Journal Name: Journal of Biomedical Research and Reviews
Article Type: Review
Received date: 03 September, 2018
Accepted date: 05 September, 2018
Published date: 2021-03-21
Citation: Alzaibak MAA, Kassab YW (2018) Comparison between creatinine-based equations among diabetic nephropathy patients. J Biomed Res Rev Vol: 1, Issu: 2 (26-30).
Copyright: © 2018 Alzaibak MAA. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Background: Diabetes is a leading cause of chronic kidney disease (CKD). Using some creatinine-based equations is the most widely distributed method in evaluating the kidney function. it can give an inaccurate estimated result, especially in individuals with typical renal function Modification of Diet in Renal Disease (MDRD) formula, Cockcroft-Gault (CG) equation, and the newly published formula of Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) equation are widely used during estimation the kidney function practice.
Method: A total of 31 studies have been included in the final review. These studies comparing three creatinine-based formulas (MDRD, CG, And CKD-EPI equations) among diabetic nephropathy (DN) patients. The studies have been downloaded from PubMed, ScienceDirect, and google scholar databases.
Results: CG equation overestimates the renal function among diabetes patients especially in lower glomerular filtration rate (GFR) levels. In addition, the CG equation overestimates the renal function in healthy patients more than the diabetic patients. In contrast, both CKD-EPI and MDRD formulas are underestimating the renal function, especially in higher GFR levels. CKD-EPI formula has been achieved better than MDRD and CG formulas in the renal function estimation. While CG performed better than CKD-EPI and MDRD formulas among obese diabetic nephropathy people.
Conclusion: The estimation of renal function by creatinine-based equation can be overestimated or underestimated the gold standard (mGFR).
Keywords
CG, Cockcroft-gault, Renal function estimation, MDRD, Modification of diet in renal disease, CKD Epidemiology Collaboration, CKD-EPI, Creatinine based equations, Diabetes, Diabetic nephropathy.
Abstract
Background: Diabetes is a leading cause of chronic kidney disease (CKD). Using some creatinine-based equations is the most widely distributed method in evaluating the kidney function. it can give an inaccurate estimated result, especially in individuals with typical renal function Modification of Diet in Renal Disease (MDRD) formula, Cockcroft-Gault (CG) equation, and the newly published formula of Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) equation are widely used during estimation the kidney function practice.
Method: A total of 31 studies have been included in the final review. These studies comparing three creatinine-based formulas (MDRD, CG, And CKD-EPI equations) among diabetic nephropathy (DN) patients. The studies have been downloaded from PubMed, ScienceDirect, and google scholar databases.
Results: CG equation overestimates the renal function among diabetes patients especially in lower glomerular filtration rate (GFR) levels. In addition, the CG equation overestimates the renal function in healthy patients more than the diabetic patients. In contrast, both CKD-EPI and MDRD formulas are underestimating the renal function, especially in higher GFR levels. CKD-EPI formula has been achieved better than MDRD and CG formulas in the renal function estimation. While CG performed better than CKD-EPI and MDRD formulas among obese diabetic nephropathy people.
Conclusion: The estimation of renal function by creatinine-based equation can be overestimated or underestimated the gold standard (mGFR).
Keywords
CG, Cockcroft-gault, Renal function estimation, MDRD, Modification of diet in renal disease, CKD Epidemiology Collaboration, CKD-EPI, Creatinine based equations, Diabetes, Diabetic nephropathy.
