Journal Name: Journal of Applied Microbiological Research
Article Type: Research
Received date: 08 February, 2021
Accepted date: 20 December, 2021
Published date: 27 December, 2021
Citation: Aborode AT, Adesewa VA, Ayomide OE, S larenwaju OO (2021) Demanding of Lassa Fever: Reducing its Risk as an Infectious Disease J Appl Microb Res. Vol: 4 Issu: 2 (31-37).
Copyright: © 2021 Aborode AT et al. This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
In recent years, Lassa fever has been announced as an infectious disease in the world, a few imported cases have been accounted for in various pieces of the world and there are developing worries of the possibilities of Lassa fever Virus as an organic weapon. Regardless of its assaulting impact, no substantial arrangement has been created to reduce the hazard of the ailment, about a large portion of 10 years after identifying it. A Review based on the documents from the literature search on PubMed, Scopus, Goggle Scholar and Science direct. Out of these, the final 16 articles that met the criteria were selected. Relevant information on epidemiology, the burden of management and control were obtained. Timely and effective containment of the Lassa fever disease in Lassa village four decades ago could have minimized the devastating effect and threats posed by this illness in the West African sub-region and indeed the entire globe. That was a hard lesson calling for much more proactive measures towards the eradication of the illness at primary, secondary, and tertiary levels of health care. Hence, the paper is aimed at appraising the threats associated with Lassa fever disease; its demands on curtailing the menace of the epidemic, and recommendations on important focal points.
Keywords
Lassa Fever, Virus, Infectious Disease, Hazard, West Africa, Health Care, Epidemiology, Epidemic, Measures, Burden, Management.
Abstract
In recent years, Lassa fever has been announced as an infectious disease in the world, a few imported cases have been accounted for in various pieces of the world and there are developing worries of the possibilities of Lassa fever Virus as an organic weapon. Regardless of its assaulting impact, no substantial arrangement has been created to reduce the hazard of the ailment, about a large portion of 10 years after identifying it. A Review based on the documents from the literature search on PubMed, Scopus, Goggle Scholar and Science direct. Out of these, the final 16 articles that met the criteria were selected. Relevant information on epidemiology, the burden of management and control were obtained. Timely and effective containment of the Lassa fever disease in Lassa village four decades ago could have minimized the devastating effect and threats posed by this illness in the West African sub-region and indeed the entire globe. That was a hard lesson calling for much more proactive measures towards the eradication of the illness at primary, secondary, and tertiary levels of health care. Hence, the paper is aimed at appraising the threats associated with Lassa fever disease; its demands on curtailing the menace of the epidemic, and recommendations on important focal points.
Keywords
Lassa Fever, Virus, Infectious Disease, Hazard, West Africa, Health Care, Epidemiology, Epidemic, Measures, Burden, Management.
Introduction
As of Today, Lassa fever has been a major threat to most developing countries, however, several cases of Lassa fever with hazardous outcomes have been reported in various parts of the world which include North America, Europe, Asia, and so on [1-8]. The major growing concern of the possibility of the Lassa fever virus (LAV) as a biological weapon is real, yet no lasting solution to this problem has been developed, nearly half a century of its discovery in a remote village in West Africa.
To this end, the paper is aimed at evaluating the problems associated with LAF illness; the demand in halting the epidemic, and recommendations on important focal points. The resources of information used in this article include literature search on (1) PubMed, (2) Scopus and Science direct with the mesh words “Lassa fever”, “Epidemiology”, “symptoms” and “control”. Furthermore, resource information was also obtained from the websites of the World Health Organization (WHO) and the Center for Disease Control and Prevention (CDC). 245 related articles respectively were returned from the two major search engines. All the in-vivo and in-silico studies were excluded and only those papers directly focused on the topic were considered. Aftermath, 16 articles were identified and a further search at their references yielded 3 more result. The contents of these various articles were used in the preparation of the manuscript.
Epidemiology of Lassa Fever
Lassa fever is an acute hemorrhagic fever caused of Lassa virus (LAV) (European Federation of Audiology Societies, 2011), a bi-segmented ambisense single-stranded RNA virus that belongs to the family old world Arenaviridisae spp. [9,10]. It is prevalent in the West African sub-region where about 3-5 million, individuals are infected on a yearly basis [11]. The first comprehensive identification of this illness was at Lassa village in Nigeria in the year 1969, where 2 missionary nurses were infected and lost their lives in the process along with some other health workers [12,13].
