Journal Name: Journal of Biomedical Research and Reviews
Article Type: Review
Received date: 10 May, 2018
Accepted date: 22 May, 2018
Published date: 01 June, 2018
Citation: Van Dyke K, Castranova V (2018) Lung Diseases in Surface, Underground Coal Mining and Stone Workers: Role of Silica and Calcium Causative Agents in Inflammatory Reactions. J Biomed Res Rev Vol: 1, Issu: 2 (01-09).
Copyright: © 2018 Van Dyke K , et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Black lung disease or pneumoconiosis recently has dramatically increased in certain areas of Virginia, West Virginia and Kentucky where mineable coal seams are now relatively narrow in comparison to ten or more years ago. It has been previously established that the coal mine dust that miners breathe contains both coal and silica-based rock dust. The coal mine dust causing most of the increased toxicity to the lungs of these relatively younger miners has a higher concentration of silica dust demonstrated to be at least twenty-fold more toxic than coal dust to human lungs. The likely reason for the higher concentration of silica contaminating aforementioned coal mine dust is the use of new highly efficient mining machinery causing greater production of both coal and silica dust because there is less specificity in mining narrow coal seams. The coal companies use water sprays to prevent larger amounts of respirable dust and use a higher volume of fresh air for dilution but neither method effectively lowers the silica to coal dust ratio. It has been shown that freshly cut silica is more toxic than aged silica dust. The surface of silica of freshly fractured generates more free radicals than aged silica. However, either type of silica can create both acute and chronic inflammation that permanently injures the lung. When the silica enters deep in the lung, it is engulfed by phagocytic cells causing the complete spectrum of inflammation and lung injury and disease, if exposure is prolonged. Filtering masks can be effective but cause breathing difficulty. Methods have been developed to detoxify the silica particles, but they have not been used in mines. It is very difficult to treat silicosis, but Chinese physicians have developed an effective whole lung lavage system to remove silica from the lungs and have reported important improvement in lung function.
Keywords
Black lung disease, Silicosis, Lung damage, Acute and chronic inflammation, Cancer.
Abstract
Black lung disease or pneumoconiosis recently has dramatically increased in certain areas of Virginia, West Virginia and Kentucky where mineable coal seams are now relatively narrow in comparison to ten or more years ago. It has been previously established that the coal mine dust that miners breathe contains both coal and silica-based rock dust. The coal mine dust causing most of the increased toxicity to the lungs of these relatively younger miners has a higher concentration of silica dust demonstrated to be at least twenty-fold more toxic than coal dust to human lungs. The likely reason for the higher concentration of silica contaminating aforementioned coal mine dust is the use of new highly efficient mining machinery causing greater production of both coal and silica dust because there is less specificity in mining narrow coal seams. The coal companies use water sprays to prevent larger amounts of respirable dust and use a higher volume of fresh air for dilution but neither method effectively lowers the silica to coal dust ratio. It has been shown that freshly cut silica is more toxic than aged silica dust. The surface of silica of freshly fractured generates more free radicals than aged silica. However, either type of silica can create both acute and chronic inflammation that permanently injures the lung. When the silica enters deep in the lung, it is engulfed by phagocytic cells causing the complete spectrum of inflammation and lung injury and disease, if exposure is prolonged. Filtering masks can be effective but cause breathing difficulty. Methods have been developed to detoxify the silica particles, but they have not been used in mines. It is very difficult to treat silicosis, but Chinese physicians have developed an effective whole lung lavage system to remove silica from the lungs and have reported important improvement in lung function.
Keywords
Black lung disease, Silicosis, Lung damage, Acute and chronic inflammation, Cancer.
