic drugs should be used in combination immunosuppressive drugs especially in active RA disease.
There are no references