Journal Name: Journal of Applied Microbiological Research
Article Type: Research
Received date: 04 March, 2022
Accepted date: 14 April, 2022
Published date: 21 April, 2022
Citation: Zeru T, Endalamaw D, Taye B (2022) 5-Year (2014-2018) Trends of Visceral Leishmaniasis in Amhara Region, North West Ethiopia. J Appl Microb Res. Vol: 5 Issu: 1 (08-13).
Copyright: © 2022 Zeru T et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Background: Visceral leishmaniasis (VL; also known as kala-azar), caused by protozoan parasites of the Leishmania donovani complex, is a major public health problem in Ethiopia. Despite VL is endemic in the lowlands of Amhara region, and is almost always fatal if left untreated, there is no report that shows regional wide trends of VL cases over years of period.
Method: A retrospective data to determine cumulative number of cases, trends in incidence and mortality rate, and geographic coverage of VL over 5 years’ period (2014-2018) was obtained from Health Management Information System (HMIS) database owned by Amhara Regional Health Bureau Leishmaniasis Service. SPSS version 20 was used to analyze the data.
Results: Over 5 years of period (2014-2108), a total of 5,624 VL cases were registered across all zones of Amhara Region. The majority of these VL patients (90%) were adult while, men being the most affected ones (87%) than women (13%). High incidence rate of VL with a trend of steady increment over the 5 years’ period was observed. The highest fatality rates were recorded in North Gondar zone and No fatality rates were recorded in North Wollo, South wollo, North Shoa, East gojam and West gojam respectively. With regard to health service attendance, 58% of VL cases were register outpatient attendees.
Conclusion: VL was reported in almost all parts of the Amhara region posing a serious challenge on provision of diagnosis and treatment services, especially in areas where the disease has never been reported before. Additionally, adult men representing the working group of the community were the most sufferers of VL, suggesting the bad consequence on the socioeconomy of the region. To overcome those challenges associated with VL, training health care providers on prompt diagnosis and clinical management of VL along with other strategies is imperative.
Keywords
Viscera Leishmaniasis (VL), Trends, Amhara, Ethiopia.
Abstract
Background: Visceral leishmaniasis (VL; also known as kala-azar), caused by protozoan parasites of the Leishmania donovani complex, is a major public health problem in Ethiopia. Despite VL is endemic in the lowlands of Amhara region, and is almost always fatal if left untreated, there is no report that shows regional wide trends of VL cases over years of period.
Method: A retrospective data to determine cumulative number of cases, trends in incidence and mortality rate, and geographic coverage of VL over 5 years’ period (2014-2018) was obtained from Health Management Information System (HMIS) database owned by Amhara Regional Health Bureau Leishmaniasis Service. SPSS version 20 was used to analyze the data.
Results: Over 5 years of period (2014-2108), a total of 5,624 VL cases were registered across all zones of Amhara Region. The majority of these VL patients (90%) were adult while, men being the most affected ones (87%) than women (13%). High incidence rate of VL with a trend of steady increment over the 5 years’ period was observed. The highest fatality rates were recorded in North Gondar zone and No fatality rates were recorded in North Wollo, South wollo, North Shoa, East gojam and West gojam respectively. With regard to health service attendance, 58% of VL cases were register outpatient attendees.
Conclusion: VL was reported in almost all parts of the Amhara region posing a serious challenge on provision of diagnosis and treatment services, especially in areas where the disease has never been reported before. Additionally, adult men representing the working group of the community were the most sufferers of VL, suggesting the bad consequence on the socioeconomy of the region. To overcome those challenges associated with VL, training health care providers on prompt diagnosis and clinical management of VL along with other strategies is imperative.
Keywords
Viscera Leishmaniasis (VL), Trends, Amhara, Ethiopia.
Background
Depending on the parasite species and the immunogenic background of the infected person, infections with protozoan parasites of the genus Leishmania can cause a broad spectrum of syndromes, ranging from selfhealing cutaneous leishmaniasis to the most fatal Viscera Leishmaniasis (VL; kala-azar). Leishmaniasis, including VL is transmitted from person to person by the bite of infected phlebotomies sand flies [1].
