Journal Name: Journal of Applied Microbiological Research
Article Type: Short Communication
Received date: 16 June, 2020
Accepted date: 17 August, 2020
Published date: 24 August, 2020
Citation: Nedim D, L Marsh M, Grunig G (2020) New Coronavirus (COVID-19) Pandemic: Complexities Resulting in a Tragedy. J Appl Microb Res. Vol: 3 Issu: 2 (14-20).
Copyright: © 2020 Nedim D et all. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
A striking aspect of COVID-19 is the difference in the outcome of the infection between different countries, and different ethnic groups within one country. We surveyed the literature on SARS-CoV-2 complemented with comparative publications on SARS-CoV and other coronaviruses to capture the current understanding of virus – host interactions. We particularly focused on virus subtypes, transmission, zoonotic aspects, and potential host determinants.
Keywords
COVID-19, Virus, Pandemic, Pneumonia
Abstract
A striking aspect of COVID-19 is the difference in the outcome of the infection between different countries, and different ethnic groups within one country. We surveyed the literature on SARS-CoV-2 complemented with comparative publications on SARS-CoV and other coronaviruses to capture the current understanding of virus – host interactions. We particularly focused on virus subtypes, transmission, zoonotic aspects, and potential host determinants.
Keywords
COVID-19, Virus, Pandemic, Pneumonia
Introduction
The novel coronavirus, SARS-CoV-2 which causes COVID-19, has caused many deaths and has put even more patients in intensive care, and therefore has induced much anxiety around the globe [1]. The COVID-19 disease started in Wuhan, China at the end of 2019 and has since become a pandemic affecting all countries globally.
Globally, and in the US, we have built biomedical response teams - from basic scientists, clinical trial persons, epidemiologists, clinical response teams, to the physicians, from public health officials, hospitals to biotech and pharmaceutical companies - all are trained to run towards the crisis. We are also trained in networked, coordinated collaborations that ultimately enable the clinical response team to come up with the optimal answer to a disease as dangerous and fear-inducing as COVID-19.
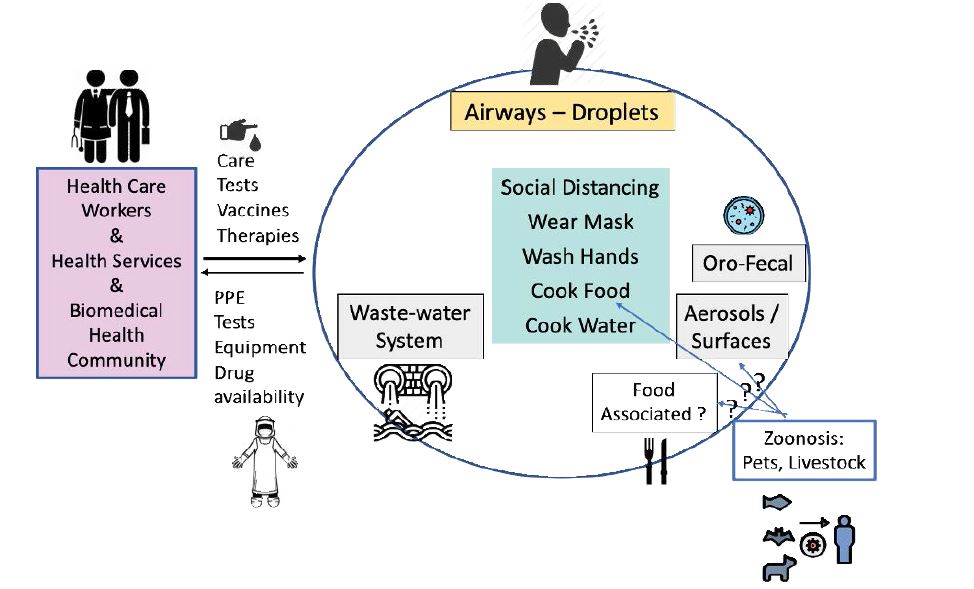
Early limitations included insufficient quantities of protective clothing and equipment for health care workers [2,3], and beds in hospital floors / wings / buildings that are dedicated to a highly communicable infectious disease staffed by well-equipped personnel. Intensive care equipment specifically reserved for the highly communicable infectious disease including ventilators are also limiting for a large concurrent number of patients, globally (schematically presented in figure 1).
To add to the health-related fears, our global economy is built on contact, travel and personal interaction. COVID-19 is having a major economic impact, for small and large businesses alike [4]. Therefore, the health care task force is now also asked to address the COVID-19 issue in order to get the economy back on its feet.
Research Methodology
To understand the effects of the SARS-CoV-2 infection, we performed a literature review on the material published January 01 to June 15, 2020. We searched Google Scholar and Google databases for SARS-CoV-2 or COVID-19 plus each of the specific questions addressed in this Perspective. We added manuscripts on SARS-CoV and other coronaviruses for comparative biology assessment, using the same databases and SARS-CoV, or MERS-CoV, or coronavirus plus specific question to be queried as keywords.
