Journal Name: J Clinical Pharmacy
Article Type: Review
Received date: 22/5/19
Accepted date: 30 May, 2019
Published date: 2019-07-09
Citation: Santalo O (2019) A Practice Model for Twenty-Four Hour Code Coverage with Pharmacy Residents. J Clin Pharm Vol: 1, Issu: 1 (01-04).
Copyright: © 2019 Santalo O. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Introduction: Pharmacists who are integrated into cardiac arrest teams show an improved quality in ACLS documentation and adherence to ACLS guidelines resulting in reductions in patient mortality. American Society of Health System Pharmacy recommends how hospitals should continue their services for 24 hours. An institution wished to continue pharmacy medical emergency coverage for 24 hours utilizing its pharmacy residents. The purpose of this study is to evaluate the code coverage practice model with pharmacy residents.
Methods: This was a prospective, IRB approved for quality improvement, observational cohort study at a community tertiary care center. Primary outcome was amount of codes versus day and overnight shift, the locations of the code during the overnight shift, and the times of the codes during the overnight shift.
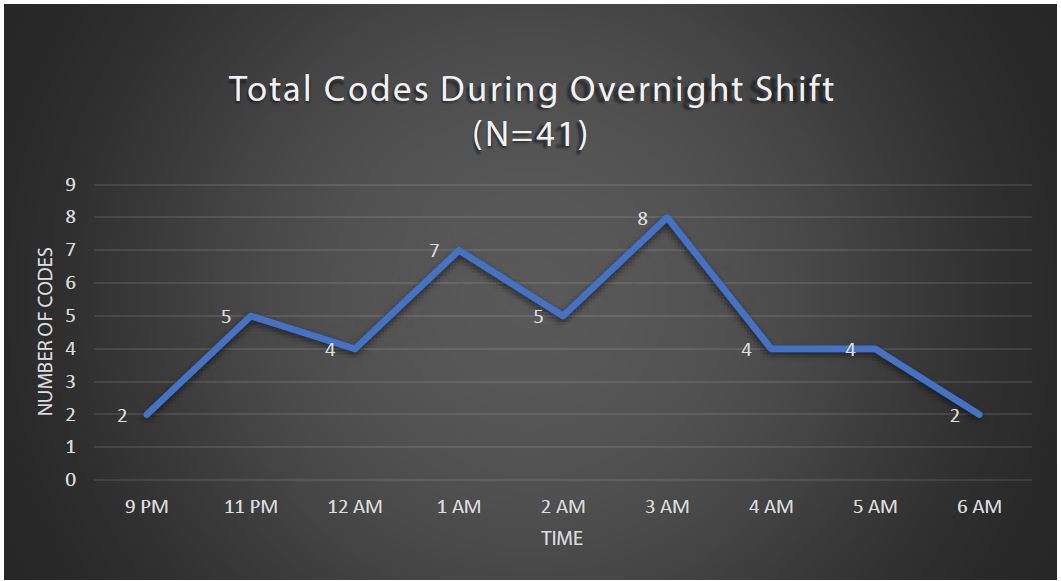
Results: 41 out of the 79 codes were called during the overnight shift over a seven-week span. During this period, the highest incidences of codes took place from 0300-0400 and the most codes during an overnight shift was four.
Conclusion: With 51% of the cardiac resuscitation responses called during the overnight shift, the two overnight resident model was able to provide a continuation of pharmaceutical care for 24 hours. With only one occurrence where codes took place simultaneously, the institution will decrease the overnight resident model down to one resident. Further studies are needed to assess the impact of the overnight shift on the resident’s physical and mental health.
Keywords
ACLS guidelines; Pharmacists; Mortality Rate.
Abstract
Introduction: Pharmacists who are integrated into cardiac arrest teams show an improved quality in ACLS documentation and adherence to ACLS guidelines resulting in reductions in patient mortality. American Society of Health System Pharmacy recommends how hospitals should continue their services for 24 hours. An institution wished to continue pharmacy medical emergency coverage for 24 hours utilizing its pharmacy residents. The purpose of this study is to evaluate the code coverage practice model with pharmacy residents.
Methods: This was a prospective, IRB approved for quality improvement, observational cohort study at a community tertiary care center. Primary outcome was amount of codes versus day and overnight shift, the locations of the code during the overnight shift, and the times of the codes during the overnight shift.
Results: 41 out of the 79 codes were called during the overnight shift over a seven-week span. During this period, the highest incidences of codes took place from 0300-0400 and the most codes during an overnight shift was four.
Conclusion: With 51% of the cardiac resuscitation responses called during the overnight shift, the two overnight resident model was able to provide a continuation of pharmaceutical care for 24 hours. With only one occurrence where codes took place simultaneously, the institution will decrease the overnight resident model down to one resident. Further studies are needed to assess the impact of the overnight shift on the resident’s physical and mental health.
Keywords
ACLS guidelines; Pharmacists; Mortality Rate.