Globally an estimated 500,000–1,000,000 new cases of Leishmaniasis occur annually but only a small fraction of these cases (19%–37%), are actually reported to health authorities [2-4].VL alone, is responsible for 50,000 deaths and the loss of over 2.3 million of disability-adjusted life years annually.
In Africa Continent, Ethiopia is the second most affected country by VL epidemics next to Sudan with an estimated of 4000 new cases each year. Over 60% of these cases are associated with HIV/AIDS. It is endemic in lowland arid areas bordering Sudan in north, and bordering Kenya in south but recently has spread to become endemic in many parts of the country.
In northwest Ethiopia, Humera, Matama, Blessa, Libo Kemkem districts are known to be major epicentrics of VL epidemics. In this part of Ethiopia, epidemics are often associated with migration and movement of non-immune highlander seasonal workers into the same growing VL endemic farmlands. During post-harvest season, these migrant seasonal workers often return to their original places probably being infected and might later develop the clinical symptoms and signs following the 2 to 6 months of incubation period depending on the nutritional and immunological status of the infected individuals. The classical symptoms of VL include fever, pallor, food refusal, weight loss, vomiting, hepatosplenomegaly, ecchymosis and gingival bleeding [5-8].
Fever is usually associated with rigor and chills and can be intermittent. Fatigue and weakness are worsened by anemia, which is caused by the persistent inflammatory state, hypersplenism (the peripheral destruction of erythrocytes in the enlarged spleen). These clinical manifestations of VL appeared to be non-specific, often confused with other febrile illness such as malaria. This makes diagnosis VL very complicated especially in health facilities located in non-VL endemic areas and/or the health workers are less experienced inexperienced to diagnosis and manage VL patients.
Despite VL is endemic in the lowlands of Amhara region and increasingly spreading to previously non- endemic highland areas, there is no report that shows regional wide trends of VL cases over years of period. We therefore used 5-years data obtained from Health Management Information System (HMIS) database managed by Amhara Regional Health Bureau Leishmaniasis Service in order to investigate cumulative number of cases, trends in incidence and mortality rate, and geographic coverage of VL from 2014 to 2018.
Methods
Study area and setting
The study was conducted in Amhara regional state which is one of the nine regional states of Federal Democratic Republic of Ethiopia. The State shares common borders with the state of Tigray in the north, afar in the east, Oromiya in the south, Benishangul/Gumuz in the south west, and the Republic of Sudan in the west. The climatic condition of the region is divided in to Kola (31%), Woyna-Dga (44%) and Dega (25%).
Study design
This was a retrospective HMIS report analysis of Visceral Leishmaniasis (VL) service results of Amhara regional health bureau. All patients with HMIS report of diagnosis as VL from 2014 to Aug 2018 were included
Sample size and sampling
All HMIS regional Visceral Leishmaniasis data were included from 2014 to 2018. During the reporting period 2641 patients were involved in the study.
Data management and analysis
Data was collected from the HMIS report of Amhara regional state health bureau. It was documented in an excel sheet and cross checked for consistency by the investigator. It was transferred to SPSS version 20 finally results were summarized by using frequency table and graph.
Results
The burden of Visceral Leshimaniasis in Amhara region from 2014 to 2018
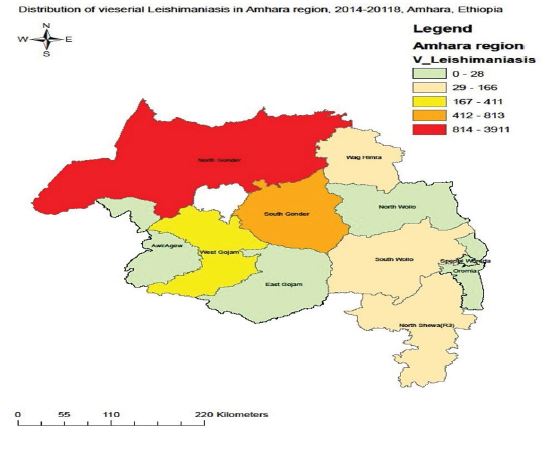
All zones of Amhara region reported 5624 cases of VL cases in the 5 years. Of these, Gondar town and North Gondar zone accounts 70% of the total cases reported. the lowest number cases were reported from East Gojam and Awi zones but no case was reported from Oromia zones of Amhara region (Figure 1). Majority of VL cases (90%) were adults while males account 87% of the cases reported cases. Furthermore 58% of the reported cases were OPD (Table 1).
