Journal Name: Journal of Biomedical Research and Reviews
Article Type: Research
Received date: 01st-March-2018
Accepted date: 16th-April-2018
Published date: 23rd-April-2018
Citation: Takao K, Norihiko K, Yuta M, Masaru H, Hiroyasu I, et al. (2018) Comparison of Bone Quality in Patients with or Without Weekly Injection of Teriparatide to Improve Bone ingrowth after Cementless Total Knee Arthroplasty. J Biomed Res Rev 1: 1 (25-30).
Copyright: © 2018 Takao K, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Background: In the present study, the effectiveness of postoperative a once-weekly teriparatide for the management of this decline, with the specific objective of testing the hypothesis that teriparatide administration following TKA promotes bone ingrowth between the joint prosthesis and cancellous bone, was investigated.
Methods: The subjects were 40 patients who underwent cementless TKA (CR-type) for treatment of medial gonarthrosis. The implemented device was a trabecular metal modular tibia. All cases in which postoperative simple X-ray examination showed malalignment or a radiolucent line was excluded from the analysis. For determination of ossification density 3, 6, and 9,12 months postoperatively a phantom consisting of a cylinder composed of a material corresponding to cortical bone and filled with a material having a bone density corresponding to cancellous bone was placed under the knee, and imaging was then performed by MDCT. 20 cases (group A), the once-weekly teriparatide formulation was injected subcutaneously/hypodermically for 48 weeks, beginning 1 week postoperatively, with no administration of any other therapeutic agent for osteoporosis. In the other 20 cases (group B), no teriparatide or any other osteoporosis therapeutic agent was administered. The structural parameters subjected to analysis were bone mineral content/total volume (BMC/TV). Region of interest(ROI) was divided into 6 legions [ROI 1 (medial), ROI 2 lateral, ROI 3 (anteromedial), ROI 4 (posteromedial), ROI 5 (anterolateral), and ROI 6 (posterolateral)].
Results: The BMC/TV was differed significantly between the two groups at 6, 9and 12 months postoperatively in ROI 1,3 and 4. There was not differed significantly between the two groups in ROI 2,5and 6. In ROIs 1, 3, and 4, ossification density was higher with once-weekly teriparatide administration.
Conclusion: Teriparatide treatment promotes bone ingrowth between and the joint prothesis and medial cancellous bone after cementless total knee arthroplasty.
Keywords
Knee arthroplasty, Teriparatide, Tibia, Ligament, Cancellous bone.
Abstract
Background: In the present study, the effectiveness of postoperative a once-weekly teriparatide for the management of this decline, with the specific objective of testing the hypothesis that teriparatide administration following TKA promotes bone ingrowth between the joint prosthesis and cancellous bone, was investigated.
Methods: The subjects were 40 patients who underwent cementless TKA (CR-type) for treatment of medial gonarthrosis. The implemented device was a trabecular metal modular tibia. All cases in which postoperative simple X-ray examination showed malalignment or a radiolucent line was excluded from the analysis. For determination of ossification density 3, 6, and 9,12 months postoperatively a phantom consisting of a cylinder composed of a material corresponding to cortical bone and filled with a material having a bone density corresponding to cancellous bone was placed under the knee, and imaging was then performed by MDCT. 20 cases (group A), the once-weekly teriparatide formulation was injected subcutaneously/hypodermically for 48 weeks, beginning 1 week postoperatively, with no administration of any other therapeutic agent for osteoporosis. In the other 20 cases (group B), no teriparatide or any other osteoporosis therapeutic agent was administered. The structural parameters subjected to analysis were bone mineral content/total volume (BMC/TV). Region of interest(ROI) was divided into 6 legions [ROI 1 (medial), ROI 2 lateral, ROI 3 (anteromedial), ROI 4 (posteromedial), ROI 5 (anterolateral), and ROI 6 (posterolateral)].
Results: The BMC/TV was differed significantly between the two groups at 6, 9and 12 months postoperatively in ROI 1,3 and 4. There was not differed significantly between the two groups in ROI 2,5and 6. In ROIs 1, 3, and 4, ossification density was higher with once-weekly teriparatide administration.
Conclusion: Teriparatide treatment promotes bone ingrowth between and the joint prothesis and medial cancellous bone after cementless total knee arthroplasty.