Introduction
About 2,09,000 patients are treated annually for in-hospital cardiac arrest [1]. A cardiac arrest is a circulatory collapse with cessation of cardiac function that is either restored by resuscitative efforts. Survival to hospital discharge ranges from 22.3% to 25.5% among patients who received resuscitative efforts. Coronary artery disease, non-ischemic cardiomyopathies, cardiac conduction diseases, electrolyte disorders, strokes, hemodynamic instabilities, and medications can cause cardiac arrest. Major complications of cardiac arrest are sudden death and irreversible neurological injury.
The way hospitals approach inpatient cardiac arrests are through medical emergency teams (METs) or rapid response teams (RRTs) [2]. These teams consist of interdisciplinary combinations of physicians, nurses, respiratory therapists, and pharmacists [3]. The traditional roles of pharmacists on cardiac arrest teams include preparing intravenous medication admixtures needed for resuscitation, identify and treat medication-related problems. Pharmacists who are integrated into cardiac arrest teams show an improved quality in ACLS documentation and adherence to ACLS guidelines resulting in reductions in patient mortality. The presence of pharmacists on cardiac arrest teams show a significant improvement in the documentation and compliance with ACLS algorithms. With the addition of a pharmacist on the team, nurses can concentrate on preparing medication and retrieving other supplies from the resuscitation cart leading to minimized preparation delays and errors that could occur while performing multiple tasks.
Emergency Department (ED) pharmacists have demonstrated multiple improvements on the team such as providing a positive impact on patient-specific outcome measures, timely medication administration, optimization of therapy, medication safety, and cost of care [3]. According to Farmer et al., there is published data to demonstrate the presence of an ED pharmacist can reduce time to antibiotic administration for patients with sepsis, time to first analgesic in trauma patients, time to sedation and analgesia after rapid sequence intubation, time to thrombolysis for patients with acute ischemic stroke, and door-to-balloon time for patients with acute myocardial infarction [4].
Training for pharmacist may require programs that incorporate pharmacists onto the cardiac arrest teams in the role of documenter and pharmacotherapy consultant [5]. Researchers evaluated changes in documentation quality, ACLS compliance, survival, and other quality metrics after program implementation. Formed a core group of 12 pharmacists including critical care pharmacists, and two post-graduate year 2 (PGY-2) pharmacy specialty residents (specializing in critical care and solid organ transplantation). The pilot study did not require ACLS certification through the AHA. The lead pharmacist and PGY-2 resident obtained it voluntarily [5]. Extensive training took place where guest pharmacists volunteered their time to provide lectures to orient pharmacists in training for the critical care team.
Integrating Pharmacy Residents into Cardiac Arrest Teams
American Society of Health System Pharmacy recommends how hospitals should continue their services for 24 hours [6]. An institution wished to continue pharmacy medical emergency coverage for 24 hours. The institution wished to utilize its pharmacy residents (combined PGY- 1s and PGY-2s) that are responsible for attending codes. This was to ensure daily coverage and also helped with drug shortages. The model previously had residents cover the day and evening shift. The pharmacy resident medical emergency model had two residents on each shift. Shifts were broken down into day shift which was from 0600 until 1500, evening shift which was 1500 until 2100, and overnight coverage which was from 2100 until 0700 the next day. During the day shift two residents are on coverage while on their respective rotations. The two residents in the evening were on code coverage while executing their longitudinal evening staffing requirement which was supported by other pharmacy staff if they had to attend codes. The overnight shift had one pharmacy resident in the emergency department and the other in one of the Intensive Care Units (ICUs). The residents went to all of the called code blues throughout the entire hospital.
The purpose of this study is to evaluate the code coverage practice model with pharmacy residents at this institution. Pharmacy leaders wanted to ensure that the services are being provided continuously over 24 hours. The leaders also wanted a practice model that would be sustainable for years to come.
Methods
The resident code coverage model, codes attended were confirmed by the code pager and resident documenting their interventions during codes. This was a prospective, IRB approved for quality improvement, observational cohort study at a community tertiary care center. Data collection from 2/12/2018 to 4/1/2018. Data points collected were the amount of codes per shift, start time of code, end time of code, location of code, overlapping codes, and patients achieved ROSC. Primary outcome was amount of codes versus day and overnight shift, the locations of the code during the overnight shift, and the times of the codes during the overnight shift. Secondary outcomes were percent of patients that achieved ROSC and the average time spent at codes. T-test was used for all continuous variables, and Fisher’s exact test was used for categorical variables. All P values were two-tailed, and α < 0.05 was set as the level of statistical significance for all tests. All analyses were performed by using Stata version 14 (Stata Corp.,2015).
Results
There was a total of 79 code cardiac resuscitation responses. Results of the study are reflected on Table 1 along with secondary outcomes. 41 of them were called during the overnight shift over a seven-week span. 21 of them were in the critical care and emergency department division. Nine out of the 21 codes were in the hospital’s multi-system intensive care unit. During this period, the highest incidences of codes took place from 0300-0400 shown in Figure 1. The most codes during an overnight shift was four. Sunday, Monday, and Tuesday were the busiest days out of the week for overnight codes with Friday being the least. 56.1% of the patients achieved ROSC during the overnight shift.