SARS-CoV-2
Virus RNA analysis indicates that the virus developed from a bat reservoir and used a mammalian intermediate host to mutate into a human specific virus [5-7]. Virus genome analysis suggests that there are at least two types of SARS-CoV-2 [8,9]. Three independent science groups have concluded that there is one haplotype that is older, more closely related to the bat viruses, and could have been circulating prior to the Wuhan strain. The region of origin in China of this older subtype remains uncertain, and this virus type potentially causes less severe disease, or spreads at lower frequency [8-10]. The Wuhan subtype SARS-CoV-2 is evolutionary younger, caused the outbreak of severe pneumonia cases in Wuhan and spreads extremely fast [8- 10]. These assertions are under debate [11,12] because the variation between the haplotypes is relatively minor, and different biological behavior between the two SARS-CoV-2 types has not been confirmed experimentally [11]. Another independent group has also analyzed virus genomes and concludes that there is a sub-type that has emerged in Wuhan prior to the outbreak of the Wuhan pneumonia, and that the prior subtype is closer to the bat genomes and distinct from the subtype that caused the Wuhan pneumonia outbreak [13]. Furthermore, groups have described SARS-CoV-2 drift variants, seen particularly in Europe [14]. Current PCR tests are designed to identify SARS-CoV-2 [15], but they do not distinguish between SARS-CoV-2 subtypes. Whole genome analysis of SARS-CoV-2 has been used to trace the origin of infectious outbreaks in certain geographic regions to virus sources. In all four studies that have inferred an ancestral type and a later type that caused the Wuhan outbreak, both types of SARS-CoV2 were later traced and sequenced throughout the world (e.g. United States [8-10,13], Japan [8- 10,13], Australia [8-10,13], Korea [9], Taiwan [9], England [9]). Therefore, even if there are SARS-CoV-2 types that cause different outcomes in the host (subclinical, or mild vs. severe disease), this cannot be inferred by geographical location, but will have to be investigated using personal whole-genome virus analysis studies.
Analysis of the virus sequence, structure and cell infection studies have identified the SARS-CoV-2 protein, spike protein, that binds to the cellular receptor, ACE- 2 angiotensin converting enzyme-2 [5,7,16]. The crystal structure of the spike protein identified key differences between SARS-CoV-2 and SARS virus in the receptor binding site [17,18]. In addition to receptor binding, virus entry requires proteolytic cleavage of ACE2 or spike protein by a cell surface bound cellular protease, most prominently transmembrane protease serine 2 (TMPRSS2) [19]. The proteolytic cleavage of spike protein is essential for virus entry into the cells [19,20].
Fewer reports indicate that SARS-CoV-2 can utilize another cell entry way via CD147 [21,22]. CD147 exhibits a different expression pattern, which includes leukocytes, erythrocytes and skeletal muscle. T cells have been reported to be infected by SARS-CoV-2 via membrane fusion [23]. However, blood samples have been mostly negative for virus RNA [24], therefore it is not clear how frequently the CD147 virus entry or the membrane fusion pathways are utilized.
Management
The most important management tool is social distancing (closure of schools, universities, restaurants, art institutions, sports, limiting gathering in groups, delaying elections, distancing between individuals, limiting travel) [25,26]. Currently, there is not yet any specific treatment available for COVID-19. To bridge the time until specific treatment becomes available, drug libraries have been scanned to identify candidates that could be repurposed for COVID-19 [27,28], and new potential drug candidates were identified (e.g. remdesivir [29,30]). Despite still ongoing or inconclusive clinical trials [31], antiviral treatment is regularly used in China [32,33], Singapore [34], many European Countries [35], and in the United States [29,36]. A global clinical trial of these drugs has just been announced by the World Health Organization [37].
Prophylactic treatment is being evaluated in clinical trials [38]. This could be considered for health care workers, persons at high risk, their caretakers and families who live in hot-spot areas, and who have been in contact with persons who tested positive.
Vaccine
Clinical vaccine trials have just started in the United States [39], and others are planned globally and in the United States [40]. One vaccine is approved for a limited population in Russia [41]. However, it will take many more months until a safe and effective vaccine is available. The strategy used for the human vaccines relies on recombinant molecular biology technology to create recombinant viruses / virus epitopes. Even in the case that the vaccines may induce immune responses that are not fully protective, they will aid in boosting the response to virus challenge.
Transmission
ACE2 and TMPRSS2 co-expression is most frequently observed in epithelial cells, for example in the tracheal, bronchi and alveoli, as well as intestinal epithelial cells [42]. This expression pattern corresponds to an aerogenic transmission which is also supported by detection of the virus in pharyngeal swabs, and sputum (Figure 1 schematic). Additionally, oro-fecal virus shedding occurs to a lesser degree and lower frequency, and virus is detected in stool samples even in the absence of diarrhea [24,43]. A consequence of the presence of fecal SARS-CoV-2 RNA and the environmental stability of the virus [44] is the detection of virus RNA in sewage, for example measured close to the Amsterdam Airport and in other cities in the Netherlands, Massachusetts and in Australia [45-48]. The detection of virus RNA in wastewater can be used as an indicator of the presence of the virus in the population [45-47]. Experimental spiking of coronaviruses to wastewater has demonstrated virus stability for 1-3 days [49]. Based on these experimental studies and virus transmission tracking of the previous SARS virus (SARS-CoV) [50,51], water and wastewater aerosols could also be potential routes of transmission of the current SARS-CoV-2 [52,53].