Keywords
Knee arthroplasty, Teriparatide, Tibia, Ligament, Cancellous bone.
Introduction
The parathyroid hormone drug PTH 1-34 (teriparatide) is a formulation produced in Japan by chemical synthesis of the N-terminal 34 amino acids comprising the active region of the human parathyroid hormone (PTH). In clinical use in Japan since 2011 as a once-weekly injection formulation of teriparatide (Teribon; Asahi Kasei Pharma Corporation, Tokyo, Japan), it has, by its effect of promoting new bone formation, reduced the incidence of new bone fractures in osteoporosis patients. It also promotes ossification remodeling and induces fibrous bone replacement by lamellar bone and its transformation to cortical bone. Various groups have reported that teriparatide effectively promotes fracture healing, but its effects during the early stages following surgical stabilization of implants have not yet been confirmed.
The bone mass of the proximal tibia has been reported to decline following total knee arthroplasty (TKA), apparently as an effect of shear-stress shielding, and it has also been reported that the loss ratio is particularly marked during the first postoperative year. The aim of this study is to compare of bone quality in patients with or without weekly injection of teriparatide after cementless TKA.
Materials
The subjects were 40 patients who underwent cementless TKA (CR-type) for treatment of medial gonarthrosis between October 2012 and January 2013. The implanted device was a trabecular metal modular tibia (Nexgen CR-Flex; Zimmer, Warsaw, Indiana) having tantalum as its main component. In 20 of the 40 cases (group A), the once-weekly teriparatide formulation was injected subcutaneously/hypodermically for 48 weeks, starting from 1-week postoperation, with no administration of any other therapeutic agent for osteoporosis [1,2]. In the other 20 cases (group B), no teriparatide or any other osteoporosis therapeutic agent was administered. The two groups were matched by sex, age, BMI, preoperative extension and flexion angles, and Knee Society scores [3-6].
Surgical technique
In all cases, the TKA surgical procedure was performed by one author (T. K.) and was minimally invasive, with a skin incision of 8-11 cm and retention of the posterior cruciate ligament. Patient walking was permitted from the day following the operation.
Methods
Any case in which postoperative simple X-ray examination showed malalignment or a radiolucent line was excluded from the analysis.For determination of ossification density 3, 6, and 9,12 months postoperatively, a phantom consisting of a cylinder composed of a material corresponding to cortical bone and filled with a material having a bone density corresponding to cancellous bone was placed under the knee, and imaging was then performed by multi detector-row computed tomography (MDCT). From the obtained images, the cancellous trabecular structure was visualized three-dimensionally with 3D osteomorphometry software (TRI/3D-BON64; RATOC System Engineering Co., Ltd., Tokyo, Japan), and the structural parameters were calculated. The structural parameters subjected to analysis were those recommended by the American Society for Bone and Mineral Research: bone mineral content/total volume (BMC/TV), representing three-dimensional bone mineral density (BMD), and bone volume/total volume (BV/TV), representing mineralized bone volume as a percentage of total volume.
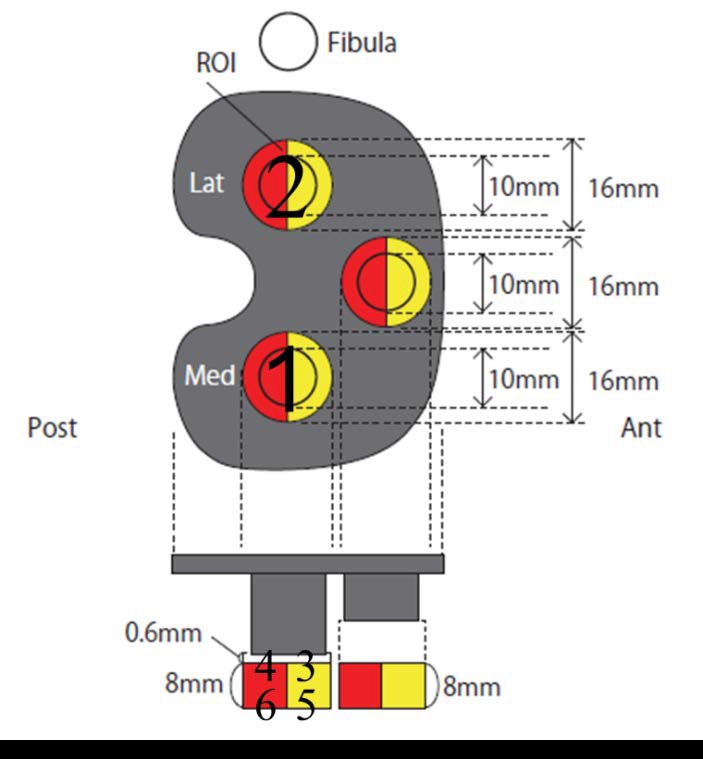
In the assessment of BMD by MDCT imaging of the proximal tibia, the joint prosthesis itself generated artifacts, which prevented accurate delineation. Therefore, the overall region was divided into 6 regions of interest (ROIs), consisting of two cylindrical volumes, each 16 mm in diameter and 8 mm in height, with their tops 0.6 mm below the medial or lateral peg, with each further divided into 2 half-cylinders. [ROI 1 (medial), ROI 2 (lateral), ROI 3 (anteromedial), ROI 4 (posteromedial), ROI 5 (anterolateral), and ROI 6 (posterolateral)] (Figure 1).