Introduction
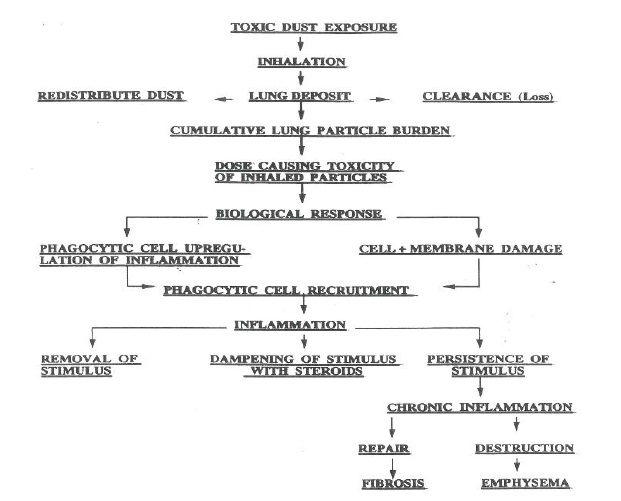
Miners breathing air from either surface or underground mines, over a series of years, can develop acute, chronic and massive lung inflammatory diseases where breathing becomes difficult [1,2]. The lung can develop silicosis, bronchitis, cancer and systemic autoimmune diseases like lupus and rheumatoid arthritis. Indeed, most of particleinduced lung damage originates from inhalation of respirable particles less than 10 microns in diameter. More recently nanoparticles are also thought to be responsible. The majority of this dust originates from coal itself which is generated in the process of mining it. However, often the mining equipment contacts and breaks rock which generates particles like sand, which is known as silica or chemically SiO2 (silicon dioxide). SiO2 is often found in nature as alpha quartz which is a crystalline structure with a central tetrahedron sharing all four of its corner oxygen atoms; the two face-center tetrahedra share two of their corner oxygen atoms; and the four edgecentered tetrahedra share just one of their oxygen atoms with other SiO4 tetrahedra. This leaves a net charge of 12 out of 24 total vertices for that portion of the seven SiO4 tetrahedra that are considered to be part of the unit cell for silica. It is well understood that particles of silica display negative charges which have a measureable zeta potential [3]. When miner’s inhale coal dust often with silica particles, it deposits along the respiratory tract. The body’s defense of particles, which deposit deep in the lung alveoli, are neutrophils and macrophage cells. Both cell types engulf foreign particles and carry them up the respiratory tract to the mucocillary escalator to be cleared. When the lung burden of either coal or silica dust is high, these phagocytic cells are activated/ damaged and release mediators and enzymes that can further damage the lung cells. These inflammatory mediators recruit more macrophages and other phagocytic cells into the alveolar spaces, and the process repeats many times until persistent/progressive inflammation and lung damage occurs, which triggers fibroblasts to produce fibrotic lesions. Initially the cells are activated to acute inflammation and after a series of weeks or months chronic inflammation occurs. Acute inflammation can be controlled with antiinflammatory steroids, but these drugs are ineffective in a chronic state.
Lung Disease Caused by Coal and Silica Dust
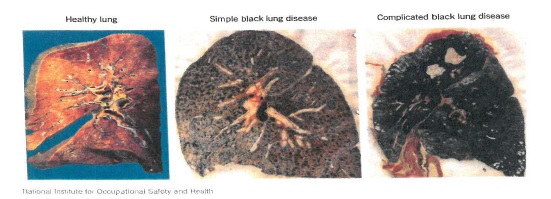
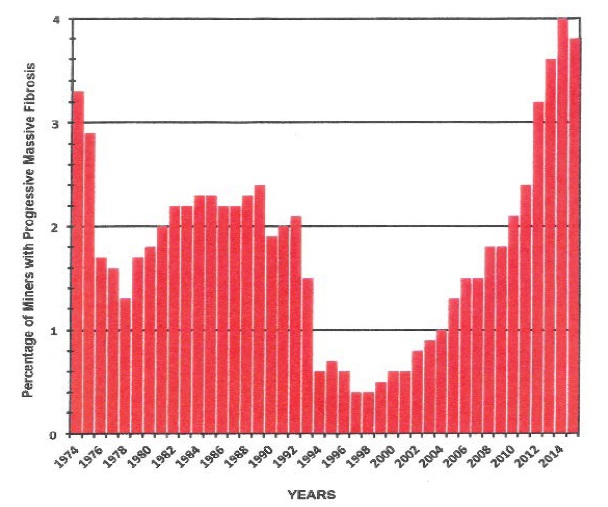
A major portion of lung damage in coal worker miners is coal workers’ pneumoconiosis, which is characterized by lesions called coal macules and coal nodules [3,4]. If miners are also exposed to crystalline silica, Silicosis can result [4,5]. Silicosis is characterized by fibrosis or scarring, which causes thickening of alveolar walls and a decrease in oxygen transport to pulmonary capillary blood. As silicosis progresses, silicotic nodules, i.e., spiral fibrotic lesions, become apparent [5] which occurs in the later stage chronic form of the disease. (Tables 1 and 2). In Figure 1 is demonstrated that the rate of progressive massive fibrosis decreased with the regulation of coal mine dust in the early 1970s to 2 mg/m2. However, an alarming rise in progressive massive fibrosis has been noted more recently (Figure 2). Underground mining and surface mining are very dangerous occupations in the United States and other countries as well [6]. In 2016, Blackley et al. [7] reported an outbreak of progressive massive fibrosis (PMF) in miners from Kentucky and Virginia. They identified that 416 of 11,200 miners have PMF which is 3.7% have this irreversible disease (Figures 3 and 4). PMF is a more quickly forming and very dangerous lung disease, in which massive fibrosis (scarring) of the lung occurs. This is the most severe form of black lung disease, which actually causes the volume of the lungs to shrink and causes damage to adjacent lung tissue making breathing difficult and decreasing gas exchange. Miners work long hours per day and many days per week. The recent trend is that this massive fibrosis can occur in as little as 5 years of mining underground. This massive fibrotic disease occurs to a greater extent in certain mines in Virginia, West Virginia and Kentucky but can also occur in surface mines. Why do these hot spots of PMF occur? Werntz and Allen [8] have proposed that multiple factors occur in coal mines in this region. For example, many old mines are cutting seams of coal that are ‘low coal”, which means the coal seams narrow to 32-36 inches. When the new continuous mining (tall machines) cut the coal from these seams–they remove 12- 16 inches of sandstone adjacent to the coal seam. This silica dust from sandstone mixes with the coal dust generated by this process. Mining machines equipped with water sprays do decrease airborne dust levels. However, cutting extensive amounts of sandstone produces substantial amounts of respirable silica dust, and it is often difficult to control silica dust within the limits of governmental standards, since newer coal mining machines cut through coal or rock more quickly than older ones and thus more toxic dust is generated per time.