Using the previous SARS-CoV data to derive a modeling framework, the current SARS-CoV-2 outbreak was analyzed. This indicates that fecal-oral transmission (e.g. via aerosol droplets from wastewater) has played a role in amplifying the epidemic in Wuhan, but not the less severe outbreaks in Singapore and Taiwan [54]. However, direct experimental studies of infectious SARS-CoV-2 in feces or wastewater are not available yet.
Tests
Diagnostic tests are based on the detection of virus RNA or antibodies specific for SARS-CoV-2 [55]. Current limitations of the test for virus RNA are that these tests are rather slow, and do not distinguish between virus sub-types. Antibody assays are designed with the receptor binding site of spike protein, or the nucleocapsid protein of SARSCoV- 2 as antigens (baits) [56-58]. These antibodies are expected to be virus neutralizing because they reduce virus replication. Antibody tests will identify people who have already undergone SARS-CoV-2 infection and will help to trace the virus [59]. The tests will also allow for a deepened understanding of the pathogenesis of COVID-19 [60-68]. Furthermore, the identification of neutralizing antibodies can be used for therapeutic purposes by engineering these antibodies in vitro for passive immunization of person affected with COVID-19. Passive immunization, for a relatively few number of patients, can also be achieved by administration of convalescent plasma [69].
Figure 1: COVID-19, schematic of measures to control spreading and infection. Established measures and pathways are denoted by text boxes and arrows while pathways needing further studies are indicated by ‘?’. Abbreviation: PPE – Personal Protective Equipment.
Zoonosis
COVID-19 started as a zoonosis. The precursor of SARSCoV- 2 developed in bats. Perhaps climate change that affects reproduction and feeding behaviors [70], and fungal disease prevalence in bats may have caused more replication and mutation of coronaviruses in these animals [71]. The closest relative to SARS-CoV-2 infected an intermediate host, most likely a mammalian host. There is no evidence exactly how SARS-CoV-2 migrated to humans and acquired the ability to spread from human to human. Additional direct observations of the zoonosis [72,73] include a small but measurable virus load in two dogs in Hong Kong, China, perhaps transmitted by their human owners [74]. Further, the Bronx Zoo in New York City, United States, has had 5 tigers and 3 lions that tested positive for SARS-CoV-2 [73,75,76]. The test on the first tiger was performed on nasal swab, the tests on the other animals on fecal samples. Seven of the 8 big cats showed dry coughs and their animal handler presented as asymptomatic SARSCoV- 2 carrier [76]. Because humans usually stay at distance from tigers and lions, there may be a possibility that the animal’s food (raw meat) or water may have become virus positive and this is how the virus was transmitted. Reports from China identified house cats with antibodies against SARS-CoV-2 [77]; two house cats from Belgium and two house cats with respiratory symptoms from New York were identified as virus positive [78,79]. Experimental infection studies from two independent groups have demonstrated that house cats can be infected by the airway route, and that they can transmit the virus to co-housed cats [80,81]. Social distancing may be a suggestion to pets, for example, dog runs were closed in New York City as of April 6, 2020 due to potential overcrowding. There are few feral cats in big cities like New York City, and therefore, cats or other pet animals are currently not considered a virus reservoir that would amplify the infection risk for humans [82].
There are no reports that livestock like pigs, chicken or cattle are infected by SARS-CoV-2. However, experimental infection studies were only performed via the airway route, the oral infection route was not explored [80,83]. Systematic testing of meats and poultry is still lacking. On the other hand, comparative analysis of the ACE-2 binding site for the SARS-CoV-2 spike protein [84], and a cell transfection study with pig ACE-2 [7] has suggested that livestock could be potentially infected. Livestock meat processing plants in the United States have had a spike of SARS-CoV-2 positive workers in many states, forcing the plants to close [85]. It is possible that infections occurred because of humans working together in close proximity. Regardless of infection source, food products could potentially become contaminated because of the environmental stability of the virus (Figure 1 schematic), although this has not been demonstrated. Food packaging can also be positive for SARS-CoV-2 but this is thought to be an unlikely source for virus spread [86]. International public health organizations recommend to cook meat and eggs [87,88].
Risk
Many chronic conditions increase the risk for COVID-19 including hypertension, cardiovascular disease, diabetes, cancer, autoimmune disease [25,32,34,89,90]. In many of these cases, the underlying disease causes changes that predispose for severe outcome. In others, COPD, nicotine inhaled via cigarette or perhaps also e-cigarette smoking has been shown to increase the expression of ACE-2 in the airways [91,92], thereby providing more cellular targets of SARS-CoV-2.