Although there are existing report that this virus was first encountered in Sierra Leone (West Africa) about 10 years earlier [14]. Afterward, the illness has spread within the sub-region and beyond. Several Cases of Lassa fever have been reported in countries like South Africa, Zambia, and outside sub-Saharan Africa with catastrophic outcomes. The transmission of Lassa fever is majorly via the urines and faeces of the multi-mammate rat (Mastomys Natalensis Spp) which serves as the host to the virus. This rodent found majorly around homes and farm settlements has some distinctive features which includes the long hairless tail, pointed rostrum, and ventral surface lined by multiple mammary glands (in females) from the thorax down to its abdomen [15-20].
On average, Lassa fever weighs 20-80g, the head to body measures about 6-17cm and the tail 6-15cm. This malevolent rodent has an average life span of 2 years, breeds round the year with each pregnancy resulting in 16-20 litters [15]. Lassa fever (LF) is also acquired and transmitted through the body fluids of infected humans, fomites, and aerosol thereby causing high morbidity and mortality rates. In recent studies, it was speculated that at least 10,000 people die of Lassa fever in West Africa yearly [18].
Table 1: The classical clinical course of Lassa fever [21].
| Stage | Symptoms |
|---|---|
| 1 (days 1-3) | General weakness and malaise. High fever, >39°C, constant with peaks of 40-4°C |
| 2 (days 4-7) | Sore throat (with white exudative patches) very common; headache; back, chest, side, or abdominal pain; conjunctivitis; nausea and vomiting; diarrhea; productive cough; proteinuria; low blood pressure (systolic) |
| 3 (after 7 days) | Facial edema; convulsions; mucosal bleeding (mouth, nose, eyes); internal bleeding; confusion or disorientation |
| 4 (after 14 days) | Coma and death |
Clinical Features of Lassa Fever
The mode of presentation of Lassa fever can be nonspecific and hence the difficulty in the clinical diagnosis of some cases. However, the classical modes of presentation include high-grade fever >38°C, sore throat, retrosternal pain, cough, odynophagia, conjunctivitis, petechial hemorrhages, abdominal pains, vomiting, and diarrhea. It could also present with headache, joint paint pains, and facial swellings. The symptoms normally set in within first and third week of introduction to the LAV [19].
Throat assessment normally uncovers exudative pharyngitis and urinalysis frequently is portrayed by proteinuria. The neutrophil count is frequently discouraged. Neurological indications (tremors, spasms, meningitis manifestations, and so forth) are not normally present at this beginning period, in any case, sensorineural hearing loss at times presents. Recent research suggests that early sensorineural hearing loss and probably an early manifestation of other CNS features depict poor prognostication [16,20]. The classical clinical course of Lassa fever is demonstrated in table 1 [17,21].
The morbidity and mortality are influenced by some key factors such as the time of presentation, diagnosis, and commencement of appropriate treatment. Pregnancy carries a poor prognosis and most often fetuses are lost [22]. It is proposed that a solitary shot of a fitting portion of Ribavirin inside the first week of showing symptoms would lessen the death rate by 90% [12,16,20]. The case fatality rates vary among centers but could be as high as 16.5%-28% [23].
In a case study of 441 patients, McCormick et al. observed that the best indicator of Lassa fever incorporates the mix of fever, pharyngitis, retrosternal agony, and proteinuria (prescient worth 0.81) while for the result, the best indicator was the mix of fever, sore throat, and regurgitating (relative danger of death, 5.5) [23].
Moreover, they watched the accompanying intricacies: mucosal dying (17%), reciprocal or one-sided eighthnerve deafness (4%), and pleural (3%) or pericardial (2%) radiation. In a related study conducted among 908 patients by Inegbenebor et al. in Nigeria; cultural practices and hygiene were identified as strong factors promoting the propagation of the disease [21,24].
Patients with subclinical infections to Lassa fever pass un-noticed. However, this group along with survivors of the acute Lassa fever illness stands the risk of developing sensorineural hearing loss of different degrees in the future. The hearing loss is usually bilateral and can affect all frequencies of hearing and according to WHO about 25% of patients exposed to LAV are affected (WHO, 2005) [18,21]. The pathogenesis of this hearing loss is believed to follow an immunological reaction between the circulating Lassa virus antibodies and the basal cell membrane /outer hair cells of the cochlear [24]. Other neurological complications sometimes associated with survivors of Lassa fever are seizures, gait disturbances, tremors, and encephalitis.
