Journal Name: Journal of Biomedical Research and Reviews
Article Type: Research
Received date: 08-November-2021
Accepted date: 21-December-2021
Published date: 28 December-2021
Citation: Yu T, Hua Y, Cen X, Niu S (2021) The Impact of Fidelity-Based Simulated Medical Undergraduate Education: A Systematic Review and Meta-Analysis of Randomised Controlled Trials. J Biomed Res Rev Vol: 4, Issu: 2. (09-15).
Copyright: © 2021 Yu T et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
This study aims to compare the effectiveness of the fidelity level of the simulation on undergraduate medical education through meta-analysis. 15 studies met the inclusion criteria. Six studies evaluated students’ theoretical knowledge between high-fidelity and low-fidelity simulators, five of these studies reported no significant difference between lowfidelity simulation and high-fidelity simulation groups, and one of these studies reported that high-fidelity simulators are more effective than lowfidelity simulators. Twelve studies evaluated students’ skill performance between high-fidelity and low-fidelity simulators, seven of these studies reported no significant difference between low-fidelity simulation and high-fidelity simulation groups, four of these studies reported that highfidelity simulators are more effective than low-fidelity simulators, and one of these studies reported that low-fidelity simulation performs better than high-fidelity simulation in several sub items. Seven studies evaluated students’ confidence between high-fidelity and low-fidelity simulators, three of these studies reported no significant difference between low-fidelity simulation and high-fidelity simulation groups, and one of these studies reported that students in the high-fidelity manikin simulator group recorded higher scores than students in the low-fidelity manikin simulator group. Due to the different interventions used in each study and the different evaluation methods used for outcome indicators, it is difficult to determine which intervention is more effective through meta-analysis. Although some results are positive, it seems that there was no significant difference between high-fidelity simulation and lowfidelity simulation in terms of students’ theoretical knowledge, clinical skills or improved confidence. With the wide application of simulation in medical education, further research should focus on the influence of simulation level on continuing medical education.
Keywords
Simulator, Medical student, Education, Meta-analysis.
Abstract
This study aims to compare the effectiveness of the fidelity level of the simulation on undergraduate medical education through meta-analysis. 15 studies met the inclusion criteria. Six studies evaluated students’ theoretical knowledge between high-fidelity and low-fidelity simulators, five of these studies reported no significant difference between lowfidelity simulation and high-fidelity simulation groups, and one of these studies reported that high-fidelity simulators are more effective than lowfidelity simulators. Twelve studies evaluated students’ skill performance between high-fidelity and low-fidelity simulators, seven of these studies reported no significant difference between low-fidelity simulation and high-fidelity simulation groups, four of these studies reported that highfidelity simulators are more effective than low-fidelity simulators, and one of these studies reported that low-fidelity simulation performs better than high-fidelity simulation in several sub items. Seven studies evaluated students’ confidence between high-fidelity and low-fidelity simulators, three of these studies reported no significant difference between low-fidelity simulation and high-fidelity simulation groups, and one of these studies reported that students in the high-fidelity manikin simulator group recorded higher scores than students in the low-fidelity manikin simulator group. Due to the different interventions used in each study and the different evaluation methods used for outcome indicators, it is difficult to determine which intervention is more effective through meta-analysis. Although some results are positive, it seems that there was no significant difference between high-fidelity simulation and lowfidelity simulation in terms of students’ theoretical knowledge, clinical skills or improved confidence. With the wide application of simulation in medical education, further research should focus on the influence of simulation level on continuing medical education.
Keywords
Simulator, Medical student, Education, Meta-analysis.