The highest risk for COVID-19 is posed by group living of mostly elderly people in a nursing home or retirement home, where many of the residents may not survive COVID-19 [93]. The age of the persons in group housing is not the determinant of the increased susceptibility to being infected with SARS-CoV-2. Group housing of groups of persons of mixed age on cruise ships has resulted in multiple outbreaks of COVID-19 [94]. Large groups of younger persons living at close quarters on naval ships are also at increased risk for becoming infected with SARS-CoV-2, some of whom developed COVID-19, and consequently died [95]. Perhaps people living at close proximity, the high risk of SARS-CoV-2 infection is determined by the multiplicity of routes of transmission that SARS-CoV-2 can take (inhalational person to person, environmental, oro-fecal).
Other groups that were generally considered particularly vulnerable, are not at increased risk, among them children [96] and pregnant women [97]. In those groups, SARS-CoV-2 infection can occur but there is a substantial percentage of sub-clinical or mild infection [96,97]. However, recently a still rare multisystem inflammatory syndrome associated with SARS-CoV-2 infections has been identified in children [98-100].
Among patients affected with chronic lung diseases, some are not over-proportionally represented among COVID cases, these include asthma [101], and pulmonary arterial hypertension [102]. A search for studies demonstrating clear anti-viral activity of common drugs taken for these conditions has not yielded clear positive data. Therefore, one explanation for the observed data in these patient groups is that infectious disease prophylaxis is routinely and stringently performed as part of the daily management, because any infectious disease could cause a major exacerbation with severe consequences.
Ethnic disparity for COVID-19 incidence and severity has been reported for the United States, particularly for persons of color [103,104]. In the data published June 7, 2020 by the state of New York, excluding New York City, African Americans represent 9% of the population, while Covid-19 fatalities are 18% [105]. Whites have a relative lower percentage of Covid-19 fatalities (60%) relative to the percentage of the population (74%) [105]. Analyzing the United states nationally for COVID-19 hotspots identified 79 counties with a population of more than 25 million [104]. In these hotpot counties, persons of color had a disproportionally high incidence of COVID-19 [104]. Currently there is no scientific evidence to support genetic resistance that would be the major determinant of this disparity based on polymorphisms in the ACE2 gene [106]. Instead, social and health care disparities are likely the reason for the disparate outcome to SARS-CoV-2 [103, 107].
Conclusion
Complexities of transmission, the potential of different responses due to variations in the virus and the zoonotic aspects of SARS-CoV-2 are perhaps the most underappreciated aspects of the COVID-19 pandemic. The management of the pandemic is aimed at protecting these persons who are at risk and also elderly persons [89] and to avert mortality – which could strike anyone infected with SARS-CoV-2. It is important to note that COVID-19 can develop in persons younger than 45 years of age and in children [108,109]. Specific treatments and specific vaccines for SARS-CoV-2 are still many months away and therefore, a big fear concerns the global economy which depends on the health care system’s ability to mitigate COVID-19 now. We also have to keep in mind of living in a global world like a village now, only having national crisis plans are not enough, international collaborative plans should be available for the management of SARS-CoV-2 and possible future pandemics.
Maxmen A, Tollefson J (2020) Two decades of pandemic war games failed to account for donald trump. Nature 584: 26-29. [ Ref ]
Mahase E (2020) Coronavirus: Global stocks of protective gear are depleted, with demand at 100 times normal level, who warns. British Medical Journal Publishing Group 368: m543. [ Ref ]
Ong SWX, Tan YK, Chia PY, Lee TH, Ng OT, et al. (2020) Air, surface environmental, and personal protective equipment contamination by severe acute respiratory syndrome coronavirus 2 (sars-cov-2) from a symptomatic patient. The Journal of the American Medical Association 323: 1610-1612. [ Ref ]
Bonaccorsi G, Pierri F, Cinelli M, Flori A, Galeazzi A, et al. (2020) Economic and social consequences of human mobility restrictions under covid-19. Proc Natl Acad Sci USA 117: 15530-15535. [ Ref ]