Figure 1: Healthy Dried Lung, Simple Black Lung, Complicated Black Lung.
Figure 2: Percentage of miners with progressive massive fibrosis from 1974-2016.
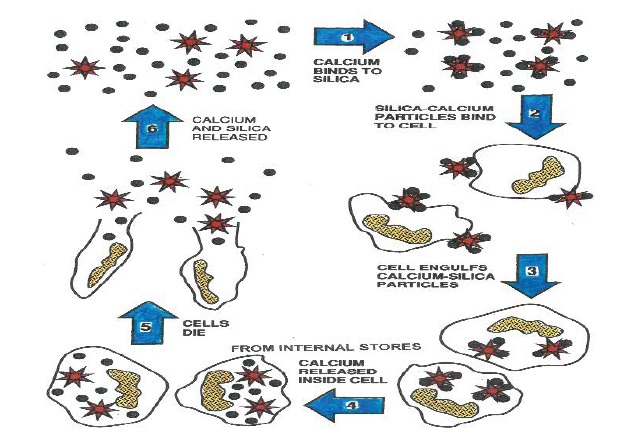
Figure 3: Theoretical cyclic diagram of the interaction of calcium, silica (quartz)and engulfment by phagocytic cells and release of calcium from various stores and the death of the cells.
Table 1: Respirable crystalline silica- (Quartz).
| Factor | Effect |
|---|---|
| Exposure | Silica is more toxic than coal (exposure limited to 1/20th that of coal in 1969 Act) |
| Age | Freshly fractured silica is more toxic than aged silica |
| Particle size | Smaller particles are more toxic |
| Consequences of overexposure | Silicosis Airways diseases Pulmonary TB Chronic renal disease Lung Cancer |
Table 2: Silicosis-chronic, accelerated, acute times of development.
| Silicosis | ||
|---|---|---|
| Chronic | Accelerated | Acute |
| Occurs after 10 or more years of exposure | Develops in 5 to 10 years | Develops in less than 5 years |
| Swelling in lungs | Symptoms occur faster than in chronic silicosis | Lungs become inflamed and fill with fluid |
| Troubled breathing similar to COPD | Severe shortness of breath and low blood oxygen | |
It is now suggested that rapid onset and progression of lung disease in coal miners from this region is due to inhalation of higher concentrations of silica dust [9]. The main method used to prevent lung diseases caused by coal mine dust is to limit the airborne level of dust inhaled by the worker. The federal regulated limit for coal mine dust has recently been lowered from 2.0 milligrams per cubic meter of air down to 1.5 milligrams per cubic meter of air by the Mine Safety and Health Administration (MSHA). This minor change in particles is 25% less than before but if the ratio of silica particles to coal particles is higher in certain minesthe silica exposure could actually be higher than previously regulated. It is clear that the amount of inhaled silica needs to be reduced.
Can We Decrease the Amount of Toxic Dust by Breathing Less Silica or Decreasing the Toxicity of Silica Inhaled?
Certainly, a simple answer is to use fiber masks which fit over the nose and mouth snugly to the face which are manufactured by several companies and can decrease the concentration of inhaled small particles by 95% or more. Furthermore, these masks could be charged positively so they more efficiently capture negatively charged silica. When a masks clogs with dust, it can be replaced with a similar mask that adheres to the face. However, most miners consider the masks uncomfortable and generally they are not used on a routine basis.
There are positive air pressure filtering respirator helmets which attach to the head and are powered by external battery worn on the belt. A fan attached to the head unit draws in air from the mine and filters it to remove particles and then the filtered air is blown into a clear screen that partially covers the face from which the wearer breathes. This clear mask bends around the face- with the filtered air descending from the top of the unit with the filter on top. The apparatus looks something like a welder’s helmet but can be made light weight. The main advantage is that breathing is not impaired, and the moving clean air also cools the face. This would make wearing this personal protective device more comfortable. Masks of this type are used by surgeons. The disadvantage is that these positive air filtering masks are much more expensive.