Introduction
Since its birth in the 1960s and with the rapid development of human model simulators, simulation-based teaching has been integrated into most clinical courses [1]. Moreover, many experiments have fully demonstrated the positive effects of simulation-based theoretical knowledge and clinical skills [2,3]. Lack of clinical practice is a common problem in undergraduate medical education. Training and teaching based on simulation can provide medical students with practical application experience. Training and teaching based on simulation is an ideal teaching mode to provide medical students with theoretical knowledge and hands-on practice by constructing simulation environments instead of real scenes; this approach is considered to have great development potential. With the development of modern technology and advances in synthetic materials technology, current simulators are able to provide a very realistic environment, reproducing realistic changes and providing feedback. High-fidelity simulation (HFS) can be used for training and to immerse users in complex and realistic scenarios by providing realistic feedback. However, some simulators with limited functions can only provide a specific simulation environment and cannot provide all realistic feedback; this is called low-fidelity simulation (LFS). Studies have found that compared with LFS, HFS can not only fail to improve students’ abilities in terms of knowledge and skills but can also cause them to have blind confidence and seriously overestimate their abilities. This is an undesirable outcome because one of the most common cognitive biases that leads to clinical diagnosis errors is overconfidence [4]. The impact of fidelity based on simulated theoretical knowledge, skill performance, or confidence is unlcear. Therefore, to explore the effect of simulator fidelity on undergraduate medical education, a meta-analysis based on existing studies is necessary. This study aims to compare the theoretical knowledge, skill performance and confidence of undergraduate medical students between LFS and HFS through meta-analysis according to the fidelity level of the simulator.
Materials and Methods
Search strategy
Literature retrieval: Two researchers (Y.H. and XY. C) independently searched PubMed, the Cochrane Library, and Embase online and collected randomised controlled studies on HFS and LFS in medical undergraduate education; the date range was January 1, 1995, to October 20, 2020. The online search was supplemented by a manual search and followup search, and the authors were asked for the full text and original data. Search keywords: (“high patient simulators” or “high fidelity simulation”) and (“low fidelity simulation” or “static” or “low patient simulators) and (“medical education” or “undergraduate education”).
Data screening and extraction
Inclusion criteria: 1. Type of study: randomised controlled study on the differences in theoretical knowledge, skill performance and confidence between LFS and HFS; 2. Research objects: Students receiving undergraduate medical education; 3. Intervention measures: A high-fidelity simulator was used in the experimental group, and a lowfidelity simulator was used in the control group. Specific information on the simulator was mentioned in the paper, and the sizes of the experimental group and control group were clear. 4. Outcome indicators: theoretical knowledge, skill performance and confidence.
Exclusion criteria: 1. Data repeat; 2. The ending is not related; 3. The result is incomplete; 4. Result cannot be obtained or extracted
Study selection: All possible eligible study titles were screened by two independent reviewers (Y.H. and XY. C), not excluding abstracts and full text. After filtering based on the titles of the articles, both reviewers reviewed the remaining papers and identified articles that met the inclusion criteria. Differences between the two reviewers were resolved by discussion or by arbitration by the third investigator. We define the fidelity of the simulator as the physical properties of the simulator. High-fidelity simulators are “those that provide physical examination, display vital signs, physiological responses, intervention (through a computer interface) and allow certain operations to be performed on them (endotracheal intubation, intravenous intubation, face mask, etc.).” Low-fidelity simulators, on the other hand, are “static models that are otherwise limited by these capabilities” [5].
Grading the evidence
Data collection: Two independent reviewers (Y.H. and XY. C) used spreadsheet data extraction to extract the results of the randomised controlled trials. To evaluate the quality of the included studies reporting and randomisation, degree of blinding and concealed allocation, we applied the Cochrane bias risk tool, and discussion or arbitration by a third researcher was used to settle differences in the evaluation [6]. If the articles reported uncertain data or had missing data, the author was contacted to obtain the missing details so that enough original data could be obtained for the meta-analysis.
Endpoints
The main end point is to compare low-fidelity simulators and high-fidelity simulators in terms of the theoretical knowledge and skill performance of medical undergraduate students. The secondary endpoint is a comparison of the confidence of participants between those taught with lowfidelity simulators and those taught with high-fidelity simulators. Theoretical knowledge is defined as the degree of mastery of the clinical knowledge system. Skill performance is defined as the performance of clinical skills and thinking ability. Confidence is defined as the level of self-satisfaction and self-efficacy.