Figure 1: 6 regions of interest (ROIs) under the peg of the tibial component. Regions 1 (medial) and 2 (lateral), and 3 (anteromedial), 4 (posteromedial), 5 (anterolateral), and 6 (posterolateral).
Statistical analysis
Statistical analysis was performed for relative change in ossification density, immediately and 3, 6, and 9,12 months postoperatively in each of the two groups by the Mann- Whitney U test and for comparison between the two groups by the paired t-test. P values of less than 0.05 were deemed significant. This study was approved by the Institutional Review Board of our hospital, and informed consent was received from each patient who participated.
Results
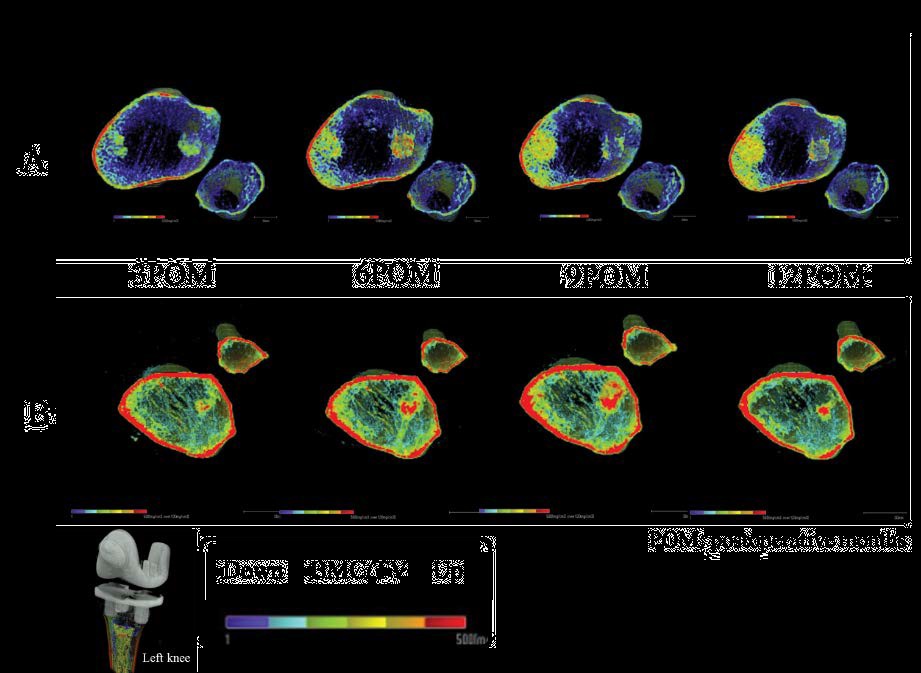
There were no significant differences between the two groups in preoperative age, sex, BMI, extension or flexion angle, or Knee Society score (knee function) (Table 1). Postoperatively, there were no significant differences between the two groups in Knee Society X-ray evaluation, extension or flexion angle, or Knee Society score (knee function) (Table 2). The axial 3D-MDCT images in Figure 2 were obtained for a 77-year-old group A woman age and a 78-year-old group B man. In the immediately postoperative images, bone rarefaction (porosity) was clearly more advanced in the group A patient than in the group B patient. The ossification density in the lateral tibial plateau increased until 9 months postoperatively and then declined in the group B patient, but in the group A patient, it clearly continued to increase beyond 9 months postoperatively.