Lassa Virus Diagnostic Challenges
One significant challenge in West Africa is differentiating between etiologies of febrile illness with similar initial clinical presentations, including malaria, influenza, dengue, yellow fever, and Lassa fever, with limited laboratory facility and reagent availabilities. Empirical treatment for presumed malaria or bacterial infection is often trialed, and Lassa fever is only suspected when a patient fails to improve with antimalarial and antibiotic therapy.
This diagnostic delay leads to delayed patient isolation, an increased potential for transmission to family members and health care workers, and delayed initiation of ribavirin therapy, thereby decreasing its beneficial effect.
Further highlighting the challenges of appropriate diagnostics is the emergence of Ebola virus in West Africa. A recent study found 60 to 70% of the patients with blood samples submitted to the Lassa Diagnostic Laboratory in Kenema, Sierra Leone, in the years prior to the Ebola virus outbreak were negative for malaria and Lassa virus, and there was serological evidence of Ebola and Marburg virus infections [25,26]. Correctly identifying the cause of an acute febrile illness in West Africa in an actionable time frame requires validated, rapid region-appropriate diagnostic assays.
Given the risk of person-to-person virus spread via bodily fluids, laboratory staff should be aware of the risk of Lassa virus when processing potentially infectious specimens. Poor sample storage and handling may pose a safety hazard to laboratory staff as well as decrease the sensitivity of diagnostic assays.
The World Health Organization guidelines for the collection, storage, and handling of specimens for Ebola virus testing should be followed when testing for Lassa virus [26,27]. BSL-4 precautions are recommended when handling specimens which may contain infectious Lassa virus; however, the availability of such high-containment laboratories is limited worldwide. If BSL-4 precautions are not available, samples may be handled in a class II or III biosafety cabinet or inactivated to allow safe handling of specimens under BSL-2 precautions [27-29].
While there are multiple methods for viral inactivation in the literature, different methods are appropriate depending on the intended downstream testing (e.g., molecular or immunological pathogen detection, clinical laboratory tests, etc.). Chemical inactivation using solutions containing guanidine salts (e.g., TRIzol, Triton X-100, and buffer AVL combined with ethanol) is well documented, is effective with multiple pathogens, and is commonly used [25-27].
Inactivation can be achieved by heating a blood specimen to 60°C for 60 min, although inactivation at 56°C for 30 min has been reported [28,29]. Depending on the sample matrix and the specific pathogen, heat exposure alone may not result in complete inactivation; the use of chemical denaturizing solutions in combination with heating to provide more complete inactivation is recommended [30].
Gamma irradiation is also used to inactivate Lassa virus in liquid and dried samples [31,32]. Since the required absorbed radiation dose for successful viral inactivation varies depending on the temperature of the sample, empirical sample safety testing is required to confirm inactivation [28].
The high-containment safety requirements complicate Lassa virus assay development and validation studies. Many assay reagents need to be generated under BSL-4 conditions. Synthetic nucleic acids and recombinant proteins are more commonly being used as assay components, but assay validation with mock clinical samples still requires viral materials generated under BSL-4 conditions.
The development of appropriate diagnostic assays is further complicated by significant Lassa virus diversity. The high nucleotide and amino acid diversity of Lassa virus isolates sequenced across West Africa can result in falsenegative results if the primer/probe
However, we are currently unaware of any Lassa virus diagnostic validation studies demonstrating assay performance using viruses isolated across West Africa that cover the wide diversity of Lassa genetic variation possible.
In the absence of a single, timely, pan-Lassa virus diagnostic assay, one future strategy could be the designing and validating of assays based on geographic region, as Lassa virus diversity generally clusters with geographic location [33]. While ideal for use in specific countries/regions, this approach, in the context of exported cases of Lassa fever from multiple countries where it is endemic, would require many validated assays being available for accurate diagnosis.
Medical Laboratory Diagnosis of LF towards Risk Reduction
The medical laboratory diagnoses of Lassa fever towards risk reduction are explained in detailed below:
Viral culture
Given the diagnostic challenges due to Lassa virus diversity, viral isolation in cell culture remains the “gold standard” for the diagnosis of Lassa fever, although RT-PCR and immunoassays have become commonly used assays for a clinically actionable diagnosis [34].
Viremia is often present at the time of presentation to medical care and declines after the sixth day of illness in patients who ultimately survived their infection, whereas it may persist until death in fatal cases [35]. Culturing is performed by the inoculation of sample specimens suspected of containing the virus in Vero E6 cells at 37°C [36].