Results
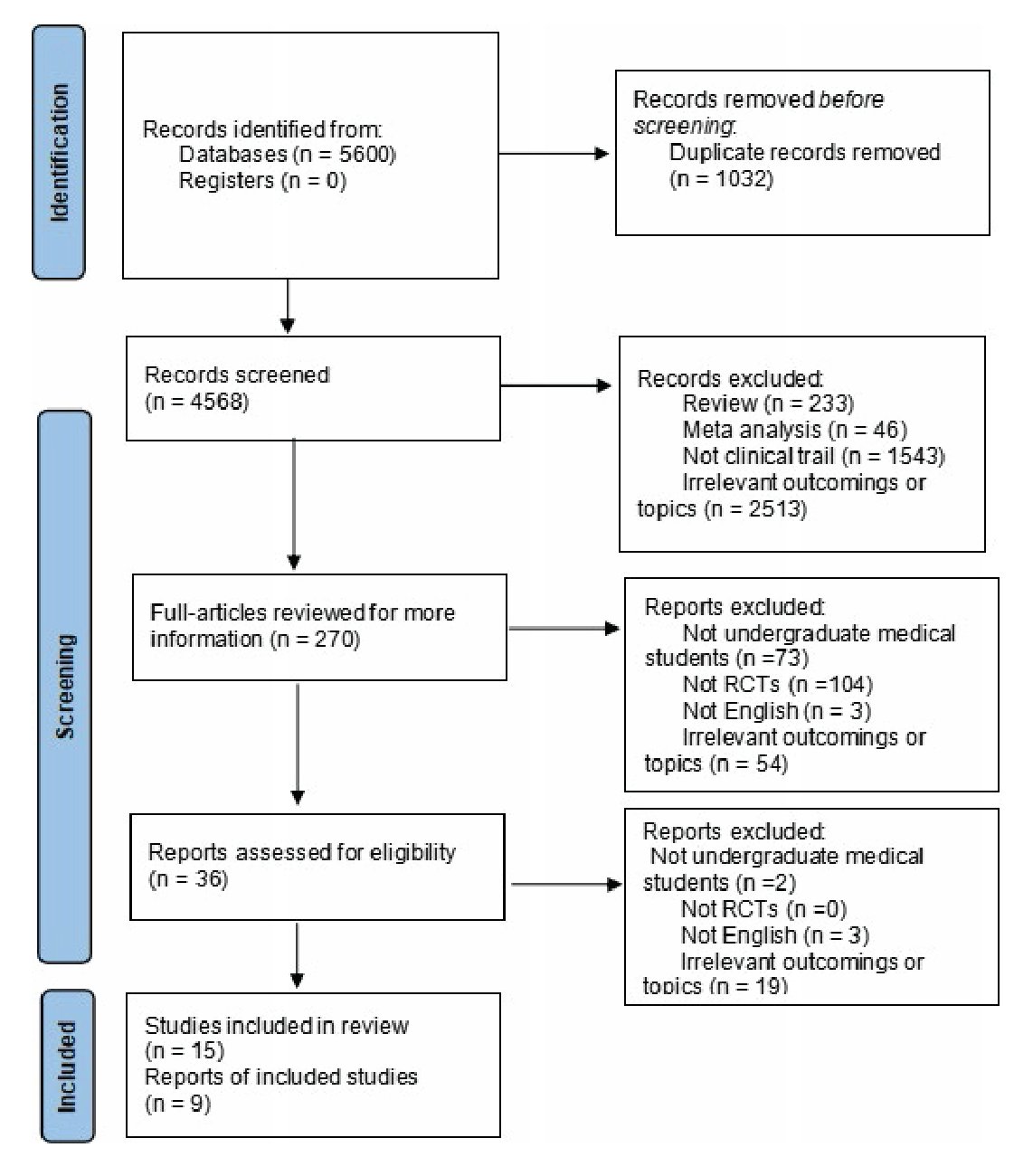
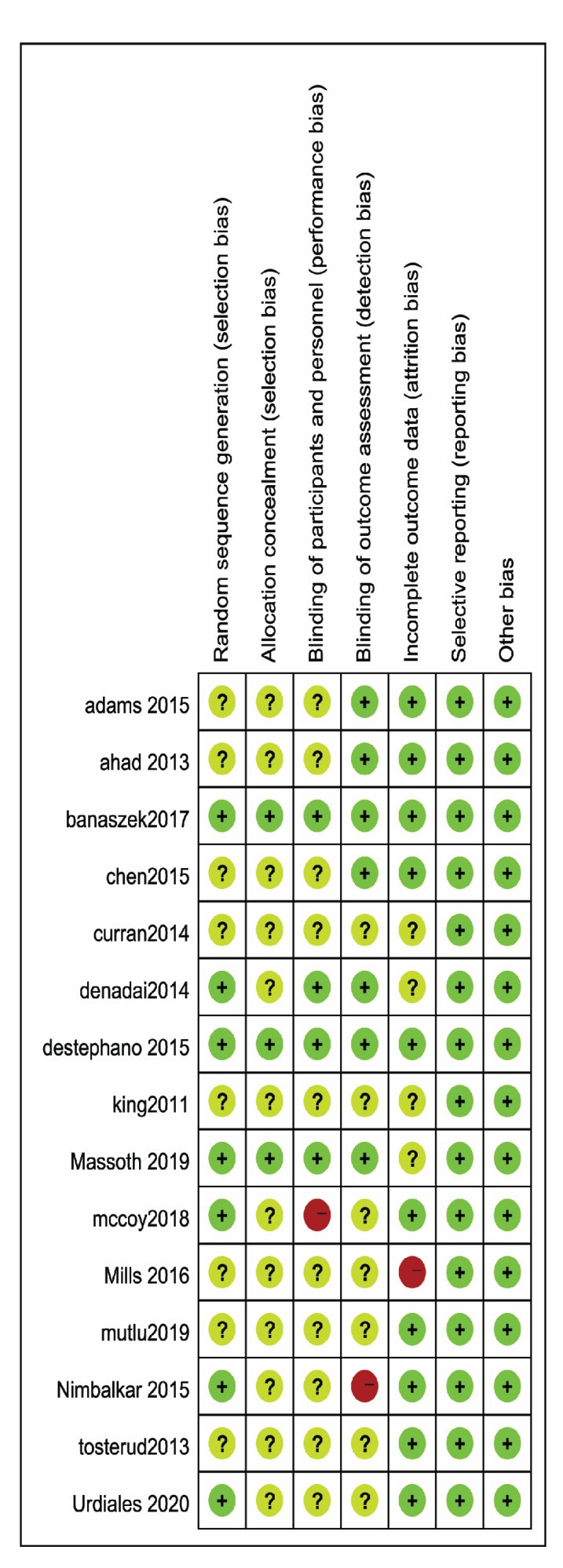
Using the above search strategy, we identified 4,568 potentially relevant studies. Fifteen of the studies met the criteria (Figure 1). The characteristics of the 15 studies included in this meta-analysis and review are listed in table 1. Random assignment was used in all the studies. Thirteen studies compared high-fidelity simulators with lowfidelity simulators, and two studies compared high-fidelity simulators with static simulators. Figure 2 summaries the risk of bias assessment. Eight studies did not describe the method of random allocation [7-14]. Three studies detailed the generation of allocation. Four studies used a blinded method, while one study clearly indicated that no blinding was used [4,15-18]. Six studies blinded the evaluators; participants in one study were randomly assigned, but the researchers who assessed their scores were not [4,7- 9,16,17,19]. One study had a risk of bias due to missing results [12]. There was a low risk of publication bias in all the studies.
Figure 1: Flow chart of study screening.
Outcomes
Six studies quantitatively compared the mastery of theoretical knowledge of undergraduate medical students exposed to HFS and LFS [4,7,9,13,19,20]. Five of these studies reported no significant difference between lowfidelity simulation and high-fidelity simulation groups [4,7,13,19,20]. One of these studies reported that highfidelity simulators are more effective than low-fidelity simulators [9]. King and Reising compared the effectiveness of static simulation and HFS in the teaching of advanced heart life support guidelines [11]. The results showed that there was no significant difference in theoretical knowledge between the static simulation group and the HFS group (P=0.1455, a=0.05).