Table 1: Pre-operative of patient’s data in the once-weekly teriparatide and no teriparatide or any other osteoporosis therapeutic agent groups.
| Group | A (n=20) | B (n=20) | Mean ± SD |
|---|---|---|---|
| Age (yr) | 74.13 ± 7.40 | 77.13 ± 6.15 | n.s |
| Man/Female | 4/16 | 4/16 | n.s |
| BMI (Kg/m2) | <26.96 ± 4.21/td> | 24.80 ± 4.21 | n.s |
| Knee society score (Points) | 13.88 ± 8.31 | 20. 13 ± 12.76 | n.s |
| Knee function range of motion (deg) | 62.50 ± 11.95 | 52.50 ± 18.52 | n.s |
| Extension | 11.88 ± 5.94 | 12.50 ± 4.63 | n.s |
| Flexion | Flexion | 119.38 ± 4.17 | n.s |
Table 2: Post-operative of patient’s data in the once-weekly teriparatide and no teriparatide or any other osteoporosis therapeutic agent groups.
| Group | A (n=20) | B (n=20) | Mean ± SD |
|---|---|---|---|
| Knee society score (Points) | 88 ± 9.41 | 8218 ± 10.46 | n.s |
| Knee Function | 79.38 ± 10.16 | 78.49 ± 9.54 | n.s |
| Ranfe of motion (deg) | |||
| Extension | 1.25 ± 9.43 | 0 ± 0 | n.s |
| Flexion | 129.38 ± 9.43 | 135.63 ± 6.23 | n.s |
| Post knee society (deg) | |||
| Femoreal angle (α) | 88.88 ± 1.41 | 91.11 ± 1.08 | n.s |
| Femoreal angle (β) | 90.45 ± 1.62 | 90.18 ± 1.42 | n.s |
| Tibial angle (γ) | 0.82 ± 2.42 | 0.81 ± 3.47 | n.s |
| Tibial angle (δ) | 87.71 ± 1.44 | 87.70 ± 1.46 | n.s |
Figure 2: The axial 3D-MDCT images in A. 77-year-old woman B. 78-year-old man. In the group B patient, the ossification density in the lateral tibial plateau increases during the first 9 months postoperatively and then decreases, whereas in the group A patient, it increases in the medial tibial plateau throughout the observation period up to and including 12 months postoperatively.