A positive result may yield a cell cytopathic effect; however, a second method of detection, such as RT-PCR, viral antigen detection, or electron microscopy, must be used to confirm the identity of the virus [37]. Lassa virus may be cultured from blood, throat swabs, urine, and cerebrospinal fluid samples from patients, although the detection of virus in throat swabs and urine is inconsistent among patients with serum viremia [38,39]. The viral culture may be positive from organ samples (liver, spleen, lung, kidney, heart, and placenta) at autopsy in cases of fatal infections [37].
Viral culture allows for detection that is independent of genetic variations between strains and allows further characterization of the virus if desired. Viral culture also allows for the quantification of viremia, which may provide additional virus characterization information, as viremia with 103 50% tissue culture infective doses (TCID50)/ml has a fatality odds ratio of 3.7 compared with viremia with less than 103 TCID50/ml [35].
Viral culture is neither rapid, taking at least several days to produce results, nor widely available due to the need for BSL-4 precautions to handle live viral specimens, which limits its utility for the early diagnosis of Lassa infection.
Nucleic acid detection methods
Real-time RT-PCR is a commonly used diagnostic approach for infectious diseases due to the high specificity and sensitivity of the method and has become a clinical standard for Lassa fever diagnosis. Coupled with automated sample processing and 96-well-plate-based thermocyclers, large numbers of samples can be tested quickly and inexpensively [40].
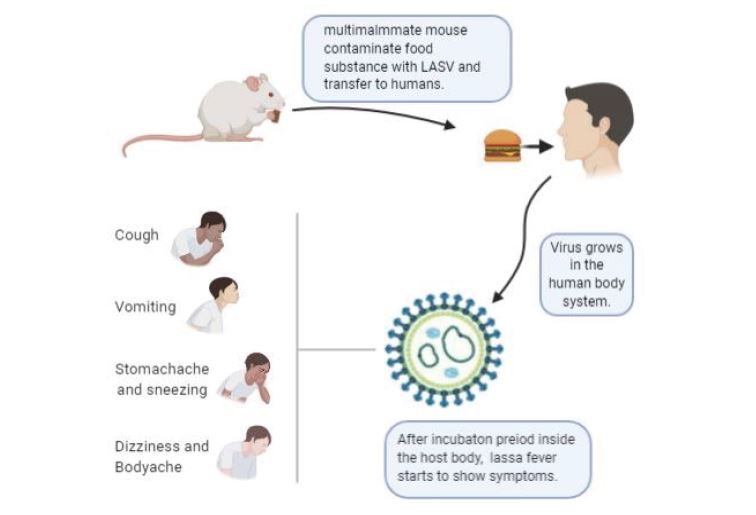
Figure 1:Mode of Transmission of Lassa Fever and Some of the symptoms. The primary host specie of the Lassa fever virus is the multimammate mouse (Mastomys natalensis). The host transmits the virus through contaminated food substances taken by humans. Upon entry into the human body system, the virus starts replicating itself and after about 7 days of incubation, symptoms will start showing. Some of the symptoms include cough, vomiting, tiredness, and dizziness.
PCR assays may be able to detect virus for a longer duration and earlier in illness compared with detection by viral culture and may be performed on chemically inactivated specimens [41].
The use of cycle threshold values with quantitative RT-PCR may assist with gross estimates of viremia using appropriately selected positive-control material for standard curve generation. Depending on the primers and virus strain used, the 95% probability limit of detection estimates with RT-PCR vary from 1,237 to 4,290 RNA copies/ml [42-44].
However, with highly diverse pathogens such as Lassa virus, genetic diversity can be problematic for nucleic acidbased assays, as even a single nucleotide variant in one of the primers can have a significant negative impact on assay sensitivity depending on the location of the nucleotide variant [45].
As additional sample testing and sequencing information becomes available, mismatches have been identified using established assays, necessitating assay redesign to improve performance. For example, Ölschläger and colleagues redesigned a commonly used standard RT-PCR assay for Lassa virus after identifying decreased assay sensitivity due to sequence variants for the reverse primer [44].
This new RT-PCR assay is widely used for screening samples for Lassa virus and performed well in an external quality assessment study conducted by the European Network for Diagnostics of Imported Viral Diseases [37]. Multiplex panels to simultaneously detect a multitude of viruses that can produce hemorrhagic fever syndromes, including Lassa and Ebola viruses, using RT-PCR alone or in combination with either enzyme hybridization or ligase detection reactions have also been developed [39,46,47].