Twelve studies evaluated students’ skill performance between high-fidelity and low-fidelity simulators, seven of these studies reported no significant difference between low-fidelity simulation and high-fidelity simulation groups, and four of these studies quantitatively compared the professional skill performance of undergraduate medical students taught via HFS and LFS [4,7-12,15-19]. Four of these studies obtained positive results: Banaszek et al., King and Reising, Mills et al. and McCoy et al. The results showed that the clinical skills performance of students in the HFS group after receiving HFS teaching was significantly different from that of students in the LFS group (P<0.05) [11,12,15,18]. One of these studies reported that low-fidelity simulation performs better than high-fidelity simulation in several subitems.
Seven studies evaluated students’ confidence between high-fidelity and low-fidelity simulators [4,10,12,14,16,17,19]. Three of these studies quantitatively compared participants’ confidence after receiving HFS and LFS teaching and training [10,14,17]. Three of these studies reported no significant difference between low-fidelity simulation and high-fidelity simulation groups [14,17,19]. One of these studies reported that students in the highfidelity manikin simulator group recorded higher scores than students in the low-fidelity manikin simulator group [10]. One of these studies reported that students in the lowfidelity simulator group were significantly more confident in their ability than students in the high-fidelity simulator group [16]. One of these studies reported that self-rated confidence was significantly overrated in the high-fidelity simulation group compared with the low-fidelity simulation group [4]. One of these studies reported that high-fidelity simulation creates a significant additional cognitive burden [12].
Table 1: Descriptions and outcomes of included studies.
| Author (Year), Study setting and participants | Description of method | Measurements of outcomes | Outcomes | |||
|---|---|---|---|---|---|---|
| Experimental group;Sample size(n) | Control group;Sample size(n) | Knowledge | Skill Performance | Confidence | ||
| Adams et al. (2015, USA)7;Random assignment;1st- 2nd year medical students AND 1st-year physician assistant students | high-fidelity simulation activities (n=9) | Low-fidelity simulation: a DARTsim electrocardiogram (ECG) software simulator (n=10) | Written posttest and Megacode performance were assessed | No significant difference between Low-fidelity simulation and high-fidelity simulation groups | Low-fidelity simulation was statistically equivalent to highfidelity simulation | Not evaluated |
| Ahad et al. (2013, USA)8;Random assignment;3rd-4th year medical students | High-Fidelity Model (n=16) | Low-Fidelity Model (n=16) | Performances was assessed by computer-based evalution parametera used on AccuTouch colonoscopy simulator | Not evaluated | No significant difference between High-Fidelity Model and Low- Fidelity Model groups | Not evaluated |
| Banaszek et al. (2017,Canada)15;Random assignment; preclerkship level medical students | a high-fidelity virtual reality arthroscopic simulation (n=16) | low-fidelity simulation: a benchtop arthroscopic setup (n=16) | Procedural efficiency was evaluated by using the Golbal Rating Scale | Not evaluated | Positive outcome:high- fidelity simulation group was superior to low-fidelity simulation group | Not evaluated |
| Chen et al. (2015, Canada)9;Random assignment;senior undergraduate nursing students | high-fidelity simulation: human patient simulator (n=21) | low-fidelity simulation: digital sounds on a computer (n=21) | auscultation tests of respiratory and cardiac sounds, observer-rated performances | Not evaluated | No significant difference between high-fidelity simulation and low-fidelity simulation groups | Not evaluated |
| Curran et al. (2015,Canada)10;Random assignment;3rd-year medical students | high-fidelity manikin simulator (n=31) | low-fidelity manikin simulator (n=35) | megacode performance of integrated skills station; participant satisfaction and confidence | Not evaluated | No significant difference between high-fidelity manikin simulation and low-fidelity manikin simulation groups | Positive outcome: students in the high-fidelity manikin simulator group recorded high score than students in the lowfidelity manikin simulator group did |
| Denadai et al. (2014, Brazil)17;Random assignment;1st-2nd year medical students | high-fidelity chicken leg skin (n=12) | low-fidelity rubberized line (n=12) | Flap performances using the Global Rating Scale; selfperceived confidence | Not evaluated | No significant difference between high-fidelity simulation and low-fidelity simulation groups | No significant difference between between high-fidelity simulation and low-fidelity simulation groups |