Lu R, Zhao X, Li J, Niu P, Yang B, et al. (2020) Genomic characterisation and epidemiology of 2019 novel coronavirus: Implications for virus origins and receptor binding. Lancet 395: 565-574. [ Ref ]
Wu F, Zhao S, Yu B, Chen YM, Wang W, et al. (2020) A new coronavirus associated with human respiratory disease in china. Nature 579: 265- 269. [ Ref ]
Zhou P, Yang XL, Wang XG, Hu B, Zhang L, et al. (2020) A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature 579: 270-273. [ Ref ]
Tang X, Wu C, Li X, Song Y, Yao Z, et al. (2020) On the origin and continuing evolution of sars-cov-2. National Science Review 7: 1012-1023. [ Ref ]
Zhang L, Yang JR, Zhang Z, Lin Z (2020) Genomic variations of sars-cov-2 suggest multiple outbreak sources of transmission. MedRxiv. [ Ref ]
Yu WB, Tang GD, Zhang L, Corlett RT (2020) Decoding the evolution and transmissions of the novel pneumonia coronavirus (sars-cov-2) using whole genomic data. ChinaXiv. [ Ref ]
MacLean O, Orton R, Singer J, Robertson D (2020) Response to on the origin and continuing evolution of sars-cov-2. [ Ref ]
Johnson N (2020) Faculty opinions recommendation of [tang x et al., natl sci rev 2020]. f1000 In Faculty Opinions, 06 Mar 2020. [ Ref ]
Fang B, Liu L, Yu X, Li X, Ye G, et al. (2020) Genome-wide data inferring the evolution and population demography of the novel pneumonia coronavirus (sars-cov-2). Biorxiv. [ Ref ]
Koyama T, Weeraratne D, Snowdon J, Parida L (2020) Emergence of drift variants that may affect covid-19 vaccine development and antibody treatment. Pathogens 9: 324. [ Ref ]
Corman VM, Landt O, Kaiser M, Molenkamp R, Meijer A, et al. (2020) Detection of 2019 novel coronavirus (2019-ncov) by real-time rt-pcr. Euro Surveill 25: 2000045. [ Ref ]
Letko M, Marzi A, Munster V (2020) Functional assessment of cell entry and receptor usage for sars-cov-2 and other lineage b betacoronaviruses. Nat Microbiol 5: 562-569. [ Ref ]
Wrapp D, Wang N, Corbett KS, Goldsmith JA, Hsieh HL, et al. (2020) Cryoem structure of the 2019-ncov spike in the prefusion conformation. Science 367: 1260-1263. [ Ref ]
Yan R, Zhang Y, Li Y, Xia L, Guo Y et al. (2020) Structural basis for the recognition of the sars-cov-2 by full-length human ace2. Science 367: 1444-1448. [ Ref ]
Hoffmann M, Kleine-Weber H, Schroeder S, Krüger N, Herrler T, et al. (2020) Sars-cov-2 cell entry depends on ace2 and tmprss2 and is blocked by a clinically proven protease inhibitor. Cell 181: 271-280.e8. [ Ref ]
Meng T, Cao H, Zhang H, Kang Z, Xu D, et al. (2020) The insert sequence in sars-cov-2 enhances spike protein cleavage by tmprss. biorxiv. [ Ref ]
Wang K, Chen W, Zhou YS, Lian JQ, Zhang Z, et al. (2020) Sars-cov-2 invades host cells via a novel route: Cd147-spike protein. biorxiv. [ Ref ]
Bian H, Zheng ZH, Wei D, Zhang Z, Kang WZ, et al. (2020) Meplazumab treats covid-19 pneumonia: An open-labelled, concurrent controlled add-on clinical trial. medRxiv. [ Ref ]
Wang X, Xu W, Hu G, Xia S, Sun Z, et al. (2020) Sars-cov-2 infects T lymphocytes through its spike protein-mediated membrane fusion. Cellular & Molecular Immunology. [ Ref ]
Woelfel R, Corman VM, Guggemos W, Seilmaier M, Zange S, et al. (2020) Clinical presentation and virological assessment of hospitalized cases of coronavirus disease 2019 in a travel-associated transmission cluster. medRxiv. [ Ref ]
Mizumoto K, Chowell G (2020) Estimating risk for death from 2019 novel coronavirus disease, china, january-february 2020. Emerging infectious diseases 26: 1251-1256. [ Ref ]
Wilder-Smith A, Freedman D (2020) Isolation, quarantine, social distancing and community containment: Pivotal role for old-style public health measures in the novel coronavirus (2019-ncov) outbreak. Journal of travel medicine 27: taaa020. [ Ref ]
Li G, De Clercq E (2020) Therapeutic options for the 2019 novel coronavirus (2019-ncov). Nat Rev Drug Discov 19: 149-150. [ Ref ]
Wang M, Cao R, Zhang L, Yang X, Liu J, et al. (2020) Remdesivir and chloroquine effectively inhibit the recently emerged novel coronavirus (2019-ncov) in vitro. Cell Res 30: 269-271. [ Ref ]
Grein J, Ohmagari N, Shin D, Diaz G, Asperges E, et al. (2020) Compassionate use of remdesivir for patients with severe covid-19. New England Journal of Medicine. [ Ref ]
Wang Y, Zhang D, Du G, Du R, Zhao J, et al. (2020) Remdesivir in adults with severe covid-19: A randomised, double-blind, placebo-controlled, multicentre trial. The Lancet 395: 1569-1578. [ Ref ]