Introduction
Diabetic nephropathy (DN) has emerged as a global problem in the community health with growing prevalence [1]. Making matters worse, Diabetes mellitus (DM) is the prime causative for end-stage renal disease (ESRD) and renal failure. Therefore, precise assessment of kidney function among DM patients is needed [2]. There are Numerous equations for estimation the renal function, those equations have been used for glomerular filtration rate (GFR) or creatinine clearance (CrCl) evaluation, However, there is a lack of universality across the multiple clinical situations encountered by the health care providers [3]. Using some creatinine-based equations is the most widely distributed method in evaluating the kidney function. However, it can give inaccurate estimated results, especially in individuals with typical renal function [4]. Creatinine-based equations are regularly performed for estimation the renal function because of being both practical and cheap. These formulas are used for ESRD detecting, monitoring of the disease progression, and prognosis prediction [5]. Modification of Diet in Renal Disease (MDRD) formula, Cockcroft-Gault (CG) equation, and the newly published formula of Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) equation are widely used during estimation the kidney function practice [6].
Research Methodology
This review article comparing between creatinine-based formulas (MDRD, CKD-EPI, CG equations) among diabetic nephropathy (DN) patients. After searching on online databases (ScienceDirect, PubMed, And Google scholar), 34 studies were found comparing between creatinine-based equations in DN patients. Three studies were excluded because the full text was not in the English language. In the review study, 31 studies were included. All the included studies were in English and published between 2010 and 2018. Keywords (such as diabetes, diabetic nephropathy, CKD, Chronic kidney disease, renal function estimation, glomerular filtration rate, GFR, MDRD, CKD Epidemiology Collaboration, CG, CrCl, Cockcroft-gault, Cr clearance, modification of diet in renal disease, CKD-EPI, Creatininebased equations) were used with different combinations.
Comparison between MDRD and CKD-EPI Equations
Table 1 shows the comparison between MDRD and CKDEPI formulas among DN patients.