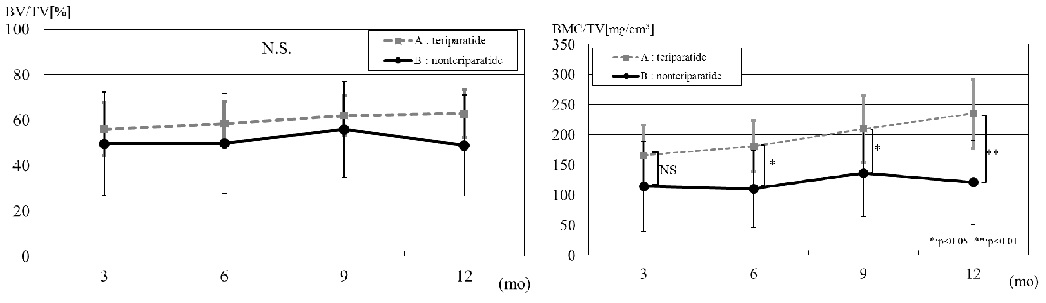
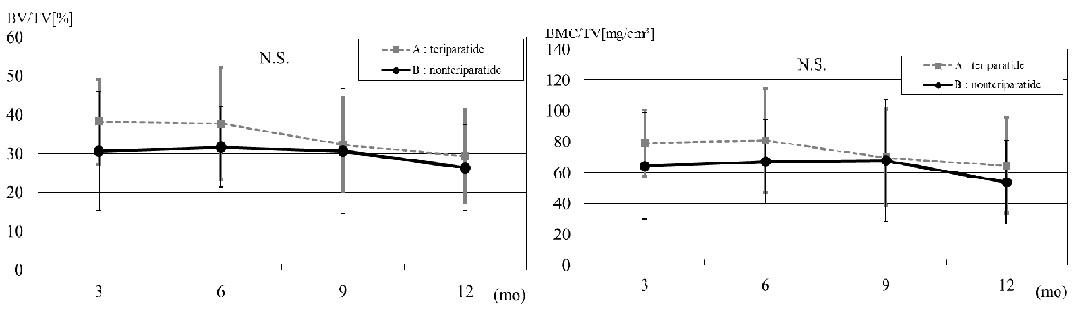
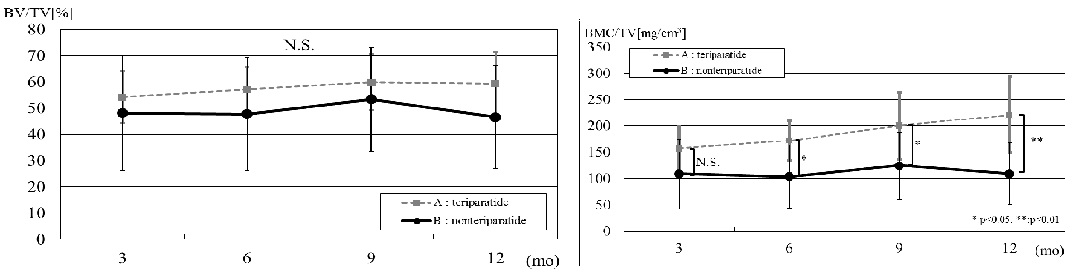
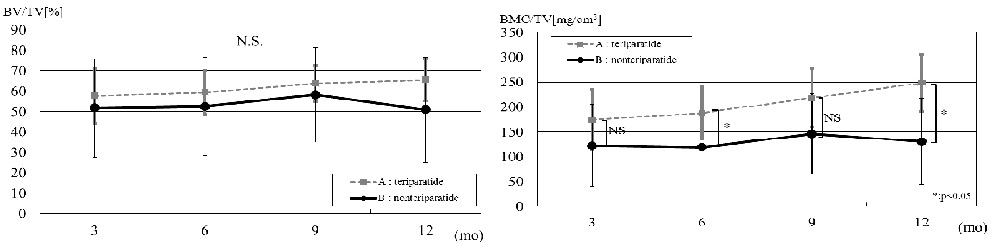
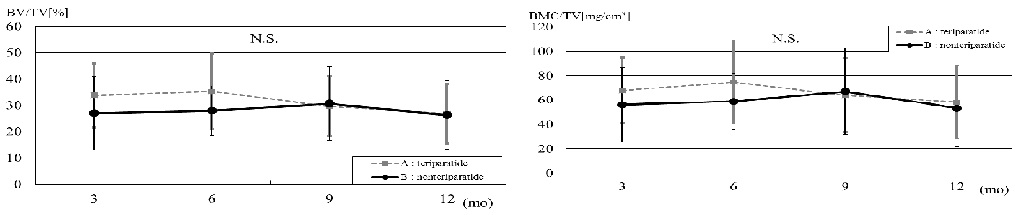
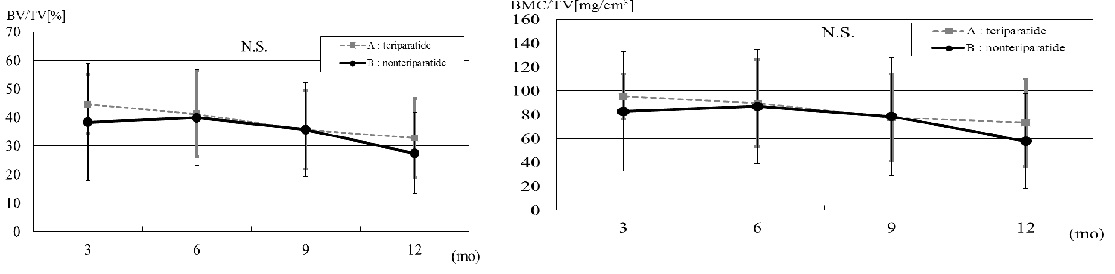
The BV/TM values in ROI 1 (medial) increased throughout the postoperative period in group A and declined after 6 months postoperatively in group B, though there were no significant differences between the groups. The BMC/TV in ROI 1, however, differed significantly between the two groups at 6, 9and 12 months postoperatively, with a markedly higher increase in group A than in group B at 12 months postoperatively (Figure 3). In ROI 2 (lateral), postoperative BV/TV and BMS/TV both showed a decreasing trend, with no significant difference between the groups (Figure 4). In ROI 3 (anteromedial) and ROI 4 (posteromedial), as in ROI 1, significant differences between the two groups were found at postoperative 6,9 and 12 months in BMC/TV but not in BV/TM. The difference between the groups in BMC/TV at 12 months postoperatively was markedly higher in ROI 3 (p<0.01) than in ROI 4 (Figure 5, 6). In ROI 5 (anterolateral) and ROI 6 (posterolateral), as in ROI 2, no significant differences were found between the two groups. In these two regions, the ossification density declined from the immediate postoperative level with no apparent increase, but in group A, the decline in BV/TV and BMC/TV ended after 9 months postoperatively (Figure 7, 8). During the period of observation, no radiolucent line was found around the pegs of the tibial component, and no bone fracture was found around the knee prosthesis.