| King and Reising (2011,USA)11;Random assignment; senior nursing students | a high-fidelity simulation (n=24) | low-fidelity simulation: a static simulation (n=25) | written examination; megacode performance | No significant difference between high-fidelity simulation and low-fidelity simulation groups | Positive outcome: the high-fidelity simulation group outperformed the low-fidelity simulation group | Not evaluated |
| DeStephano et al. (2015, USA)16; Random assignment;2nd-4th year medical students | a high-fidelity simulation group: computercontrolled mannequin (n=47) | low-fidelity simulation group: an obstetrical abdominal-pelvic model (n=46) | performance of vaginal delivery manoeuvres; confidence to perform vaginal delivery manoeuvres | Not evaluated | No significant difference between high-fidelity simulation and low-fidelity simulation groups | students in the low-fidelity simulator group were significantly more confident in their ability than students in the high-fidelity simulator group did |
| Massoth et al. (2019,Germany)4; Random assignment; 4th-year medical students | a high-fidelity simulated Advanced Life Support training session (n=67) | a low-fidelity simulated Advanced Life Support training session (n=68) | pre- and post tests of theoretical knowledge; performance was recorded and rated | No significant difference between high-fidelity simulation and low-fidelity simulation groups | Low-fidelity simulation performs better than high-fidelity simulation in several subitems | Self-rated confidence was significantly overrated in the high-fidelity simulation than low-fidelity simulation groups |
| McCoy et al. (2019, USA)18; Random assignment; 4th-year medical students | a high-fidelity simulator (n=35) | a low-fidelity Resusci Anne cardiopulmonary resuscitation manikin (n=35) | performance in cardiopulmonary resuscitation skill | Not evaluated | Positive outcome: high-fidelity simulation is superior to lowfidelity simulation group | Not evaluated |
| Mills et al. (2016, Australia)12; Random assignment; 1st-year paramedicine students | high environmental fidelity simulations (LFenS) (n=19) | low environmental fidelity simulations (LFenS) (n=20) | psychological immersion and cognitive burden; performance | Not evaluated | Positive outcome:highfidelity simulation performs better than low-fidelity simulation group | high-fidelity simulation creates significant additional cognitive burden |
| Mutlu et al. (2019, Turkey)13; Random assignment; 3rd-4th year nursing students | high-fidelity simulators (interactive patient simulators) (n=36) | low-fidelity simulators (computer and video) (n=35) | the Auscultation Skills Form; Descriptive Information Form | Positive outcome:highfidelity simulators is more effective than low-fidelity simulators | Not evaluated | Not evaluated |
| Nimbalkar et al. (2015, Gujarat)19; Random assignment; 3rd-year medical students | SimNewB (an inter active high fidelity simulator) (n=50) | low fidelity Resusci® Baby Basic (n=51) | written test; Megacode assessment score | No significant difference between high-fidelity simulation and low-fidelity simulation groups | No significant difference between high-fidelity simulation and low-fidelity simulation groups | No significant difference between high-fidelity simulation and low-fidelity simulation groups |
| Tosterud et al. (2013, Norway)14; Random assignment; 1st-3rd year nursing students | High-fidelity patient simulator (n=29) | low-fidelity simulation group: Static mannequin (n=28) | Satisfaction and Self- Confidence | Not evaluated | Not evaluated | No significant difference between high-fidelity simulation and low-fidelity simulation groups |
| Urdiales et al. (2020, Brazil)20; Random assignment; 1st-2nd year medical students | a high-fidelity Megacode Kelly Laerdal® mannequin (n=30) | a low-fidelity model developed by the researcher (n=30) | multiple-choice test with 20 questions | No significant difference between high-fidelity simulation and low-fidelity simulation groups | Not evaluated | Not evaluated |
Discussion
This meta-analysis and review provides data for evidence-based education by comprehensively analysing undergraduate medical education under different backgrounds and types of simulation. In this study, due to the different interventions used in each study and the different evaluation methods used for outcome indicators, it is difficult to determine which intervention is more effective. Although some results are positive, it seems that there was no significant difference between HFS and LFS in terms of students’ theoretical knowledge, clinical skills or improved confidence.
Figure 2: Risk assessment diagram of studies included in the meta-analysis.