Table 1: Comparison between MDRD and CKD-EPI formulas among DN patients.
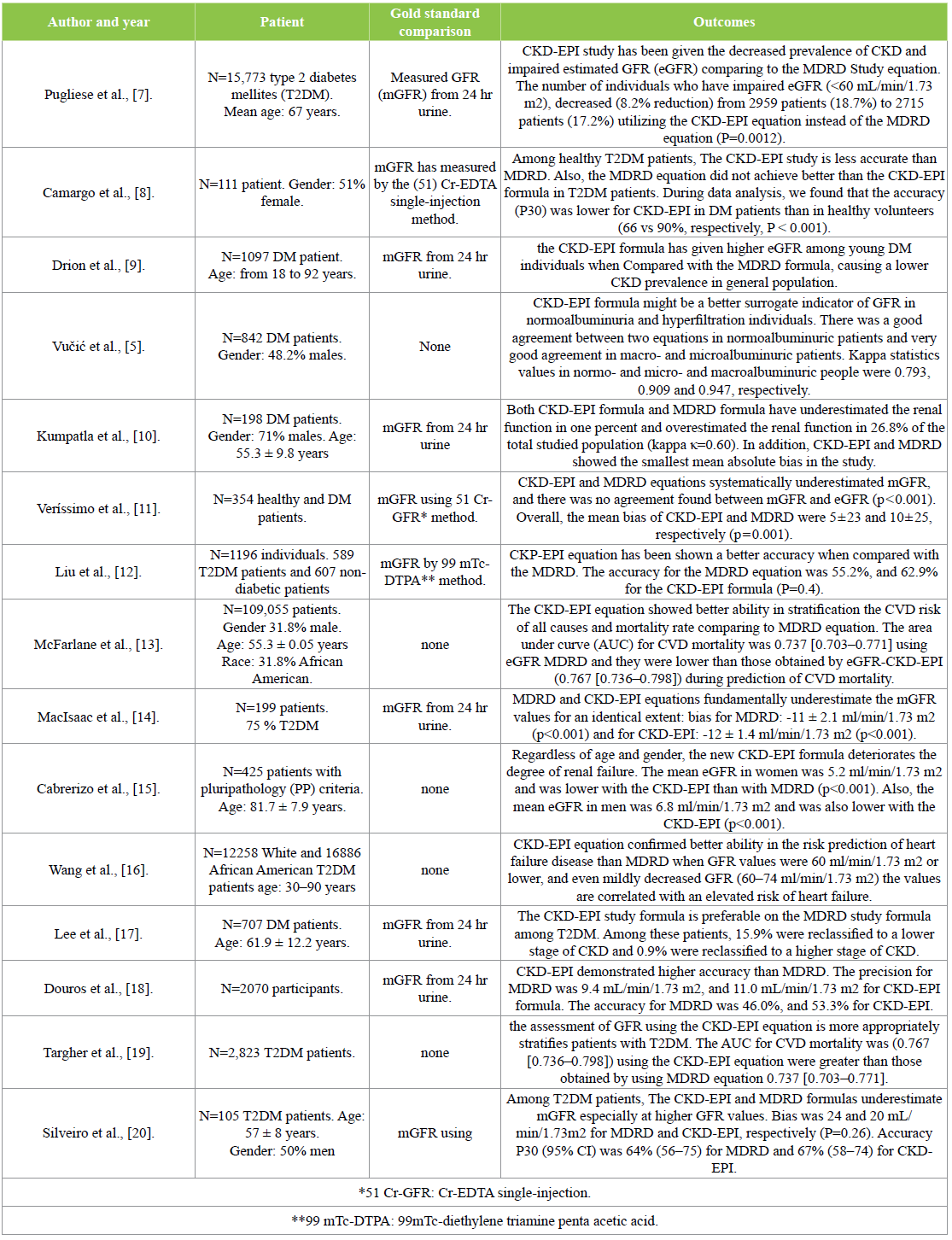
Discussion: Based on the outcomes of the compared studies among DN patients, CKD-EPI and MDRD equations both of them underestimate the renal function when compared with mGFR standard values [11,14,20]. These equations can enhance the underestimation of the renal function particularly at higher GFR values and chronic kidney disease (CKD) stages [20]. In terms of evaluating the accuracy of the CKD-EPI, CKD-EPI formula has been shown a better accuracy and precision when compared to MDRD study during the estimation of the renal function [17-19]. Furthermore, CKD-EPI formula gave more accurate assessment among healthy patient when compared to DN patients [8].
A new study has been published, check the abilities of both equations in predicting the progression of cardiovascular disease (CVD). This study found that the CKD-EPI equation showed better ability in stratification the CVD risk of all causes and mortality rate [13]. Additional study has been done, showing the abilities of the equations in the prediction of the heart failure risk. The study showed that the CKD-EPI equation confirmed better ability in the risk prediction of the heart failure disease [16].
Finally, CKD-EPI study gave higher eGFR estimates among young DM people when Compared with MDRD equation [9]. Therefore, it leads to the lower prevalence of impaired renal function among DN population and lower prevalence of CKD, that when comparing it with the MDRD [7].
Comparison between MDRD and CG Equations
Table 2 explains the differentiation between MDRD and CG equations among DN patients.
Table 2: Differentiation between MDRD and CG equations among DN patients.
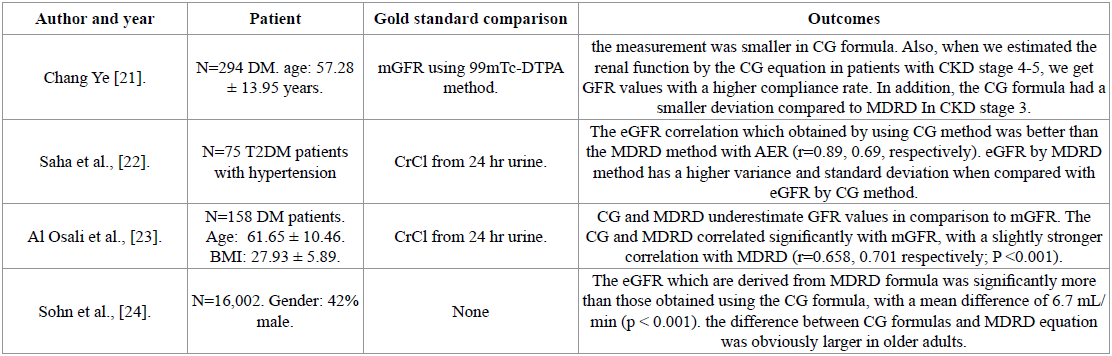
Discussion: The comparison studies confirmed that CG and MDRD underestimate the renal function (eGFR) in comparison with the golden standard, CrCl measured by using 24 hr urine [23]. In addition, a large study has done on 16,002 patients. That study confirmed that the obtained eGFR values MDRD are higher than those obtained from the CG equation [24]. Finally, the GFR estimates values which are calculated by the CG equation has a smaller variance and standard deviation when compared to the GFR estimates which are calculated by the MDRD equation [22].