Figure 3: The relative change in bone volume/total volume (BV/TV) and bone mineral contents/total volume (BMC/TV) in ROI 1. BMC/TV is significantly higher in group A than in group B at 6 and 9 months postoperatively (*p<0.05) and particularly higher at 12 months postoperatively (**p<0.01).
Figure 4: The relative change in bone volume/total volume (BV/TV) and bone mineral contents/total volume (BMC/TV) in a region of interest (ROI 2). Both BV/TV and BMC/TV tend to decline over time in both groups, with no significant difference between the two groups.
Figure 5: The relative change in bone volume/total volume (BV/TV) and bone mineral contents/total volume (BMC/TV) in a region of interest (ROI 3). BMC/TV is significantly higher in group A than in group B at 6, 9, and 12 months postoperatively (*: p<0.05, **: p<0.01).
Figure 6: The relative change in bone volume/total volume (BV/TV) and bone mineral contents/total volume (BMC/TV) in a region of interest (ROI 4). BMC/TV is significantly higher in group A than in group B at 6,9 and 12 months postoperatively (*p<0.05).
Figure 7: The relative change in bone volume/total volume (BV/TV) and bone mineral contents/total volume (BMC/TV) in regions of interest (ROI 5). No significant difference in BV/TV or BMC/TV is seen between the two group.`
Figure 8: The relative change in bone volume/total volume (BV/TV) and bone mineral contents/total volume (BMC/TV) in regions of interest (ROI 6). No significant difference in BV/TV or BMC/TV is seen between the two groups.
Discussion
Total knee arthroplasty (TKA) is performed with either cemented or cementless fixation. Cemented fixation may pose problems related to cement toxicity, residual cement particles, and loosening due to cement degradation. In cementless fixing, progress has been made in the development of technologies that strengthen bone ingrowth to joint prostheses through treatment of their metal surfaces, and robust fixation can be expected if biological fixation is successful. Good results have been reported for cementless TKA with hydroxyapatite-coated prosthesis components [7,8]. The porous tantalum of the joint prosthesis used in the present study resembles cancellous bone and is characterized by a high coefficient of friction [9], high porosity, and low elastic modulus. Various reports have been published on the motion of tibial components as found by radio stereometric analysis (RSA). Stilling et al [10], reported that trabecular metal is migratory at 3 months postoperatively but stable at 1 year. Dunbar et al [11], similarly reported that tibial components migrate initially but then stabilize, and they noted that migration tended to be greater in patients with low bone density.
In the present study, the possibility of obtaining higher bone strength between the tibial component and cancellous bone by postoperative administration of onceweekly teriparatide was investigated. Bone strength is reportedly dependent on bone density and bone quality [12], which in turn is governed by the properties of the bone material and structure (microstructure). Abnormalities in bone microstructure tend to occur under accelerated bone resorption, and most osteoporosis treatment has been performed with the objective of inhibiting bone resorption, with bisphosphonate and selective estrogen receptor modulators (SERMs) used widely for this purpose. Teriparatide, the parathyroid hormone formulation investigated in the present study, improves bone density, microstructure, and material properties by a mechanism different from those of bone resorption inhibitors and has been recommended for increasing bone strength in the first treatment drug for osteoporosis [13].