Cao B, Wang Y, Wen D, Liu W, Wang J, et al. (2020) A trial of lopinavirritonavir in adults hospitalized with severe covid-19. N Engl J Med 382: 1787-1799. [ Ref ]
Wu C, Chen X, Cai Y, Xia J, Zhou X, et al. (2020) Risk factors associated with acute respiratory distress syndrome and death in patients with coronavirus disease 2019 pneumonia in wuhan, china. The Journal of the American Medical Association Intern Med 180: 934-943. [ Ref ]
Yang X, Yu Y, Xu J, Shu H, Xia J, et al. (2020) Clinical course and outcomes of critically ill patients with sars-cov-2 pneumonia in wuhan, china: A single-centered, retrospective, observational study. Lancet Respir Med 8: 475-481. [ Ref ]
Young BE, Ong SWX, Kalimuddin S, Low JG, Tan SY, et al. (2020) Epidemiologic features and clinical course of patients infected with sarscov- 2 in singapore. The Journal of the American Medical Association 323: 1488-1494. [ Ref ]
Belgium Task Force for COVID-19 (2020) Interim clinical guidance for patients suspected of/confirmed with covid-19 in belgium. [ Ref ]
Pastick KA, Okafor EC, Wang F, Lofgren SM, Skipper CP, et al. (2020) Hydroxychloroquine and chloroquine for treatment of sars-cov-2 (covid-19). Presented at Open Forum Infectious Diseases 7: ofaa130. [ Ref ]
World Health Organization (2020) Who director-general’s opening remarks at the media briefing on covid-19 - 18 march. [ Ref ]
Clinical Trials (2020) g. Hydroxychloroquine post exposure prophylaxis for coronavirus disease (covid-19). [ Ref ]
National Institutes of Health (2020) NIH clinical trial of investigational vaccine for covid-19 begins. [ Ref ]
Gates B (2020) Responding to covid-19-a once-in-a-century pandemic? New England Journal of Medicine 382:1677-1679. [ Ref ]
Cohen J (2020) Russia’s approval of a covid-19 vaccine is less than meets the press release. Science News Aug 11, 2020. [ Ref ]
Zhang H, Kang Z, Gong H, Xu D, Wang J, et al. (2020) The digestive system is a potential route of 2019-ncov infection: A bioinformatics analysis based on single-cell transcriptomes. bioRxiv. [ Ref ]
Chen Y, Chen L, Deng Q, Zhang G, Wu K, et al. (2020) The presence of sars-cov-2 rna in feces of covid‐19 patients. Journal of Medical Virology 92: 833-840. [ Ref ]
Goh GKM, Dunker AK, Foster JA, Uversky VN (2020) Shell disorder analysis predicts greater resilience of the sars-cov-2 (covid-19) outside the body and in body fluids. Microb Pathog 144: 104177. [ Ref ]
Lodder W, de Roda Husman AM (2020) Sars-cov-2 in wastewater: Potential health risk, but also data source. The Lancet Gastroenterology & Hepatology 5: 533-534. [ Ref ]
Medema G, Heijnen L, Elsinga G, Italiaander R, Brouwer A (2020) Presence of sars-coronavirus-2 in sewage. MedRxiv. [ Ref ]
Wu F, Xiao A, Zhang J, Gu X, Lee WL, et al. (2020) Sars-cov-2 titers in wastewater are higher than expected from clinically confirmed cases. MedRxiv. [ Ref ]
Ahmed W, Angel N, Edson J, Bibby K, Bivins A, et al. (2020) First confirmed detection of sars-cov-2 in untreated wastewater in australia: A proof of concept for the wastewater surveillance of covid-19 in the community. Science of The Total Environment 728: 138764. [ Ref ]
Gundy PM, Gerba CP, Pepper IL (2009) Survival of coronaviruses in water and wastewater. Food and Environmental Virology 1: 10. [ Ref ]
Leung WK, To KF, Chan PK, Chan HL, Wu AK, et al. (2003) Enteric involvement of severe acute respiratory syndrome-associated coronavirus infection. Gastroenterology 125: 1011-1017. [ Ref ]
Hung LS (2003) The sars epidemic in hong kong: What lessons have we learned? Journal of the Royal Society of Medicine 96: 374-378. [ Ref ]
Naddeo V, Liu H (2020) Editorial perspectives: 2019 novel coronavirus (sars-cov-2): What is its fate in urban water cycle and how can the water research community respond? Environmental Science: Water Research and Technology 6: 1213-1216. [ Ref ]
Meng X, Huang X, Zhou P, Li C, Wu A (2020) Alert for sars-cov-2 infection caused by fecal aerosols in rural areas in china. Infection Control & Hospital Epidemiology 7: 1-4. [ Ref ]
Danchin A, Ng TWP, Turinici G (2020) A new transmission route for the propagation of the sars-cov-2 coronavirus. medRxiv. [ Ref ]
Patel R, Babady E, Theel ES, Storch GA, Pinsky BA, et al. (2020) Report from the american society for microbiology covid-19 international summit, 23 march 2020: Value of diagnostic testing for sars–cov-2/ covid-19. Am Soc Microbiol 11: e00722-20. [ Ref ]
Li Z, Yi Y, Luo X, Xiong N, Liu Y, Li S, et al. (2020) Development and clinical application of a rapid igm‐igg combined antibody test for sarscov‐ 2 infection diagnosis. Journal of Medical Virology. [ Ref ]