Comparison between MDRD, CKD-EPI, and CG Equations
Table 3 shows the studies that compare MDRD, CG, and CKD-EPI equations among DN patients.
Table 3: Study of comparison of MDRD, CG, and CKD-EPI equations among DN patients.
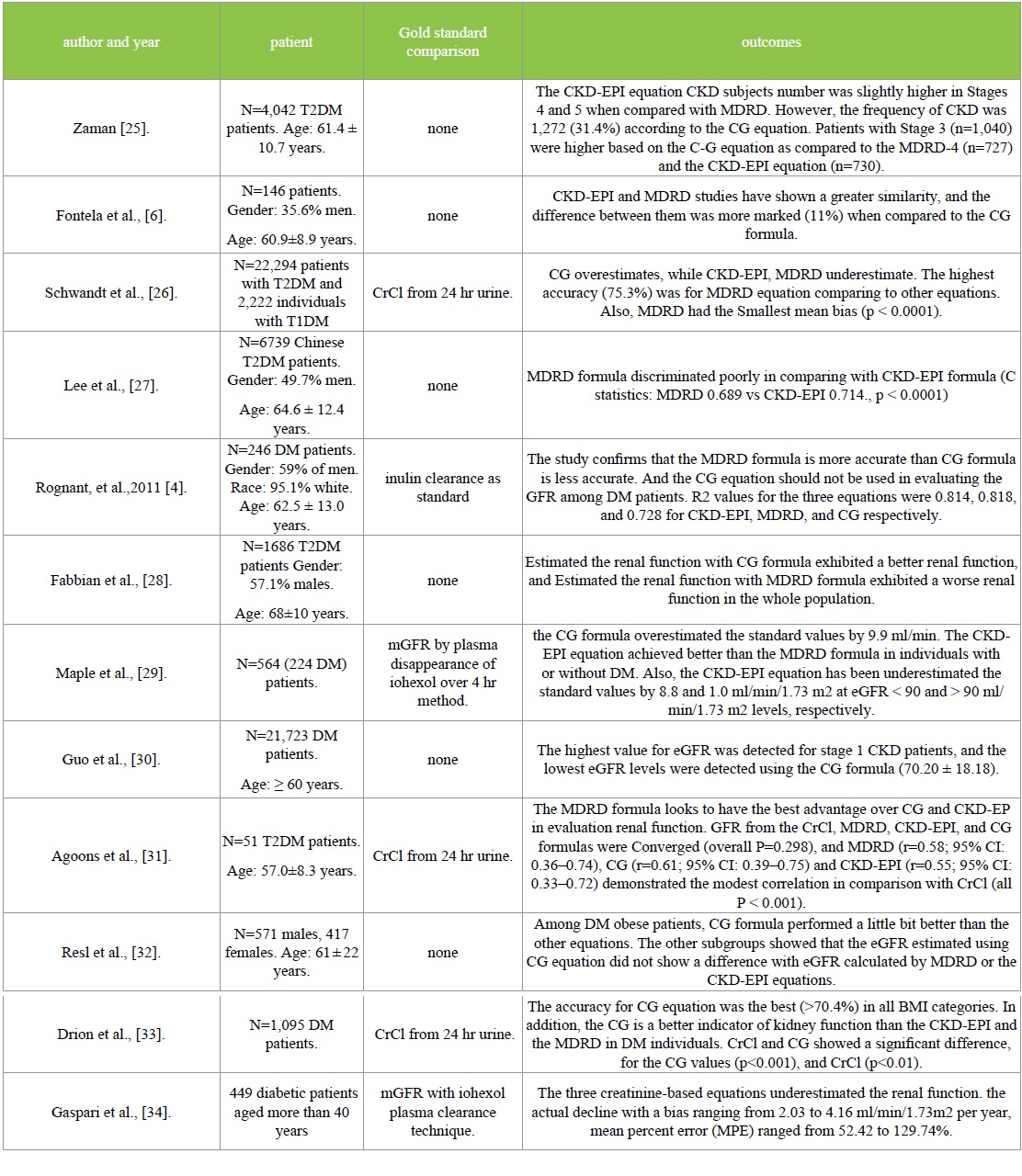
Discussion: Based on the studies result, among DN patients both CKDEPI and MDRD formulations underestimate the standard values (mGFR) while the CG equation overestimates it. CG equation overestimation increase in lower CKD stages especially in healthy patients [26, 26, 29, 34]. Furthermore, the CG equation showed the lowest levels of estimated GFR (eGFR) when compared with CKD-EPI and MDRD equations [30].
Based on the studies result, among DN patients both CKDEPI and MDRD formulations underestimate the standard values (mGFR) while the CG equation overestimates it. CG equation overestimation increase in lower CKD stages especially in healthy patients [26, 26, 29, 34]. Furthermore, the CG equation showed the lowest levels of estimated GFR (eGFR) when compared with CKD-EPI and MDRD equations [30].
In comparing the obtained values from three equations without using golden standard (mGFR), MDRD and CKDEPI demonstrated closer eGFR values for each other when compared with CG in DN patients. In addition, CG number of CKD patients was higher than MDRD and CKD-EPI formulas especially in higher CKD stages [6,25,30].
Some studies investigated the performance and the accuracy for all the equations. Those studies found that the estimated GFR values using the CG equation are less accurate than MDRD while CKD-EPI formula has higher accuracy than MDRD equation [4,27,29]. Otherwise, two studies one of them is a large cohort study done on DN patients (n=22,294 T2DM patients) showed that MDRD is more accurate and have better advantages over CG and CKD-EPI equations [26,31].