5 year’s trend of VL
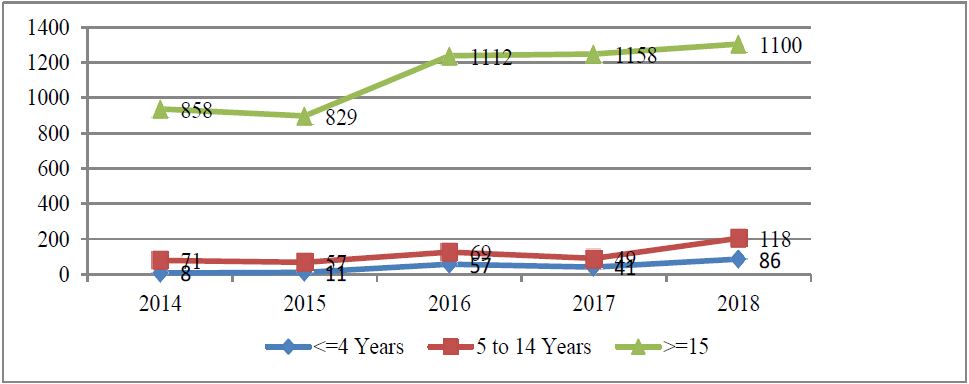
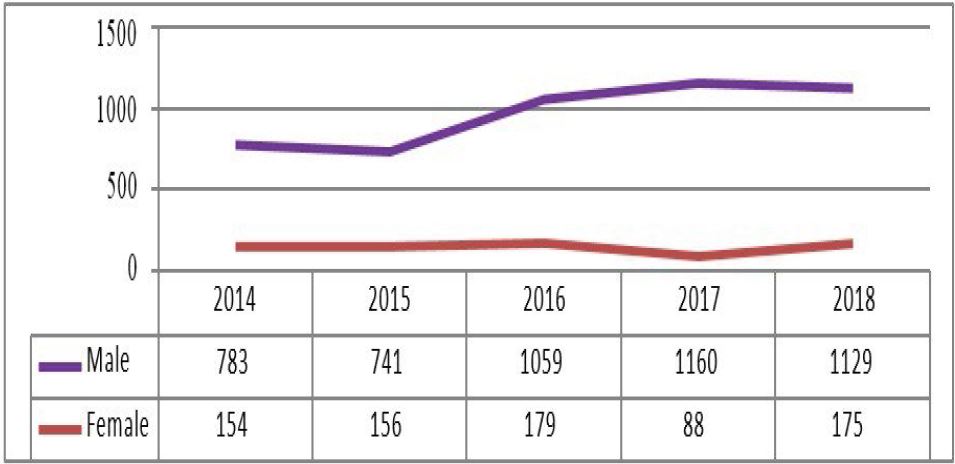
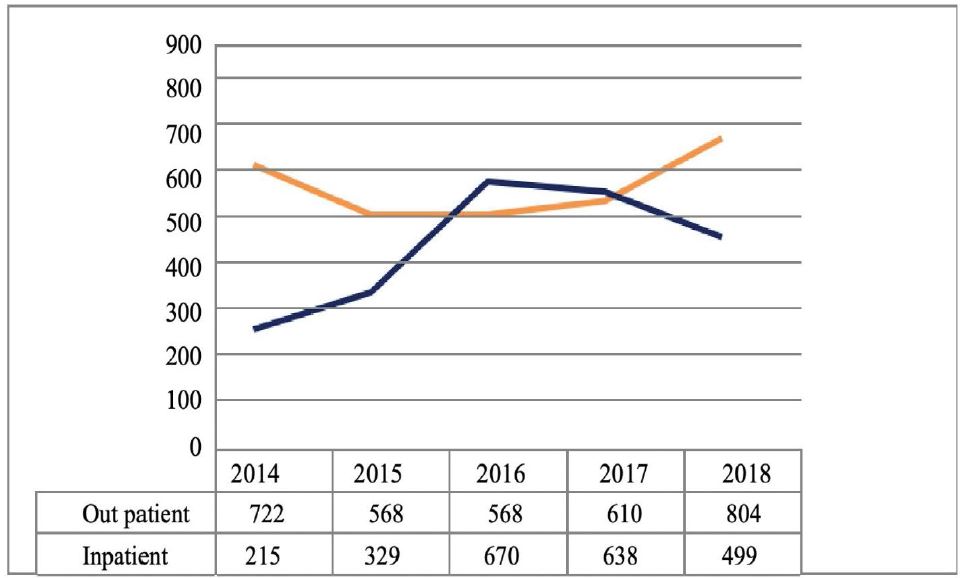
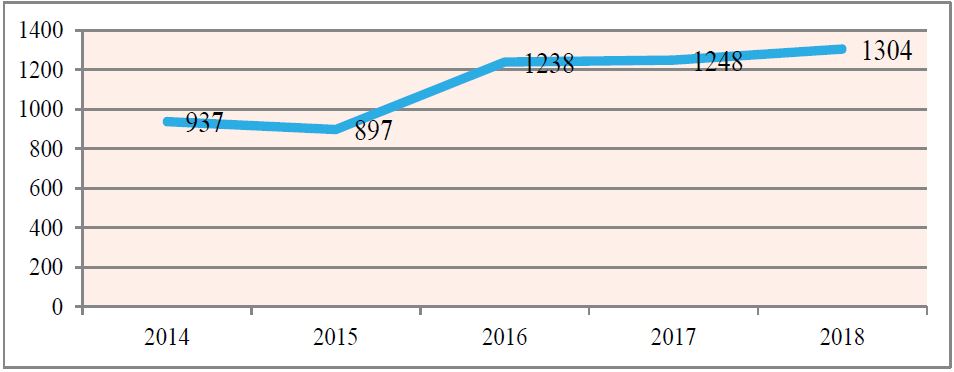
There was a declining trend in Inpatient attendance cases of VL despite increasing outpatient attendance cases was reported, while in the years 2016 and 2017, the declining was stabilizing in both Inpatient and Outpatient attendance cases. The Inpatient attendance magnitude was generally lower and Outpatient attendance cases were higher in 2018 (Figure 2). The trends in males were higher in2016 and 2017 but the trend in females were almost similar within the reporting time despite a decrements was seen in 2017 (Figure 3). In Adult patient the trend report showed that it was increased while age >= 4 and 5 to 14 years almost similar trend (Figure 4). The highest peaks were seen in Gondar town administrations in 5 years followed by North Gondar (Figure 5). Finally trend of VL within the last five years was increased and the highest prevalence was 1304 (23.2%) was found in 2018 and the lowest was found in 2014 (Figure 6).
Discussion
In Ethiopia, Ministry of health estimate, the burden of VL is expected to be between 4500 and 5000 cases (6), however in Amhara region the VL case was from 897 to 1304, this showed that VL cases are higher in the region. The majority (90%) of the VL cases were in the age groups of >=15years but a study done in Addis zemen was from 5-14 years. This might be associated with their daily activities. In the study