Use of Chemical Coatings which would Bind Specifically to the Surface of Silica and Possibly of other Toxic Silicates which Help Subvert their Toxicity
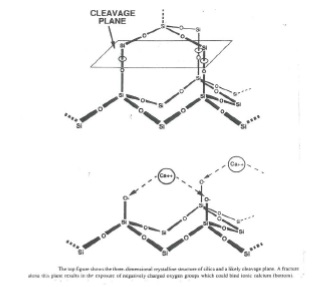
Silica particles which have been freshly cut from alpha quartz or sandstone produce free radicals or substances with unpaired electrons on their surface [10]. The demonstration of siloxyl radicals in the cleavage plane is shown in Figure 5. If freshly cut or ground silica particles are placed in a scintillation vial and counter which measures blue light, a considerable amount of counts per minute can be observed [11] and a variety of animal studies following pulmonary exposure of rats to freshly fractured versus aged silica particles clearly demonstrate that fresh silica is more toxic than similar sized aged particles [12,13]. Figures 4 and 5 explain the diagrammatic sequence of dust exposure and consequences and cyclic nature of silica activated chronic acute and chronic inflammation.
Figure 4: Diagram representing toxic dust exposure causing toxicity of inhaled particles and the biological response causing cellular damage and upregulation leading to acute and chronic inflammation and consequences.
Figure 5: Three-dimensional representation of silica molecule and cleavage with binding of calcium.
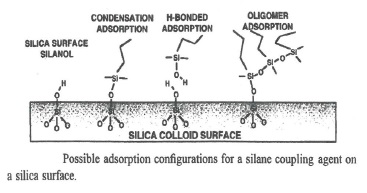
It is well known that researchers studying platelets in glass vessels have found that these platelets stick to the glass surface which activates the platelet to clot. In order to prevent this occurrence, it was found if the glass was precoated with the liquid tetramethysilane (TMS) or (Prosil 28), the platelets would not stick to the glass surface because the chemistry of silica or glass has a chemically coated surface. Since silica is a form of glass, it would follow that if you coated silica particles with TMS, they might prove to be less toxic. This reaction requires heat to be effective. During drilling or cutting of coal- adjacent silica or quartz deposits are also cut. The aerosolized coal and silica dust becomes warm because the drilling or cutting process generates friction and therefore heat. Often when continuous mining equipment generates dust from both minerals, the dust is wetted with water sprays which would also be warmed by the drill friction. If the TMS could be added to the water, it could coat the silica. Once the silica surface was covered with TMS and chemically bonded to the silica Fig 6, our laboratory has shown that the toxicity of silica is greatly reduced via coating with Prosil 28, an organosilane [14].
In addition, both newer water and organic soluble silanes are being currently produced which effectively coat the surface of silica particles. In a recent article in Annals of Work Exposure and Health 2017 [15], Christina Ziemann et al. used a similar concept as the work above [14] but with two different organosilanes-Dynasylan-or PTMO and Dynasylan SIVO 160 to coat silica particles as a covalent coating for ceramics production. This organosilane coating of silica and silicates could make ceramics production safer without loss of product quality. Coating effectiveness was measured in artificial alveolar and lysosomal fluids-then analyzed and found to be stable for at least one week. These particles were analyzed in vitro with industrially relevant quartz Q1 used as the respiratory silica model and quartz DQ12 as a positive control. They used primary rat alveolar macrophages as their cellular model-with exposure of 75 microgram/cc with a 4-hour incubation at 37C ± aluminum lactate to verify quartz-related effects. Toxicity assays were measured using macrophage lactate dehydrogenase (LDH) release and DNA strand break induction using alkaline Comet assay as biological toxicity endpoints. The results of their study indicated that Dynasylan SIVO 160 (0.2% w/w of quartz), which is highly compatible with water and most reactive with silica chemistry was most effective in inhibiting the toxicity of biologically active quartz (silica) species without interfering with the technical process quality of ceramic products. Their organosilane coating of silica was effective in both in vitro and in vivo studies. These authors concluded that covalent organosilane coatings of quartz (silica) might represent a promising strategy to increase worker safety in a traditional ceramics industry and we suggest possibly in other industries, where silica aerosilization occurs. But we do not know the toxicity of the organosilane coating of silica in man.
Toxicity Studies of Silica in Lungs of both Animals and One Human-Exposed to Silica
In a series of experiments from our lab, rats were placed under anesthesia and their lungs were exposed by intratracheal instillation to silica suspended in saline. After 24 hours exposure to silica, the contents of the lungs were washed out and their cellular content was measured [16]. In addition, nitric oxide associated luminol dependent luminescence activation was assessed as a measure of oxidative stress of the lung [17]. There was an amazing 10-fold increase in oxidative stress via this peroxynitrite luminescence after only 24 hours post silica treatment. This group of silica- treated cells was compared to cells from animals without silica as controls. When acute inflammation occurs in the lungs, the peroxynitrite luminescence is stimulated quickly and is most stimulated compared to control cells.