Although the CG equation did not show a good accuracy and precision among DN patients, it showed a better accuracy in obese DN patients when compared to other equations. Two studies improved that equation achieved slightly better than CKD-EPI and MDRD in estimation the renal function among DM obese patients [32,33].
Conclusion
The measurement of eGFR plays the main role in the monitoring and detection of renal disease among DN patients. Therefore, the estimation of true renal function in the general population plays a significant role. All the studies showed that creatinine-based equations can overestimate or underestimate the gold standard (mGFR) during the estimation of the renal function. The variation in estimates depends on the number of the risk factors for CKD such as age, sex, race, etc. MDRD and CKD-EPI formulas can enhance the underestimation of the renal function particularly at higher GFR values and chronic kidney disease (CKD) stages [20]. While the CG equation overestimates the mGFR especially at lower GFR levels, especially among healthy individuals [22].
In terms of the accuracy and precision, the accuracy of creatinine-based formulas is still unclear. CKD-EPI equation showed a better accuracy than the other equations in most of the studies. Otherwise, a large cohort study (N= 22,294) showed that the MDRD equation showed the highest accuracy compared to the other equations [26]. In contrast, the CG equation did not show a good accuracy in most of the studies but it exhibited a better accuracy on the obese DN patients [32,33].
Compliance with Ethical Standards
Conflict of Interest: Author A declares that he has no conflict of interest. Author B declares that he has no conflict of interest.
Ethical approval: This article does not contain any studies with human participants or animals performed by any of the authors.
There is no references