The Incidence of side effects for weekly Parathyloid hormone is relatively high compared vitamin D and calcium preparations, the bone resorption inhibitor, but it is a mild side effects transiently. In Phase III study Japanese, side effects were observed in 127 in 290 cases in treating with the treatment of weekly parathyroid hormone. The main side effect was 54 cases (18.6%) in nausea, 25 cases (8.6%) of vomiting, 22 cases (7.6%) in headache, 18 cases (6.2%) in fatigue, but the side effects have been observed 52 (18.1%) in 288 cases of the placebo group too. One of the reasons for side effects appeared in both groups was a long-term follow up period of 72 weeks. The another reason that complaint was increased every time of examination by coming to the hospital once a week.
Once-weekly teriparatide, unlike daily administration, has been found to increase bone mass (BV/TV) through inhibition of bone resorption concurrently with bone formation [14,15]. It has been reported that bone density and tibial component migration after total knee arthroplasty are strongly correlated, and that the decrease in proximal tibial bone density is most marked during the first 6 months postoperatively, with the decrease ranging up to 23% [16]. In the cases reported in the present study, in group B (no teriparatide administered) the BMC/TV in ROIs 1, 3, and 4 increased until 9 months postoperatively and declined thereafter, but group A (teriparatide administered) showed a trend of continuing increase after 9 months postoperatively, with a significant difference between the two groups. In contrast, the BV/TV in these ROIs increased slowly in group A, with no significant difference from group B. In ROIs 1, 3, and 4, and thus in the medial tibia, ossification density was higher with once-weekly teriparatide administration. In has recently been reported that tibial component placement with mild varus as the neutral position may be optimal, although the position varies with the level of patient activity and the presence or absence of osteoporosis [17] and Zhao, et al [18] repoted that the force is massive more medial side from the latera sidel, and even alignment of neutral alignment is measured in the simulation which measured force to be added to component postoperatively. This suggests that stress tends to concentrate on the medial tibial plateau, with once-weekly teriparatide accordingly acting on that region and thus leading to an early increase there (ROIs 1, 3, and 4) in the strength of implant fixation found with once-weekly teriparatide in the present study. In the lateral regions (ROIs 2, 5, and 6), in contrast, no significant difference in either BMC/TV or BV/TV was found between the groups with and without once-weekly teriparatide, though it must be noted that the postoperative period of observation in this study was rather short. Also noteworthy in this regard is the apparent effect of once-weekly teriparatide in group A after 9 months postoperatively. In the short follow-up period of this study, in summary, the results indicate that postoperative onceweekly teriparatide promotes bone ingrowth between the tibial component and cancellous bone in cementless TKA.
Our study is its short follow-up period. Since the number of once-weekly teriparatide administrations is limited to a maximum of 72, it will be necessary to perform a study with a follow-up period of corresponding length.
Investigation of the possibility of further increasing the early fixation strength of joint prostheses by using teriparatide in combination with denosumab, the anti- RANKL inhibitor having the highest known inhibiting effect on bone resorption, would also be desirable, since a combination of these two drugs has recently been reported [19] to result in a large increase in bone density.
Conclusion
Once-weekly teriparatide treatment increases bone mass by promoting ossification to a rate that exceeds the rate of bone resorption, and our hypothesis that teriparatide promotes bone ingrowth the joint prosthesis after cementless total knee arthroplasty and medial cancellous bone was verified by the results of this study.