This luminol- dependent blue light emanates from peroxynitrite which is produced from nitric oxide (N=O)) via the induction of the macrophage enzyme called nitric oxide synthase 2 (inducible NOS2) as demonstrated by Blackford et al. [17] and in addition superoxide reacts with an equivalent amount of nitric oxide radicals producing peroxynitrite which can react with carbon dioxide producing peroxynitrite carbonate. This is a major oxidizer and nitrator of phenolic substances and sulfhydryl groups causing R—SH→RSNO to occur. Once peroxynitrite is formed it most likely reacts with CO2 forming a carbonate which is the likely chemical which causes oxidation and stimulates nitration which is capable of producing major damage to DNA, RNA, protein and lipids [18]. The increase in peroxynitrite or its carbonate derivative occurs within a few hours of the placement of silica into the lungs, and this is a surprising and highly toxic reaction. If this reaction is investigated with macrophages from naïve rats and then exposed in vitro to silica in presence of luminol, very little luminescence over background is noticed. This indicates that exposure of silica inside the lungs of animals or humans is actually required to activate an nitric oxide synthase 2 to produce sufficient nitric oxide via an in vivo induction process, which can be mimicked either via instillation or inhalation of silica [19].
In order to understand this observation, once silica is placed inside the animal’s lungs via inhalation or instillation, the in vivo induction of nitric oxide synthase 2 occurs rather quickly. If dexamethasone is injected into animals right after the silica is instilled, the ten- fold increase in peroxynitrite luminescence (as observed with silica alone with luminol)- does not occur [20]. Dexamethasone inhibits the nuclear factor kappa b transcription factor [21], which stimulates the deacetylation of histone proteins via histone deacetylase 2. This causes the histone proteins to become positively charged and binds to DNA which stops transcription of inflammatory proteins ending acute inflammation. This observation was made originally by Professor Peter Barnes [22]. There was a clinically important case reported in which a rock driller at a surface coal mine was exposed to a very high dose of silica dust. He was treated with an anti-inflammatory steroid and this was found to be effective by allowing him to breathe fairly normally. However, the physicians in charge were worried about the effects of continuous large doses of these steroids, so he was eventually withdrawn from these drugs. The progression of disease resumed, and he soon had severe difficulty breathing again. He passed away a short time thereafter [23]. The likely basis of this clinical observation is that initially he was suffering from acute inflammation from silica inhalation. Once steroids were administered, the acute inflammation in the lungs was inhibited. However, since the silica was not removed, and steroid treatment was ended the disease state went into a chronic form. Chronic inflammatory diseases generally do not respond to steroids because the excessive peroxynitrite which is continuously formed damages the histone deactylase 2 enzyme via nitration. Clinically anti-inflammatory steroids are not recognized for long standing cases of black lung or silicosis because they are not effective. The treatment with steroids must be rendered in the acute rather than the chronic inflammatory state. However, if silica were removed from the lung via whole lung lavage as conducted by the Chinese physician’s, it seems likely steroids would be more effective (see discussion).
Why does Inhaled Silica Cause such Extensive Inflammatory Lung Damage after a Period of Time? Is Intracellular Calcium Linked to Inflammatory Cell Damage Caused by Silica?
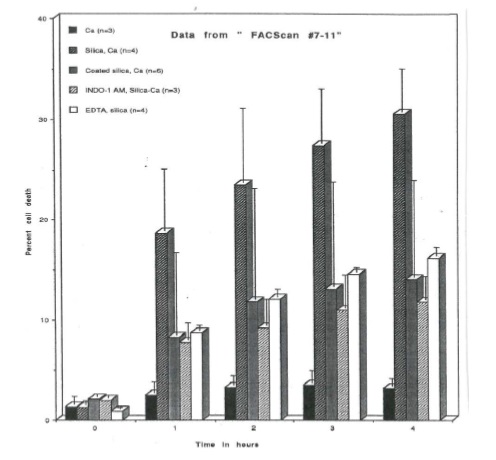
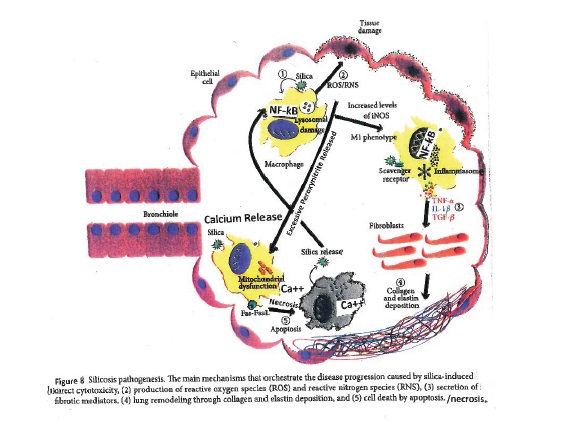
Exposure of the lung to silica induces production of reactive oxygen and nitrogen species [17, 24] as well as production of inflammatory and fibrotic mediators [5]. This activation of alveolar macrophages and lung epithelial cells apparently depends on silica-induced release of calcium from intracellular and possibly other stores as shown in figure 5 and 6. This calcium mobilization was demonstrated in flow cytometry studies using isolated human neutrophils pretreated with a calcium indicator, indo-1-am. Indo-1- am is an uncharged esterified molecule which, when deesterified once inside the cell can bind calcium mobilized from internal stores or even other stores and becoming fluorescent. Indeed, activation of phagocytic cells by silica has been shown to mobilize calcium [25]. Of interest, indo- 1 acts as a chelator of internal calcium and can be used to block silica-induced oxidant release, demonstrating the role of elevated internal calcium in stimulus-secretion coupling [26]. Pretreatment with indo-1-am actually prevents death from silica because the calcium chelator Indo-1 prevents the action of released calcium from causing death of phagocytic cells as shown in figures 7 and 8.