Both high-fidelity and low-fidelity simulators can improve students’ theoretical knowledge and clinical skills [19]. There is no difference in theoretical knowledge and clinical skills, and similar results have been reported in many studies [7,19,20]. These results may suggest that the teaching effect of LFS can be equivalent to that of HFS in medical undergraduate education. However, some studies have found that high-fidelity simulators are superior to low-fidelity simulators in improving students’ clinical skills [11,13].
In terms of economy, the cost and price of high-fidelity simulators are much higher than those of low-fidelity simulators [21]. This leads to the high fidelity simulator expensive cost is contradictory in an unsuccessful performance in the simulation education of undergraduate students. Second, the majority of students from both groups had strong positive expectations of the value of HFS. Before the course, only the majority of the HFS group adhered to this belief, while many participants in the LFS group changed their views and did not consider LFS training to be inferior [18]. This suggested that LFS training did not discourage participants but rather made them more confident.
As the simulation level increases, the cognitive burden of inexperienced students also increases, and the complexity of the working environment will distract students’ attention, leading to low learning efficiency and even lack of knowledge [22]. Some literature also suggests that students will feel pressured by high-fidelity simulators because of the highly simulated environment they create. However, students who have basic knowledge of clinical skills can refine their performance by entering the “deep” simulated environment of high-fidelity simulators [12]. It is completely feasible to conduct low-fiedlity simulations for students with little experience [20]. This has great educational value.
The limitations of this paper are as follows. First, the participants in our included studies were undergraduate medical students whose specific training and education levels may have influenced the outcomes in a way that is different from the way medical professionals are assessed. Second, the high heterogeneity of this study may be due to the heterogeneity of the intervention measures and measurement schemes across the included studies. This article includes only research published in English. Due to the different interventions used in each study and the different evaluation methods used for outcome indicators, it is difficult to determine which intervention is more effective by use of meta-analysis. Therefore, more clinical studies are needed to determine the relation between the fidelity of the simulator and medical undergraduate learning outcomes.
Conclusion
Due to the different interventions used in each study and the different evaluation methods used for outcome indicators, it is difficult to determine which intervention is more effective. According to the results of this study, there seems to be no positive relation between education outcomes and the fidelity of the simulator. This finding may be associated with the education level of our sample, and whether it is replicable in professional medical personnel needs further research. In terms of undergraduate medical education, HFS seems to not have high investment: high-fidelity simulator costs higher costs cannot be better performance in undergraduate medical simulation education, and the reasonableness of its use in medical undergraduate education is questionable. More clinical trials are needed to provide evidence.
Acknowledgement
We acknowledge support from the Clinical Skills Training Center, Wannan Medical College.
This work was supported by the Key Research and Development Program of Anhui Province (201904a07020034) and Funding of the “Peak” Training Program for Scientific Research of Yijishan Hospital, Wannan Medical College (GF2019G05). Anhui Provincial Quality Engineering Teaching Research Project (2019jyxm1068); Wannan Medical College Teaching Quality and teaching reform project key project (2018jyxm50).
Funding Statement
There is no funding.