Antigen and antibody detection assays
Given the high diversity of the Lassa virus genome and the austere laboratory conditions where Lassa fever is endemic, antigen- and antibody-based assays are attractive alternatives to the high specificity and technical requirements of PCR assays [45].
Antibody/antigen binding is generally less specific than primer/probe hybridization, allowing for greater flexibility in detecting diverse pathogens. Antigen detection relies on using specific antibodies against components of the Lassa virus to detect viral antigens in blood specimens. Initial assays detected nonspecific Lassa virus antigens with polyclonal antibodies, whereas more recent ELISAs target the Lassa virus nucleoprotein antigen [42].
A diagnosis based on the detection of the relatively conserved Lassa nucleoprotein antigen (Figure 1) may decrease the variability of test efficacy between genetically diverse viral strains in comparison to that from nucleic acidbased assays [46].
Lassa virus nucleoprotein antigen is detectable in patients with Lassa fever during the first week of illness and wanes during the second week in temporal association with the rise of detectable immunoglobulins [33].
Increased levels of antigenemia have been found in fatal cases of Lassa fever compared with those in nonfatal cases [48]. The short duration of antigenemia makes the detection of Lassa virus antigen more specific to acute Lassa virus infection than detection with antibody assays.
Antigen detection assays may diagnose Lassa fever earlier during illness than antibody assays, as antibodies frequently may not be detectable until the second week of illness [35]. However, Lassa virus antigen levels may become undetectable despite persistent viremia, and so a negative antigen test during an acute illness does not rule out Lassa fever [49].
Overall, the appropriate diagnosis of Lassa fever will likely require a combination of a clinically compatible presentation along with serological and molecular diagnostic assays. Having a rapid, point-of-care multiplex test that can diagnose Lassa fever as well as other high consequence pathogens, such as Ebola virus, would accelerate accurate diagnosis, patient isolation, and efficacious therapy.
As work for a Lassa virus vaccine and therapeutic moves toward laboratory studies, having well-validated diagnostic assays available will be a necessity to ensure appropriate patient enrollment and countermeasure performance.
Future directions for research in Lassa fever diagnostics should include assay improvement to increase detection across the genetically diverse spectrum of Lassa virus strains, assay validation to demonstrate efficacy across geographic regions and viral lineages, point-of-care diagnostic development and field validation, and content expansion of multiplex assays to distinguish Lassa fever from other diseases with similar clinical presentations.
Circumstances in the Control of Lassa fever
The high virulence and fatality rate of this disease is a major concern that is further complicated by the non-specific modes of presentation (mimicking some other fevers). From the foregoing, early presentation and subsequent diagnosis are usually not feasible, especially in our hinterlands and villages. The contagious nature of the illness poses a big threat to the Medical attendants, other hospital workers, and the caregivers who often are exposed to this disease unprotected, before diagnoses and establishment of barrier nursing. The fomite and aerosol mode of contraction posses a huge challenge to all who have close contact with the patients.
The control of the carrier vectors is herculean. The natural habitat of these rats within and around homes and farm settlements makes it cumbersome. Biological control by the introduction of safe predators to rats like cats within the endemic areas tentatively carries some prospect; however, the future consequences may be worse than the present. The ecosystem will be distorted because there is no way the cats will be able to selectively eliminate the Lassa rats alone. This line of reasoning could also be applied to why chemical control (rat pesticides) may also not suffice as an effective mode of control. Worse still, it may be possible that with time, following genetic transformations, such predators might transmute into Lassa Virus carriers. This will spell doom since these are household pets.
The inherent danger of complications that survivors and sub-clinically exposed individuals might suffer from is a concern. Studies had shown that survivors who developed severe sensorineural hearing loss had characteristic poor speech discrimination and were not amenable to hearing aids [20]. The role of antioxidants and hyperbaric oxygen in ameliorating hearing losses and other neurological complications remains hypothetical [50,51].
LF and its lethal features qualify it as a suitable biological weapon. Although the aerosol mode of transmission poses a threat to even the terrorists handling the virus, however, it might be argued that giving the growing rate of suicide bombers, such handlers may be unperturbed about any inherent consequences. Furthermore, accidentally imported cases to the rest of the world had been reported with dire consequences making LF a global challenge and not just a problem confined to the developing world.