Figure 6: Reaction of silica surface chemistry with absorption and bonding to organosilane molecules which covers the surface of the silica which inhibits toxicity to phagocytic lung cells. Further work with siliconized silica particles indicates that its molecular coating markedly inhibits silica’s toxicity and the killing of phagocytic lung cells.
Figure 7: Flow cytometry studies with human neutrophils incubated for various times (hours) with particles of silica, coated silica , and indo-1 AM treated cells with silica and EDTA-silica treated cells. This graph indicates the great killing of the cells by silica, and protection via tetramethyl silane coated silica or by INDO-1AM which is an esterified uncharged calcium chelator that once it goes inside the cell and becomes de-esterified binds the toxic calcium excess. This protects the cell from excessive calcium released inside the cell, once the silica has been engulfed.
Figure 8: Pathogenesis diagram of silicosis inside bronchiole depicting oxidative/nitrosative stress inside the macrophage with the induction of nitric oxide synthase 2. Then the scavenger receptor is activated and the inflammasome generates cytokines and chemokines and excessive peroxynitrite. This activates the fibroblasts to increase collagen and elastin deposition causing fibrogenesis and scarring. The macrophages die via apoptosis and necrosis and silica is again released to re-stimulate the chronic inflammatory cycle.
Low Dose Gamma Radiation Damage can be Inhibited by Indo-1-Am and Presents a Similar Biochemical Toxicity Picture as Silica
An article was written by Leach et al. [27] who demonstrated that low dose gamma radiation generates peroxynitrite in cells- which can be blocked by using INDO- 1-AM. These scientists went further and found that the radiation produced peroxynitrite caused membrane damage, calcium influx, and a rise in internal calcium, which affected a mitochondrial permeability transition pore mechanism which usually controls mitochondrial calcium concentration, so calcium does not become toxic to many mitochondria. When excessive internal calcium ions exist via toxic reactions, the transition pore likely becomes overloaded and the mitochondria die. This causes the cell to die since the cell depends upon the mitochondria to provide energy. It seems quite likely that excessive free internal calcium is toxic in both chronic inflammatory cases, i.e., silica/ macrophages and radiation exposed human cells. When macrophages die, and silica cannot be cleared from the lung by alveolar macrophages, silica persists, and a continuous cycle of oxidant stress, mediator release, and lung injury occurs as new phagocytic cells are recruited to the airspaces. This chronic death and inflammation eventually causes the inflammatory system to go from acute to chronic conditions where massive amounts of oxidant species are released and massive pathological damage to lung epithelial cells results in scarring, i.e., fibrosis. In the early stages of acute inflammation caused by silica- anti-inflammatory steroids are effective in controlling the acute inflammation from silica. However, when the disease goes into a chronic stage, steroids are not effective- because the excessive peroxynitrite generated in chronic diseases destroys the mechanism by which steroids act, ie., deacetylation of histones. Unfortunately, there are few alternative treatments and miners with excessive silica lung burdens develop chronic and progressive fibrosis. In severe cases, lung transplantation may be necessary to continue life. This is because silica and coal dust cause scarring of the lung and the lung eventually cannot exchange oxygen from the air sufficiently to maintain life. Miners can receive transplanted lungs, which can be helpful, but they generally must take anti-rejection drugs for the rest of their life. This creates a weakened immune system with a higher risk of problems with various infectious diseases.
In China, physicians have developed a whole lung lavage procedure for patients with chronic lung disease due to silica or other particles [28]. In this procedure, one half of the lung is washed by intratracheal instillation withdraw of physiological fluid. After a day of recovery, the other half of the lung is washed. Using this whole lung lavage, large amounts of particulates can be washed out of the lung. Therefore, this whole lung lavage is effective in dramatically reducing the lung burden of particles. Once the patient had adequately recovered, treatment with steroids may be effective.
Other Possible Procedures Which Could be Tried
If the mining procedure was more selectively directed to mining coal and not the combination of coal and rock, the recent rise in PMF may be stopped. This might be accomplished by deep x ray of the area, which would be drilled or cut- and the band of coal could be selected more precisely using more specific cutting devices set to drill coal only, once the seam was clearly delineated.
Since it is known that continuous exposure to silica can generate continuous and copious amounts of peroxynitrite in the human body, which is associated with the transition from acute to chronic inflammation, an effective strategy could be to develop a continuous method to decrease the amount of peroxynitrite. Steroids can be effective if used early in the exposure sequence, but there are likely much better peroxynitrite antagonists, which would not have so many side effects. By using luminescence screening methods [29,30-32] which detect peroxynitrite in the presence of a luminol derivative (L-012), we screened a variety of substances that are mono, di, and polyphenolic substances which were effective in destroying excessive peroxynitrite and inhibiting luminescence. In addition, we found that some unsaturated lipid molecules can be readily nitrated like tocotrienols (vitamins E form) and antioxidants like vitamin C can destroy peroxynitrite. It is likely that many substances that are antioxidants or that are targets of nitration, but which demonstrate little toxicity to the human body would be good candidates to control excessive peroxynitrite or its carbonated derivative.