area, these age group study participants are expected to keep domestic animals, participating in harvesting time who were staying outdoors especially during harvest season and dawns. This may have exposed them to the bite of sandflies.
Figure 1: No of case distribution in Amhara Ethiopia 2014-2018.
Figure 2: Trends of VL cases by Age in Amhara region Ethiopia, 2014-2018.
Figure 3: Trends of VL cases by sex in Amhara region Ethiopia 2014-2018.
Figure 4: Trends of VL cases by zones in Amhara region Ethiopia, 2014-2018.
Figure 5: Trends of VL cases by attendance in Amhara region Ethiopia, 2014-2018.
Males were more affected than females (87% vs.13%). A similar finding was also reported in other studies. This gender difference might be due to differences in outdoor activities between males and females. As indicated in another study, males are more involved in outdoor activities than females in the study area and this may have exposed them more to the bites of sandflies [7-10].
Globally the reported case of VL was decreasing while increasing in potential VL threats countries like Ethiopia which is similar trend with the current study [11].Current data show that the geographic distribution of the Sandfly vector for L. donovani seems to extend from the lower Kola to the Weina Dega ecological zones hence Endemic foci of Visceral Leishmaniasis (VL) in Ethiopia occurs mainly in the Kola agro-ecological zones with recent spread to the Woina dega of Ethiopia which is similar finding with the current study the region [11].