Unavailability of safe vaccines and cost-effective/ efficient rapid kits for diagnoses nearly half a decade after identifying the disease has hampered the containment of the illness. The future lies in the effective and safe vaccination of the populace as in the case of yellow fever [52,53].
Recommendations
At the grass-root, continuing education of the populace on the dangers of the disease, its modes of presentation, and the need to seek medical treatment early should be intensified. Awareness (campaigns) and advocacy on a clean and safe environment to promote prevention especially within the endemic areas are necessary. Abrogation of practices that might enhance contact with the LAV should be encouraged.
The secondary level of control should involve setting up serviceable diagnostic and treatment centers for Lassa fever within the West African sub-region and beyond to enhance prompt therapy and containment of the illness. The health personnel that work in such centers should be well protected, paid enhanced salaries and their lives insured. Well designed and funded researches should be instituted in this field to facilitate ameliorating breakthroughs.
Finally, the ultimate aim should be towards producing a functional and safe anti-Lassa-fever-vaccine (which Aborode Abdullahi refers to as tertiary control) that could be incorporated into the Immunization programs for children and adults respectively. The adverse immunological responses to Lassa antibodies such as hearing loss must be taken into cognition before the approval of such a vaccine for human use.
Conclusion
Prompt and effective containment of the Lassa fever disease in Lassa village and other mapped areas about five decades ago could have saved the West African sub-region and indeed the entire globe from the devastating effect and threats posed by this illness. There is still a need for more proactive measures towards the eradication of the illness at primary, secondary, and tertiary levels of health care.
Competing Interests
The authors declare that there is no competing interest.
Mahdy MS, Chiang W, McLaughlin B, Derksen K (1989) Truxton BH, Neg K. Lassa fever: the first confirmed case imported into Canada. Can Dis Wkly Rep 15: 193-198. [ Ref ]
Ufberg JW, Karras DJ (2005) Update on emerging infections: news from the Centers for Disease Control and Prevention Imported Lassa fever. Ann Emerg Med 45: 323-326. [ Ref ]
Amorosa V, MacNeil A, McConnell R, Patel A, Dillon KE, et al. (2010) Imported Lassa fever, Pennsylvania, USA, 2010. Emerg Infect Dis 16: 1598-600. [ Ref ]
Hugonnet S, Sax H, Pittet D (2002) Management of viral hemorrhagic fevers in Switzerland. Euro Surveill 7: 42-44. [ Ref ]
Haas WH, Breuer T, Pfaff G, Schmitz H, Kohler P, et al. (2003) Imported Lassa fever in Germany: surveillance and management of contact persons. Clin Infect Dis 36: 1254-1258. [ Ref ]
Kitching A, Addiman S, Cathcart S, Bishop L, Krahé D, et al. (2009) A fatal case of Lassa fever in London, January 2009. Euro Surveill 14: 10-12. [ Ref ]
Hirabayashi Y, Oka S, Goto H, Shimada K, Kurata T, et al. (1989) The first imported case of Lassa fever in Japan. Nihon Rinsho 47: 71-75. [ Ref ]
Shimizu H (1989) Current status of imported infectious diseases and control policy of the Ministry of Health and Welfare. Nihon Rinsho 47: 11-15. [ Ref ]
European Federation of Audiology Societies (EFAS) (2011) Infections and acquired hearing loss in Africa. Journal of Hearing Science 1: 32-34. [ Ref ]
Rojek JM, Kunz S (2008) Cell entry by human pathogenic arenaviruses. Cell Microbiol 10: 828-835. [ Ref ]
Buchmeier MJ, de la Torre JC, Peters CJ (2007) Arenaviridae: The viruses and their replication. Fields Virology 5: 1791-1827. [ Ref ]