Results and Conclusion
Since this is a mini-review, this is a compilation of the work of ourselves and many other scientists and the results indicate that coal mining involving respirable silica is a major factor causing acute, and chronic inflammation leading to massive fibrosis of the lung. Freshly broken silica is more toxic than aged silica likely because of extensive free radical generation. It is the surface of the silica particle that initially creates the toxicity, because when it is coated with tetramethyl- silane (Prosil 28), much of the toxicity to the lungs of animals is abrogated. Why would such a seemingly inert substance like SiO2 (sand) cause such toxicity? It is likely due to the fact that once these small silica particles- (microns in diameter) enter the deep spaces of the lung (alveoli), these particles are engulfed by cells like neutrophils and macrophages. This released stored calcium in different areas of these cells, which activates the transcription factor NF kappa b and acetylation of histone proteins that are arranged as a spool-like structure on which is wound DNA. Histone acetyl transferase (HAT) increases the acetylation of the epsilon amino groups of lysines on the histones. This changes the positive charges of the histones, which are bound to the negative phosphates on the DNA helix and opens inflammatory genes to produce a variety of proteins and inflammatory gene products. This acute inflammation, if caught early enough using anti-inflammatory steroids, can be stopped, decreasing much of the damage to respiration. However, if it is not treated at an early stage, chronic inflammation results which is not treatable with steroids because a continuous production of a peroxide (peroxynitrite carbonate) damages the steroid mechanism.
Much of this damage to the lungs is preventable by using water sprays and proper ventilation of the air or the use of respirators or even fibrous masks which can exclude 95% of the dusts. The workers find the masks produce great difficulty in breathing. However, the danger of life-long damage to respiration should produce a proper decision. In most difficult silicosis cases, Chinese physicians have developed a whole lung lavage (wash-out procedure) which is effective in removing large quantities of silica from the lung. The conclusion is that proper procedures have been outlined in NIOSH publications. Workers whose workplace produces respirable silica dust particles should be instructed by employers to follow these governmental procedures to produce a safe workplace environment.
Castranova V, Ducatman B (1997) Toxicology of the Respiratory System. Coal Dust. Elsevier Science Inc., New York, pp 361-372. [ Ref ]
Goodman GB, Kaplan PD, Stachura I, Castranova V, Pailes WH, et al. (1992) Acute silicosis responding to corticosteroid therapy. Chest 101: 366-370. [ Ref ]
Ho RF, Baird T, Hammaerschlag G, Hart D, Johnson AR, et al. (2017) Artificial stone-based silicosis: a rapidly emerging occupational lung disease. Occupational Environmental Medicine 75: 3-5. [ Ref ]
Mandel G, Mandel N (1995) Silica & Silica-Induced Lung Diseases: Current Concepts. The structure of crystalline SiO2. CRC Press, Florida, pp 63-78. [ Ref ]
Castranova V, Vallyathan V (2000) Silicosis and coal workers’ pneumoconiosis. Environ Health Perspect 108: 675-684. [ Ref ]
Castranova V (2000) From coal mine dust to quartz: mechanisms of pulmonary pathogenicity. Inhal Tox 12: 7-14. [ Ref ]
Haldin CN, Reed WR, Colinet MS, Rider JP, Petsonk EL, et al. (2015) Debilitating Lung Disease Among Coal Miners’s With no Underground Mining Tenure. J Occup Environ Med 57: 62-67. [ Ref ]
Blackle DJ, Crum JB, Halldin CN, Storey E, Laney AS (2016) Resurgence of Progressive Massive Fibrosis in Coal Miners-Eastern Kentucky,2016. Centers for Dseae Control and prevention 65: 1385-1389. [ Ref ]
Allen A, Werntz C (2018) Black Lung Disease on the rise :5 questions answered. J Am Med Assoc. [ Ref ]
Collinet J (2014) Health Consequences of Overexposure to Respirable Coal and Silica Dust-Office of Mine Safety and Health Research-OMSHRPresentation by Jay Collinet –Senior Scientist CDC NIOSH Oct 28, 2014 Beckley WV. [ Ref ]
Vallyathan V, Shi X, Dalal NS, Irr W, Castranova V (1988) Potential role of reactive silicon‑oxygen radicals in acute silica‑induced lung injury. Am Rev Resp Dis 138: 1213‑1219. [ Ref ]