Figure 6: Trends of VL cases by years in Amhara region Ethiopia, 2014-2018.
Table 1: The VL distribution by Age, sex, attendance in Amhara region Ethiopia, 2014-2018.
| Categories | Number of cases (%) | |
|---|---|---|
| Age | <=4 Years | 203 (4%) |
| 5 to 14 Years | 364 (6%) | |
| >=15 Years | 5057 (90%) | |
| Sex | Male | 4872 (87%) |
| Female | 752 (13%) | |
| Attendance | Outpatient attendance | 3732 (58%) |
| Inpatient attendance | 2351 (42%) | |
| Total | 5624 (100%) | |
Conclusion
In Amhara region the trend of Visceral Leishmaniasis has been increased and its distribution was in all parts of the region. Adults were more affected hence it has serious consequences for the region economy growth as well as for the nation in general. Thus, health planners and administrators need to give intensive health education for the community about the control and prevention of VL and proper clinical management for health workers.
Limitation of the Study
This study is limited to the data obtained from the HMIS data, being a health facility secondary data; due to this. To fill all these, there is a need for further community based study with strong design to study geographical distribution, molecular Epidemiology and Drug efficacy, should be needed.
Declarations
Ethics approval and consent to participate
Letters of permissions to get the data was obtained from Amhara regional health bureau.
Consent for publication
Not applicable.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Competing interests
The authors declare that they have no competing interests.
Funding
The authors declare that they did not receive funding for this research.
Authors’ contributions
TZ conceptualized the paper. TZ, performed article search, data extraction, and data analysis. TZ did critical review. TZ produced the first draft of the manuscript. All authors contributed to the interpretation, commented on multiple versions, and approved the final manuscript.
Acknowledgments
The authors would like to acknowledge Amhara regional health bureau for giving the chance to get the data.
Araujo Carreira JC, Machado da silva MAFMMAV (2014) The Geospatial Approach on Eco-Epidemiological Studies of Leishmaniasis. Leishmaniasis -Trends in Epidemiology, Diagnosis and Treatment. [ Ref ]
WHO (2014) Manual for case management of cutaneous leishmaniasis in the WHO Eastern Mediterranean Region. [ Ref ]
Reithinger R, Dujardin JC, Louzir H, Pirmez C, Alexander B, et al. (2007) Cutaneous leishmaniasis. Lancet Infect 7: 581-596. [ Ref ]
Ethiopia Public Health Training Initiative. The Carter Center, the Ethiopia Ministry of Health, and the Ethiopia Ministry of Education Learning module for the Ethiopian Health Center Team on leishmaniasis, 2005. [ Ref ]
Donovan C (1903) A possible cause of kala-azar. Indian Med Gaz 38: 478. [ Ref ]
FMOH Ethiopia (2006) Visceral Leishmaniasis: Diagnosis & Treatment Guideline for Health Workers in Ethiopia, FMOH Ethiopia, AddisAbaba, Ethiopia. [ Ref ]
Bashaye S, Nombela N, Argaw D, Mulugeta A, Herrero M, et al. (2009) Risk factors for visceral leishmaniasis in anew epidemic site in Amhara region, Ethiopia. The American Journal of Tropical Medicine and Hygiene 81: 34-39. [ Ref ]
Bucheton B, Kheir MM, El-Safi SH, Hammad A, Mergani A, et al. (2002) The interplay between environmental and host factors during an outbreak of visceral leishmaniasis in eastern Sudan. Microbes and Infection 4: 1449-1457. [ Ref ]
Barnett PG, Singh SP, Bern C, Hightower AW, Sundar S (2005) Virgin soil: the spread of visceral leishmaniasis into Uttar Pradesh, India. The American Journal of Tropical Medicine and Hygiene 73: 720-725. [ Ref ]
Ranjan A, Sur D, Singhetal VP (2005) Risk factors for Indian Kala-azar. The American Journal of Tropical Medicine and Hygiene 73: 74-78. [ Ref ]
Kaiming Bi, Chen Y, Zhao S, Kuang Y, JohnWu CH (2018) Current Visceral Leishmaniasis Research: A Research Review to Inspire Future Study. Bio Med Research International 10: 9872095. [ Ref ]