Frame JD, Baldwin JMJ, Gocke DJ, Troup JM (1970) Lassa fever, a new virus disease of man from West Africa: Clinical description and pathological findings. Am J Trop Med Hyg 19: 670-676. [ Ref ]
McCormick JB, Webb PA, Krebs JW, Johnson KM, Smith ES (1987) A prospective study of the epidemiology and ecology of Lassa fever. J Infect Dis 155: 437-44. [ Ref ]
Buckley SM, Casals J (1970) Lassa fever, a new virus disease of man from West Africa 3 Isolation and characterization of the virus. Am J Trop Med Hyg 19: 680-691. [ Ref ]
Burton M, Burton R (2006). Lassa fever: A Systematic Review. J Infect Dis 6: 1694-1695. [ Ref ]
McCormick JB (1986) Clinical, epidemiologic, and therapeutic aspects of Lassa fever. Med Microbiol Immunol 175: 153-155. [ Ref ]
Merlin K (2002) Licking Lassa fever: A Strategic review. Med Microbiol Immunol 1: 23-25. [ Ref ]
World Health Organization (2005) Lassa fever Fact Sheet. Lassa fever as an Infectious Disease 2: 2-5. [ Ref ]
Center Disease Control. (2011) Lassa fever. CDC Bulletin. [ Ref ]
Ibekwe TS, Okokhere PO, Asogun D, Blackie FF, Nwegbu MM, et al. (2011) Early-onset sensorineural hearing loss in Lassa fever. Eur. Arch. Otorhinolaryngol 268: 197-201. [ Ref ]
Inegbenebor U, Okosun J, Inegbenebor J (2010) Prevention of Lassa fever in Nigeria. Trans R. Soc Trop Med Hyg 104: 51-54. [ Ref ]
Branco LM, Boisen ML, Andersen KG, Grove JN, Moses LM, et al. (2011) Lassa Hemorrhagic Fever in a Late-Term Pregnancy from Northern Sierra Leone with a Positive Maternal Outcome: Case Report. Virol J 8: 400-404. [ Ref ]
McCormick JB, King IJ, Webb PA, Johnson KM, O’Sullivan R, et al (1987) A case-control study of the clinical diagnosis and course of Lassa fever. J Infect Dis 155: 445-455. [ Ref ]
Okokhere PO, Ibekwe TS, Akpede GO (2009) Sensorineural hearing loss in Lassa fever: two case reports. J Med Case Reports 3: 34-36. [ Ref ]
Blow JA, Dohm DJ, Negley DL, Mores CN (2004) Virus inactivation by nucleic acid extraction reagents. J Virol Methods 119: 195-198. [ Ref ]
Haddock E, Feldmann F, Feldmann H (2016) Effective chemical inactivation of Ebola virus. Emerg Infect Dis 22: 1292-1294. [ Ref ]
Smither SJ, Weller SA, Phelps A, Eastaugh L, Ngugi S, et al. (2015) Buffer AVL alone does not inactivate Ebola virus in a representative clinical sample type. J Clin Microbiol 53: 3148-3154. [ Ref ]
Elliott LH, McCormick JB, Johnson KM (1982) Inactivation of Lassa, Marburg, and Ebola viruses by gamma irradiation. J Clin Microbiol 16: 704-708. [ Ref ]
Mitchell SW, McCormick JB (1984) Physicochemical inactivation of Lassa, Ebola, and Marburg viruses and effect on clinical laboratory analyses. J Clin Microbiol 20: 486-489. [ Ref ]
Demby AH, Chamberlain J, Brown DW, Clegg CS (1994) Early diagnosis of Lassa fever by reverse transcription-PCR. J Clin Microbiol 32: 2898- 2903. [ Ref ]
Lytle CD, Sagripanti JL (2005) Predicted inactivation of viruses of relevance to biodefense by solar radiation. J Virol 79: 14244-14252. [ Ref ]
Sagripanti JL, Lytle CD (2011) Sensitivity to ultraviolet radiation of Lassa, vaccinia, and Ebola viruses dried on surfaces. Arch Virol 156: 489-494. [ Ref ]
Bowen MD, Rollin PE, Ksiazek TG, Hustad HL, Bausch DG, et al. (2000) Genetic diversity among Lassa virus strains. J Virol 74: 6992-7004. [ Ref ]
Emmerich P, Gunther S, Schmitz H (2008) Strain-specific antibody response to Lassa virus in the local population of West Africa. J Clin Virol 42: 40-44. [ Ref ]
Johnson KM, McCormick JB, Webb PA, Smith ES, Elliott LH, et al. (1987) Clinical virology of Lassa fever in hospitalized patients. J Infect Dis 155: 456-464. [ Ref ]
Trombley AR, Wachter L, Garrison J, Buckley-Beason VA, Jahrling J, et al. (2010) Comprehensive panel of real-time TaqMan polymerase chain reaction assays for detection and absolute quantification of filoviruses, arenaviruses, and New World Hantaviruses. Am J Trop Med Hyg 82: 954- 960. [ Ref ]