Jiang Y, Zhao JJ, Mitlak BH, Wang O, Genant HK, et al. (2003) Recombinant human parathyroid hormone (1-34) for 18 months increases cancellous bone structure. J Bone Miner Res 18: 1932-1941. [ Ref ]
Saito M, Marumo K, Kida Y, Ushiku C, Kato S, et al. (2011) Changes in the contents of enzymatic immature, mature, and non-enzymatic senescent cross-links of collagen after once-weekly treatment with human parathyroid hormone (1-34) for 18 months contribute to improvement of both strength in ovariectomized monkeys. Osteoporos Int 22: 2373- 2383. [ Ref ]
Sarri T, Uvehammer J, Carlsson L, Regner L, Karrholm J (2007) Joint area constraint had no influence on bone loss in proximal tibia 5years after total knee replacement. J Orthop Res 25: 798-803. [ Ref ]
Li MG, Nilsson KG (2000) Changes in bone mineral density at the proximal tibia after total knee arthroplasty: a 2-year follow-up of 28knees using dual enegy X-ray absorptiometry. J Orthop Res 18: 40-47. [ Ref ]
Petersen MM, Gehrchen PM, Ostgaars SE, Nielsen PK, Lund B (2005) Effect of hydroxyapatite-coated tibial components on changes in bone mineral density of the proximal tibia after uncemented total knee arthroplasty: a prospective randomized study using dual-enegy x-ray absorptiometry. J Arthroplasty 20: 516-520. [ Ref ]
Soininvaara TA, Miettinen HJ, Jurvelin JS, Suomalainen OT, Alhava EM, et al. (2004) Periprosthetic tibial bone mineral density changes after total knee arthroplasty:one-year follow-up study of 69 patients. Acta Orthop Scand 75: 600-605. [ Ref ]
Soininvaara TA, Miettinen HJ, Jurvelin JS, Suomalainen OT, Alhava EM, (2004) Periprosthetic femoral bone loss after total knee arthroplasty:1- year follow-up study of 69 patients. Knee 11: 297-302. [ Ref ]
Nelissen RG, Valster ER, Rozing PM (1998) The effect of hydroxyapatite on the micromotion of total knee prostheses; a prospective randomized double-blind study. J Bone Joint Surg Am 80: 1665-72. [ Ref ]
- Zhang Y, Ahn BP, Fitzpatrick CD, Heiner DA, Poggie AR, et al. (1999) Interfacial friction behavior; cancellous bone, cortical bone, and a novel porous tantalum biomaterial. J Musculoskelet Res 3: 245.
Stilling M, Madsen F, Odgaad A, Romer L, Anderson NT, et al. (2011) Superior fixation of pegged trabecular metal over screw fixed pegged porous titanium fiber mesh; a randomized clinical RSA study on cementless tibial components. Acta Orthop 82: 177-186. [ Ref ]
Dunbar MJ, Wilson DA, Hennigar AW, Amirault JD, Gross M, et al. (2009) Fixation of a trabecular metal knee arthroplasty components: a prospective randomized study. J Bone Joint Surg Am 91: 1578-1586. [ Ref ]
Osteoporosis prevention, diagnosis and therapy (2001) NIH consensus Development Panal on Osteoporosis Prevention, Diagnosis, and Therapy. JAMA 285: 785-795. [ Ref ]
Saito M, Mori S, Mashiba T, Komatsubara S, Marumo K (2008) Collagen maturity,glycation induced-pentosidine, and mineralization are increased following 3-year treatment with incadronate in dogs. Osteporos Int 19:1343-1354. [ Ref ]
Nakamura T, Sugimoto T, Nakano T, Kishimoto H, Ito M, et al. (2012) Randomized Teriparatide [human parathyloid hormone (PTH)1- 34] Once-Weekly Efficacy Research(TOWER) trial for examining the reduction in new vertebral fractures in subjects with primary osteoporosis and high fracture risk. J Clin Endocrinol Metab 97: 3097- 3106. [ Ref ]
Miki T, Nakatsuka K, Naka H, Masaki H, Imanishi Y, et al. (2004) Effect and safety of intermittent weekly administration of human parathyroid hormone 1-34 in patients with primary osteoporosis evaluated by histomorphometry and microstructural analysis of iliac trabecular bone before and after 1 year of treatment. J Bone Miner Metab 22: 569-576. [ Ref ]
Petersen MM, Jensen NC, Gehrchen PM, Nielsen PK, Nielsen PT (1996) The relation between trabecular bone strength and bone mineral density assessed by dual phonton and dual energy X-ray absorptiometry in the proximal tibia. Calcif Tissue Int 59: 311-314. [ Ref ]
Johan B, William C, Hilde V, Jan V (2012) The Chitranjan Ranawat Award ; Is Neutral Mechanical Alignment Normal for All Patients? The Consept of Constitutional Varus. Clin Orthop Relat Res 470: 45-53. [ Ref ]
Zhao D, Banks SA, D’Lima DD, Colwell CW Jr, Fregly BJ (2007) In vivo medial and lateral tibial loads during dynamic and high flextion activities. J Orthop Res 25: 593-602. [ Ref ]
Tsai JN, Uihlein AV, Lee H, Kumbhani R, Siwila-Sackman E, et al. (2013) Teriparatide and denosumab, alone or combined, in women with postmenopausal osteoporosis: the DATA study randomised trial. Lancet 382: 50-56. [ Ref ]