Discussion
Overnight resident model
The residents had a hierarchy of responsibilities during their overnight shift. The first responsibility is to attend any code blues via pager or overhead. The second task was to handle any consults that were passed off or new pharmacy consults during their shift. The third responsibility was to take any drug information questions. It was optional for the resident to aid the overnight team with order entry tasks. Residents were to arrive at 2100 and their shift ended at 0700. “Calling the code”, performing compressions, drug preparation, note taking, or retrieving medications or drips that had to come from the inpatient pharmacy were the roles of these pharmacy residents.
There were ten more overnight codes than day time code blues with 41 versus 31 respectively. The location of the codes was primarily in the emergency department or intensive care units. An example of “other location” in Table 1 is a hallway or radiology department. During the overnight shift, 48.8% of the overnight paged code blues were between 0100 to 0400. Patient achieved ROSC in over half of the codes attended. The average time spent at each code was 33 minutes. This study period was seven weeks and there were 22 days of no overnight code responses called and the most codes during the overnight shift was four. There were situations were ROSC was achieved but the patient shortly went back and coded again without a page or announcement.
Figure 1:Total codes during overnight shift.
Table 1:
| Primary Outcome (N) | N (%) | P value | |
|---|---|---|---|
| Codes per shift (79) | Day | 31 (39.2) | 0.38 |
| Evening | 7 (8.9) | ||
| Overnight | 41 (51.9) | ||
| Overnight Location (41) | ED/ICU | 21 (51.2) | < 0.01 |
| Overnight Code Times (41) | 2100-0100 | 13 (31.7) | 0.0179 |
| 0100-0400 | 20 (48.8) | ||
| 0400-0700 | 8 (19.5) | ||
| Secondary outcomes (N) | N (%) | |
|---|---|---|
| Patient’s achieved ROSC (41) | 23 (56.1) | |
| Average time spent per overnight code (41) | 33 minutes* | |
| Days per overnight code (41) | Sunday | 9 (21.9) |
| Monday | 8 (19.5) | |
| Tuesday | 8 (19.5) | |
| Wednesday | 4 (9.75) | |
| Thursday | 4 (9.75) | |
| Friday | 3 (7.3) | |
| Saturday | 5 (12.3) | |
| Days without overnight codes (48) | 22 (45.8) | |
| Most overnight codes per shift | 4* | |
| *Unable to calculate percentage | ||
Residents were able to attend all of the codes that were paged. Only one code overlapped with one another. The total number of overnight code blues may have been falsely lower. Code blues in the ED did not get any pages but did have overhead announces that were only in the ED. Therefore, if the resident was not in the ED, they would not have heard nor responded to the code. Medical reds and yellows were not documented since code blues were only documented. For the other locations, intensive care units did not announce nor call every rapid response. The duration of the observational study which was seven weeks, code blues in the ED and ICU were not always announced, medical reds and yellows could have been code blues, unable to document the roles or physical impact that the residents had on the codes were the limitations of this study.
Limitations
Resident code documentation, pager service, and code calling were limitations to this study. Residents may have or have not accurately documented the time of code or interventions made. There were occasions where the codes were announced on the overhead public address system instead of the pager. This might have caused confusion if the residents did not listen for the code or if they have solely relied on the pager. Lastly, in the ICUs and the ED, not every code was announced nor paged. The resident would have to be present in those areas to be able to attend those codes.
Conclusion
With 51% of the cardiac resuscitation responses called during the overnight shift, the two overnight resident model was able to provide a continuation of pharmaceutical care for 24 hours. With only one occurrence where codes took place simultaneously, the institution will decrease the overnight resident model down to one resident the following year. Further studies are needed to assess the impact of the overnight shift on the resident’s physical and mental health.
Yousuf O, Chrispin J, Tomaselli GF, Berger RD (2015) Clinical management and prevention of sudden cardiac death. Circ Res 116: 2020-2040. [ Ref ]
Kronick SL, Kurz MC, Lin S (2015) Part 4: Systems of Care and Continuous Quality Improvement: 2015 American Heart Association Guidelines Update for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 132: S397-S413. [ Ref ]
Edelson DP, Yuen TC, Mancini ME (2014) Hospital cardiac arrest resuscitation practice in the United States: a nationally representative survey. J Hosp Med 9: 353-357. [ Ref ]
Farmer BM, Hayes BD, Rao R, Farrell N, Nelson L (2018) The Role of Clinical Pharmacists in the Emergency Department. J Med Toxicol 14: 114-116. [ Ref ]
Heavner MS, Rouse GE, Lemieux SM (2017) Experience with integrating pharmacist documenters on cardiac arrest teams to improve quality. Journal of the American Pharmacists Association 58: 311-317. [ Ref ]
American Society of Health-System Pharmacists (2013) ASHP guidelines: minimum standard for pharmacies in hospitals. Am J Health-Syst Pharm 70: 1619-1630. [ Ref ]