Cooper JB, Taqueti VR (2004) A brief history of the development of mannequin simulators for clinical education and training. Qual Saf Health Care 13(S1): i11-i18. [ Ref ]
Bashir G (2010) Technology and medicine: the evolution of virtual reality simulation in laparoscopic training. Med Teach 32: 558-561. [ Ref ]
Deering S, Rowland J (2013) Obstetric emergency simulation. Semin Perinatol 37: 179-188. [ Ref ]
Massoth C, Röder H, Ohlenburg H, Hessler M, Zarbock A, et al. (2019) High-fidelity is not superior to low-fidelity simulation but leads to overconfidence in medical students. BMC Med Educ 19: 29. [ Ref ]
Cheng A, Lockey A, Bhanji F, Lin Y, Hunt EA, et al. (2015) The use of highfidelity manikins for advanced life support training--a systematic review and meta-analysis. Resuscitation 93: 142-149. [ Ref ]
Cumpston M, Li T, Page MJ, Chandler J, Welch VA, et al. (2019) Updated guidance for trusted systematic reviews: a new edition of the cochrane handbook for systematic reviews of interventions. Cochrane Database Syst Rev 10: ED000142. [ Ref ]
Adams AJ, Wasson EA, Admire JR, Pablo Gomez P, Babayeuski RA, et al. (2015) A comparison of teaching modalities and fidelity of simulation levels in teaching resuscitation scenarios. J Surg Educ 72: 778-785. [ Ref ]
Ahad S, Boehler M, Schwind CJ, Hassan I (2013) The effect of model fidelity on colonoscopic skills acquisition. A randomized controlled study. J Surg Educ 70: 522-527. [ Ref ]
Chen R, Grierson LE, Norman GR (2015) Evaluating the impact of highand low-fidelity instruction in the development of auscultation skills. Med Educ 49: 276-285. [ Ref ]
Curran V, Fleet L, White S, Bessell C, Deshpandey A, et al. (2015) A randomized controlled study of manikin simulator fidelity on neonatal resuscitation program learning outcomes. Adv Health Sci Educ Theory Pract 20: 205-218. [ Ref ]
King JM, Reising DL (2011) Teaching advanced cardiac life support protocols: the effectiveness of static versus high-fidelity simulation. Nurse Educ 36: 62-65. [ Ref ]
Mills BW, Carter OB, Rudd CJ, Claxton LA, Ross NP, et al. (2016) Effects of low- versus high-fidelity simulations on the cognitive burden and performance of entry-level paramedicine students: a mixed-methods comparison trial using eye-tracking, continuous heart rate, difficulty rating scales, video observation and interviews. Simul Healthc 11: 10-18. [ Ref ]
Mutlu B, Yılmaz OE, Dur S (2019) The effect of high- and low-fidelity simulators in learning heart and lung sounds by undergraduate nurses: a randomized controlled trial. Contemp Nurse 55: 351-359. [ Ref ]
Tosterud R, Hedelin B, Hall-Lord ML (2013) Nursing students’ perceptions of high- and low-fidelity simulation used as learning methods. Nurse Educ Pract 13: 262-270. [ Ref ]
Banaszek D, You D, Chang J, Pickell M, Hesse D, et al. (2017) Virtual reality compared with bench-top simulation in the acquisition of arthroscopic skill: a randomized controlled trial. J Bone Jt Surg Am Vol 99: e34. [ Ref ]
DeStephano CC, Chou B, Patel S, Slattery R, Hueppchen N (2015) A randomized controlled trial of birth simulation for medical students. Am J Obstet Gynecol 213: 91.e1-e7. [ Ref ]
Denadai R, Saad-Hossne R, Raposo-Amaral CE (2014) Simulation-based rhomboid flap skills training during medical education: comparing lowand high-fidelity bench models. J Craniofacial Surg 25: 2134-2138. [ Ref ]
McCoy CE, Rahman A, Rendon JC, Anderson CL, Langdorf MI, et al. (2019) Randomized controlled trial of simulation vs. standard training for teaching medical students high-quality cardiopulmonary resuscitation. West J Emerg Med 20: 15-22. [ Ref ]
Nimbalkar A, Patel D, Kungwani A, Phatak A, Vasa R, et al. (2015) Randomized control trial of high fidelity vs low fidelity simulation for training undergraduate students in neonatal resuscitation. BMC Res Notes 8: 636. [ Ref ]
Urdiales AIA, Struck GT, Guetter CR, Yaegashi CH, Temperly KS, et al. (2020) Surgical cricothyroidostomy. Analysis and comparison between teaching and validation models of simulator models. Rev Col Bras Cir 47: e20202522. [ Ref ]
Hauglum SD, Crenshaw NA, Gattamorta KA, Mitzova-Vladinov G (2018) Evaluation of a low-cost, high-fidelity animal model to train graduate advanced practice nursing students in the performance of ultrasoundguided central line catheter insertion. Simul Healthc 13: 341-347. [ Ref ]
Sewell JL, Maggio LA, Ten Cate O, van Gog T, Young JQ, et al. (2019) Cognitive load theory for training health professionals in the workplace: a BEME review of studies among diverse professions: BEME guide no. 53. Med Teach 41: 256-270. [ Ref ]