Castranova V, Vallyathan V, Van Dyke K, Dalal NS (1989) Use of chemiluminescence assays to monitor the surface characteristics and biological reactivity of freshly fractured vs aged silica. Effects of Mineral Dusts on Cells. New York. [ Ref ]
Vallyathan V, Castranova V, Pack D, Leonard S, Shumaker J, et al. (1995) Freshly fractured quartz inhalation leads to enhanced lung injury and inflammation: potential role of free radicals. Am Review Respir and Critical Care Med 152: 1003-1009. [ Ref ]
Castranova V, Pailes WH, Dalal NS (1996) Enhanced pulmonary response to the inhalation of freshly fractured silica as compared to aged dust exposure. Appl Occup & Environ Hygiene 11: 937-941. [ Ref ]
Castranova V, Van Dyke K, Wu L, Dalal NS, Vallaythan V (1995) Silica & Silica-Induced Lung Diseases: Current Concepts. Suppression of silicainduced toxicity with organosilane surface coating. CRC Press, Florida, pp 283-292. [ Ref ]
Van Dyke K, Guiterrez J, Van Dyke C, And Wu L (1995) Silica and Silica- Induced Diseases. Early Role of Lipid Mediators in Silica Toxicity: Possible methods to Detoxify Silica. CRC Press, Florida, pp 209-228. [ Ref ]
Ziemann C, Escrig A, Bonvicini G, Ibanez MJ, Monfort E, (2017) Organosilane-Based coating of Quartz Species from the Traditional Ceramics Industry:Evidence of hazard Reduction Using In Vitro and in Vivo Tests. Annls of Work Exposure s and Health 61: 468-480. [ Ref ]
Castranova V, Pailes WH, Li C (1990) Effects of silica exposure on alveolar macrophages: action of tetrandrine. Proc of the International Symposium on Pneumoconioses, China. [ Ref ]
Blackford JA, Antonini JM, Castranova V, Dey RD (1994) Induction of nitric oxide synthase gene expression and nitric oxide production in alveolar macrophages following intratracheal instillation of silica. Am J Resp Cell Mol Biol 11:426-431. [ Ref ]
Meli R, Nauser T, Latal P, anf Koppenol H (2002) Reaction of peroxynitrite with carbon dioxide: intermediates and determination of the yield of CO-3 radical and NO2- radical. Journal of Biological Inorganic Chemistry 7: 31-36. [ Ref ]
Antonini JM, Van Dyke K, Ye Z, DiMatteo M, Reasor M (1993) Introduction of Luminol-dependent Chemiluminescence as a method to study silica inflammation in the tissue and phagocytic cells of rat lung. Environmental health Perspectives 10: 37-42. [ Ref ]
Van Dyke K, Antonini J, Wu L, Ye Z, And R, et al. (1994) The inhibition of silica-induced lung inflammation by dexamethasone as measured by broncoalveolar lavage parameters and peroxynitrite dependent chemiluminescence. Agents and Action 41: 44-49. [ Ref ]
Sacks M, Gordon J, Bylander J, Porter D, Shi X, et al. (1998) Silica-induced pulmonary inflammation in rats: activation of NFkβ and its suppression by dexamethesone. Biochem Biophys Res Commun 253: 181-184. [ Ref ]
Barnes PJ (2011) Glucocorticoids current and future direction. British Journal of respiratory Pharmacology 163: 29-43. [ Ref ]
Goodman GB, Kaplan PD, Stachura I, Castranova V, Pailes WH, et al. (1992) Acute silicosis responding to corticosteroid therapy. Chest 101: 366-370. [ Ref ]
Castranova V, Antonini JM, Reasor MJ, Wu L, Van Dyke K (1995) Silica & Silica-Induced Lung Diseases: Current Concepts. Oxidant release from pulmonary phagocytes. CRC Press, Florida, pp 185-196. [ Ref ]
Castranova V, Van Scott MR, Van Dyke K (1987) Cellular Chemiluminescence. Stimulus secretion coupling in phagocytes. CRC Press, Florida. [ Ref ]
Van Dyke K, Guitterez J, Van Dyke C, Nowack C (1993) Piggy Back Mechanism with calcium may Explain How Silica Exerts its Toxicity to Phagocytic Cells. Microchemical Journal 48: 34-41. [ Ref ]
Leach JK, Van Tuyle G, Lin PS, Schmidt-Ulrich R, Mikkelsen RB (2001) Ionizing Radiation-induced Mitochondria-dependent Generaation of Reactive Oxygen/Nitrogen. Cancer Research 61: 3894-3901. [ Ref ]
Zhang YM, Zhang HT, Wang CY, Wu J, Wang C (2012) Long Term therapeutic Effects of whole lung lavage in the management of silicosis. [ Ref ]
Van Dyke Knox, McConnell P, Marquardt L (2000) Green tea extract and its polyphenols markedly inhibit luminol-dependent chemiluminescence activated by peroxynitrite or SIN-1. Luminescence 15: 37-43. [ Ref ]
Van Dyke K, Sacks M, Qazi N (1998) A new screening method to detect water-soluble antioxidants: acetaminophen (Tylenol) and other phenols react as antioxidants and destroy peroxynitrite-dependent cemilumiluminescence. J Biolum and Chemilum13: 339-348. [ Ref ]