Okba NM, Muller MA, Li W, Wang C, GeurtsvanKessel CH et al. (2020) Sars-cov-2 specific antibody responses in covid-19 patients. medRxiv. [ Ref ]
Stadlbauer D, Amanat F, Chromikova V, Jiang K, Strohmeier S, et al. (2020) Sars-cov-2 seroconversion in humans: A detailed protocol for a serological assay, antigen production, and test setup. Current Protocols in Microbiology 57: e100. [ Ref ]
Yong SEF, Anderson DE, Wei WE, Pang J, Chia WN,et al. (2020) Connecting clusters of covid-19: An epidemiological and serological investigation. The Lancet Infectious Diseases 20: 809-815. [ Ref ]
Long QX, Liu BZ, Deng HJ, Wu GC, Deng K, et al. (2020) Antibody responses to sars-cov-2 in patients with covid-19. Nature Medicine 26: 845-848. [ Ref ]
To KKW, Tsang OTY, Leung WS, Tam AR, Wu TC, et al. (2020) Temporal profiles of viral load in posterior oropharyngeal saliva samples and serum antibody responses during infection by sars-cov-2: An observational cohort study. The Lancet Infectious Diseases 20: 565-574. [ Ref ]
Zhao J, Yuan Q, Wang H, Liu W, Liao X, et al. (2020) Antibody responses to sars-cov-2 in patients of novel coronavirus disease 2019. Clinical Infectious Diseases 28: ciaa344. [ Ref ]
Wang B, Wang L, Kong X, Geng J, Xiao D, et al. (2020) Long-term coexistence of severe acute respiratory syndrome coronavirus 2 (sarscov- 2) with antibody response in coronavirus disease 2019 (covid-19) patients. medRxiv. [ Ref ]
Yongchen Z, Shen H, Wang X, Shi X, Li Y, et al. (2020) Different longitudinal patterns of nucleic acid and serology testing results based on disease severity of covid-19 patients. Emerging microbes & infections 9: 833-836. [ Ref ]
Okba NM, Müller MA, Li W, Wang C, GeurtsvanKessel CH, et al. (2020) Severe acute respiratory syndrome coronavirus 2-specific antibody responses in coronavirus disease 2019 patients. Emerging infectious diseases 26: 1478-1488. [ Ref ]
Wölfel R, Corman VM, Guggemos W, Seilmaier M, Zange S, et al. (2020) Virological assessment of hospitalized patients with covid-2019. Nature 581: 465-469. [ Ref ]
Grzelak L, Temmam S, Planchais C, Demeret C, Huon C, et al. (2020) Sars-cov-2 serological analysis of covid-19 hospitalized patients, paucisymptomatic individuals and blood donors. medRxiv. [ Ref ]
Amanat F, Nguyen T, Chromikova V, Strohmeier S, Stadlbauer S, et al. (2020) A serological assay to detect sars-cov-2 seroconversion in humans. medRxiv. [ Ref ]
Chen L, Xiong J, Bao L, Shi Y (2020) Convalescent plasma as a potential therapy for covid-19. The Lancet Infectious Diseases 20: 398-400. [ Ref ]
Lučan RK, Weiser M Hanák V (2013) Contrasting effects of climate change on the timing of reproduction and reproductive success of a temperate insectivorous bat. Journal of Zoology 290: 151-159. [ Ref ]
Carlson CJ, Albery GF, Merow C, Trisos CH, Zipfel CM, et al. (2020) Climate change will drive novel cross-species viral transmission. biorxiv. [ Ref ]
Leroy EM, Gouilh MA Brugère-Picoux J (2020) The risk of sars-cov-2 transmission to pets and other wild and domestic animals strongly mandates a one-health strategy to control the covid-19 pandemic. One Health. [ Ref ]
Gryseels S, De Bruyn L, Gyselings R, Calvignac-Spencer S, Leendertz Fand H et al. (2020) Risk of human-to-wildlife transmission of sars-cov-2. [ Ref ]
Almendros A (2020) Can companion animals become infected with covid-19? Veterinary Record 186: 388-389. [ Ref ]
Center for Disease Control and Prevention (2020) COVID-19 and Animals. [ Ref ]
Wildlife Conservation Society (2020) Update: Bronx zoo tigers and lions recovering from covid-19. [ Ref ]
Zhang Q, Zhang H, Huang K, Yang Y, Hui X, et al. (2020) Sars-cov-2 neutralizing serum antibodies in cats: A serological investigation. bioRxiv. [ Ref ]
American Veterinary Medical Association (2020) Sars-cov-2 in animals, including pets. [ Ref ]
U.S. Centers for Disease Control and Prevention (2020) Confirmation of covid-19 in two pet cats in new york. [ Ref ]
Shi J, Wen Z, Zhong G, Yang H, Wang C, et al. (2020) Susceptibility of ferrets, cats, dogs, and other domesticated animals to sars–coronavirus 2. Science 368: 1016-1020. [ Ref ]
Halfmann PJ, Hatta M, Chiba S, Maemura T, Fan S, et al. (2020) Transmission of sars-cov-2 in domestic cats. N Engl J Med 383: 592-594. [ Ref ]
United States Department of Agriculture (2020) USDA statement on the confirmation of covid-19 in a tiger in new york. [ Ref ]
Schlottau K, Rissmann M, Graaf A, Schön J, Sehl J, et al. (2020) Sars-cov-2 in fruit bats, ferrets, pigs, and chickens: An experimental transmission study. The Lancet Microbe. [ Ref ]