Nikisins S, Rieger T, Patel P, Muller R, Gunther S, et al. (2015) International external quality assessment study for molecular detection of Lassa virus. PLoS Negl Trop Dis 9: 003793. [ Ref ]
Safronetz D, Lopez JE, Sogoba N, Traore SF, Raffel SJ, et al. (2010) Detection of Lassa virus, Mali. Emerg Infect Dis 16: 1123-1126. [ Ref ]
Pang Z, Li A, Li J, Qu J, He C, et al. (2014) Comprehensive multiplex onestep real-time TaqMan qRT-PCR assays for detection and quantification of hemorrhagic fever viruses. PLoS One 9: 95633-95635. [ Ref ]
Bausch DG, Demby AH, Coulibaly M, Kanu J, Goba A, et al. (2001) Lassa fever in Guinea: I. Epidemiology of human disease and clinical observations. Vector Borne Zoonotic Dis 1: 269-281. [ Ref ]
Trappier SG, Conaty AL, Farrar BB, Auperin DD, McCormick JB, et al. (1993) Evaluation of the polymerase chain reaction for diagnosis of Lassa virus infection. Am J Trop Med Hyg. 49: 214-221. [ Ref ]
Drosten C, Gottig S, Schilling S, Asper M, Panning M, et al. (2002) Rapid detection and quantification of RNA of Ebola and Marburg viruses, Lassa virus, Crimean-Congo hemorrhagic fever virus, Rift Valley fever virus, dengue virus, and yellow fever virus by real-time reverse transcription- PCR. J Clin Microbiol 40: 2323-2330. [ Ref ]
Vieth S, Drosten C, Lenz O, Vincent M, Omilabu S, et al. (2007) RT-PCR assay for detection of Lassa virus and related Old World arenaviruses targeting the L gene. Trans R Soc Trop Med Hyg 101: 1253-1264. [ Ref ]
Olschlager S, Lelke M, Emmerich P, Panning M, Drosten C, et al. (2010) Improved detection of Lassa virus by reverse transcription-PCR targeting the 5′ region of S RNA. J Clin Microbiol 48: 2009-2013. [ Ref ]
Stadhouders R, Pas SD, Anber J, Voermans J, Mes TH, et al. (2010) The effect of primer-template mismatches on the detection and quantification of nucleic acids using the 5′ nuclease assay. J Mol Diagn 12: 109-117. [ Ref ]
He J, Kraft AJ, Fan J, Van Dyke M, Wang L, et al. (2009) Simultaneous detection of CDC category “A” DNA and RNA bioterrorism agents by use of multiplex PCR & RT-PCR enzyme hybridization assays. Viruses 1: 441-459. [ Ref ]
Das S, Rundell MS, Mirza AH, Pingle MR, Shigyo K, et al. (2015) A multiplex PCR/LDR assays for the simultaneous identification of category. A infectious pathogens: agents of viral hemorrhagic fever and variola virus. PLoS One 10: 138-144. [ Ref ]
Branco LM, Grove JN, Boisen ML, Shaffer JG, Goba A, et al. (2011) Emerging trends in Lassa fever: redefining the role of immunoglobulin M and inflammation in diagnosing acute infection. J Virol 8: 472-478. [ Ref ]
Jahrling PB, Niklasson BS, McCormick JB (1985) Early diagnosis of human Lassa fever by ELISA detection of antigen and antibody. Lancet 1: 250-252. [ Ref ]
Holy R, Navara M, Dosel P, Fundova P, Prazenica P, et al. (2011) Hyperbaric oxygen therapy in idiopathic sudden sensorineural hearing loss (ISSNHL) in association with combined treatment. Undersea Hyperb Med 38: 137-142. [ Ref ]
Sano H, Kamijo T, Ino T (2010) A free radical scavenger, in the treatment of idiopathic sudden sensorineural hearing loss with profound hearing loss. Auris Nasus Larynx 37: 42-46. [ Ref ]
Carrion R, Patterson JL, Johnson C, Gonzales M, Moreira CR, et al. (2007) A ML29 reassortant virus protects guinea pigs against a distantly related Nigerian strain of Lassa virus and can provide sterilizing immunity. Vaccine 25: 4093-4102. [ Ref ]
Lukashevich IS, Carrion R, Salvato MS, Mansfield K, Brasky K, et al. (2008). Safety, immunogenicity, and efficacy of the ML29 reassortant vaccine for Lassa fever in small non-human primates. Vaccine 26: 5246- 5254. [ Ref ]