Luan J, Lu Y, Jin X, Zhang L (2020) Spike protein recognition of mammalian ace2 predicts the host range and an optimized ace2 for sarscov- 2 infection. Biochem Biophys Res Commun 526: 165-169. [ Ref ]
National Public Radio, U.S. (2020) Meat supply is ‘perilously close’ to a shortage, CEO warns. [ Ref ]
Heidt A (2020) Coronavirus found on food packaging, but likely of little concern. The Scientist News, Aug 13, 2020. [ Ref ]
Bhosale S, Kulkarni AP (2020) Is a problem shared, a problem halved? Not always! The novel coronavirus covid-19 outbreak. Indian Journal of Critical Care Medicine: Peer-reviewed, Official Publication of Indian Society of Critical Care Medicine 24: 88-89. [ Ref ]
USDA (2020) Frequently asked questions: Can I become sick with coronavirus (covid-19) from food? [ Ref ]
Wu Z, McGoogan JM (2020) Characteristics of and important lessons from the coronavirus disease 2019 (covid-19) outbreak in china: Summary of a report of 72 314 cases from the chinese center for disease control and prevention. The Journal of the American Medical Association. [ Ref ]
Jain V, Yuan JM (2020) Systematic review and meta-analysis of predictive symptoms and comorbidities for severe covid-19 infection. medRxiv. [ Ref ]
Brake SJ, Barnsley K, Lu W, McAlinden KD, Eapen MS et al. (2020) Smoking upregulates angiotensin-converting enzyme-2 receptor: A potential adhesion site for novel coronavirus sars-cov-2 (covid-19). Multidisciplinary Digital Publishing Institute 9: 841. [ Ref ]
Leung JM, Yang CX, Tam A, Shaipanich T, Hackett TL, et al. (2020) Ace-2 expression in the small airway epithelia of smokers and copd patients: Implications for covid-19. European Respiratory Journal 55: 2000688. [ Ref ]
Barnett ML, Grabowski DC (2020) Nursing homes are ground zero for covid-19 pandemic. Presented at JAMA Health Forum, American Medical Association 1: e200369-e69. [ Ref ]
Moriarty LF (2020) Public health responses to covid-19 outbreaks on cruise ships-worldwide, February-march 2020. MMWR. Morbidity and Mortality Weekly Report 69: 347-352. [ Ref ]
Wikipedia (2020) Coronavirus pandemic on naval ships. [ Ref ]
Zimmermann P, Curtis N (2020) Coronavirus infections in children including covid-19. Pediatr Infect Dis J 39: 355-368. [ Ref ]
Sutton D, Fuchs K, D’Alton M, Goffman D (2020) Universal screening for sars-cov-2 in women admitted for delivery. New England Journal of Medicine 382: 2163-2164. [ Ref ]
Jones VG, Mills M, Suarez D, Hogan CA, Yeh D, et al. (2020) Covid-19 and kawasaki disease: Novel virus and novel case. Hospital Pediatrics 10: 537-540. [ Ref ]
Riphagen S, Gomez X, Gonzalez-Martinez C, Wilkinson N, Theocharis P (2020) Hyperinflammatory shock in children during covid-19 pandemic. The Lancet 395: 1607-1608. [ Ref ]
Harahsheh AS, Dahdah N, Newburger JW, Portman MA, Piram M, et al. (2020) Missed or delayed diagnosis of kawasaki disease during the 2019 novel coronavirus disease (covid-19) pandemic. The Journal of Pediatrics 222: 261-262. [ Ref ]
Li X, Xu S, Yu M, Wang K, Tao Y, et al. (2020) Risk factors for severity and mortality in adult covid-19 inpatients in wuhan. Journal of Allergy and Clinical Immunology 146: 110-118. [ Ref ]
Ryan JJ, Melendres L, Zamanian R, Oudiz R, Chakinala MM, et al. (2020) Express: Care of patients with pulmonary arterial hypertension during the coronavirus (covid-19) pandemic. Pulm Circ. [ Ref ]
Owen WF, Carmona R, Pomeroy C (2020) Failing another national stress test on health disparities. The Journal of the American Medical Association. [ Ref ]
Moore J, Ricaldi J, Rose C (2020) Disparities in Incidence of COVID-19 Among Underrepresented Racial/Ethnic Groups in Counties Identified as Hotspots During June 5–18, 2020 — 22 States, February–June 2020. Morbidity and Mortality Weekly Report. [ Ref ]
New York State (2020) Covid-19 tracker. [ Ref ]
Cao Y, Li L, Feng Z, Wan S, Huang P, et al. (2020) Comparative genetic analysis of the novel coronavirus (2019-ncov/sars-cov-2) receptor ace2 in different populations. Cell Discovery 6: 11. [ Ref ]
Yancy CW. (2020) Covid-19 and African Americans. The Journal of the American Medical Association. [ Ref ]
Liu W, Zhang Q, Chen J, Xiang R, Song H, et al. (2020) Detection of covid-19 in children in early january 2020 in wuhan, china. N Engl J Med 382:1370-1371. [ Ref ]
CDC (2020) COVID-19 Response Team. Severe outcomes among patients with coronavirus disease 2019 (covid-19)-united states, february 12–march 16, 2020. Morbidity and Mortality Weekly Report 69: 343-346. [ Ref ]