Journal Name: Journal of Cardiovascular Disease and Medicine
Article Type: Case Report
Received date: 12 July, 2018
Accepted date: 27 July, 2018
Published date: 03 August, 2018
Citation: Kikumura T, Tamayose S, Oroku M, Shimoji K, Shiohira Y, et al (2018) Rapid Progression of Bioprosthetic Aortic Valve Calcification in a Patient Receiving Chronic Hemodialysis: A Case Report. J Cardiovas Disea Medic Vol: 1, Issu: 1 (56-58).
Copyright: © 2018 Kikumura T, et al. This is an openaccess article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Aortic valve stenosis requiring surgical replacement is common in chronic hemodialysis (HD) patients. Bioprosthetic and artificial mechanical valves are commonly used for this purpose.
A 72-year-old man with a history of bioprosthetic aortic valve replacement 3 years prior to presentation was admitted for congestive heart failure associated with prosthetic valve dysfunction. Although his parameters indicated well-controlled chronic kidney disease-mineral and bone disorder (CKD-MBD), his resected bioprosthetic valve showed complete severe calcification. Our case indicates the importance of frequent follow-up, particularly echocardiographic assessment in HD patients with bioprosthetic aortic valve replacement.
Keywords
Aortic valve stenosis, Calcification, Chronic hemodialysis, CKD-MBD, Prosthetic valve.
Abstract
Aortic valve stenosis requiring surgical replacement is common in chronic hemodialysis (HD) patients. Bioprosthetic and artificial mechanical valves are commonly used for this purpose.
A 72-year-old man with a history of bioprosthetic aortic valve replacement 3 years prior to presentation was admitted for congestive heart failure associated with prosthetic valve dysfunction. Although his parameters indicated well-controlled chronic kidney disease-mineral and bone disorder (CKD-MBD), his resected bioprosthetic valve showed complete severe calcification. Our case indicates the importance of frequent follow-up, particularly echocardiographic assessment in HD patients with bioprosthetic aortic valve replacement.
Keywords
Aortic valve stenosis, Calcification, Chronic hemodialysis, CKD-MBD, Prosthetic valve.
Background
Dialysis patients constitute a rapidly ageing segment of the Japanese population. Based on latest reports from the Japanese Society for Dialysis Therapy, the mean age of incidence and prevalence in patients was 69.0 and 67.5 years, respectively [1]. Approximately one-fourth of cases involved patients who were ≥ 80 years of age.
Among an increasingly older dialysis population, enhanced age is also a contributing factor to the development of aortic stenosis. Aortic valve stenosis is the most common obstructive abnormality among HD patients, and it occurs most commonly in association with valvular and annular calcification.
Case Report
A 72-year-old man was admitted on December 22, 2016 with dyspnea and hypoxia. With a known history of diabetes mellitus, hypertension, colon cancer surgery, and cerebral infarction, hemodialysis (HD) was initiated in 2007 for end-stage renal disease (ESRD) secondary to diabetic nephropathy.
In August 2013, he underwent aortic valve replacement using a bioprosthetic valve to treat severe aortic stenosis. Following surgery, he resumed regular HD treatment at a clinic near his home. He was stable on a medical regimen that included candesartan, amlodipine, carvedilol, omeprazole, and aspirin. Additionally, he was prescribed calcium acetate 750 mg and sevelamer hydrochloride 750 mg with each meal and maxacalcitol 7.5 mcg and darbepoetin 60 mcg during hemodialysis.
Upon admission in 2016, his physical examination showed a blood pressure 138/77 mmHg, respiratory rate 30/minute, oxygen saturation 92% (on 28% oxygen via nasal cannula), pulse 99 beats/minute, and crackles in bilateral lung fields. There was no lower extremity edema. His body weight of 77.7 kg increased by 2.8 kg over the course of the subsequent 2 days. Laboratory results indicated the following levels: hemoglobin 11.2 g/dL, leukocyte 7,100/ μL, sodium 138 mEq/L, potassium 5.2 mEq/L, calcium 9.3 mg/dL, phosphate 5.5 mg/dL, intact parathyroid hormone (iPTH) 154 pg/mL, creatinine 15.2 mg/dL, and brain natriuretic peptide (BNP) 653.6 pg/mL.
A chest x-ray showed pulmonary edema. A transthoracic echocardiogram showed severe prosthetic valve stenosis with the valve area reduced to 0.7 cm2 (reference range: 2-4 cm2) and trans-valvular jet velocity increased to 5.4 m/s (< 2.6 m/s). The left ventricular ejection fraction was 62% and asynergy was not observed. A coronary angiogram showed 90% stenosis of the left anterior descending artery, however, fractional flow reserve was maintained. Heart failure was attributed to valvular dysfunction.
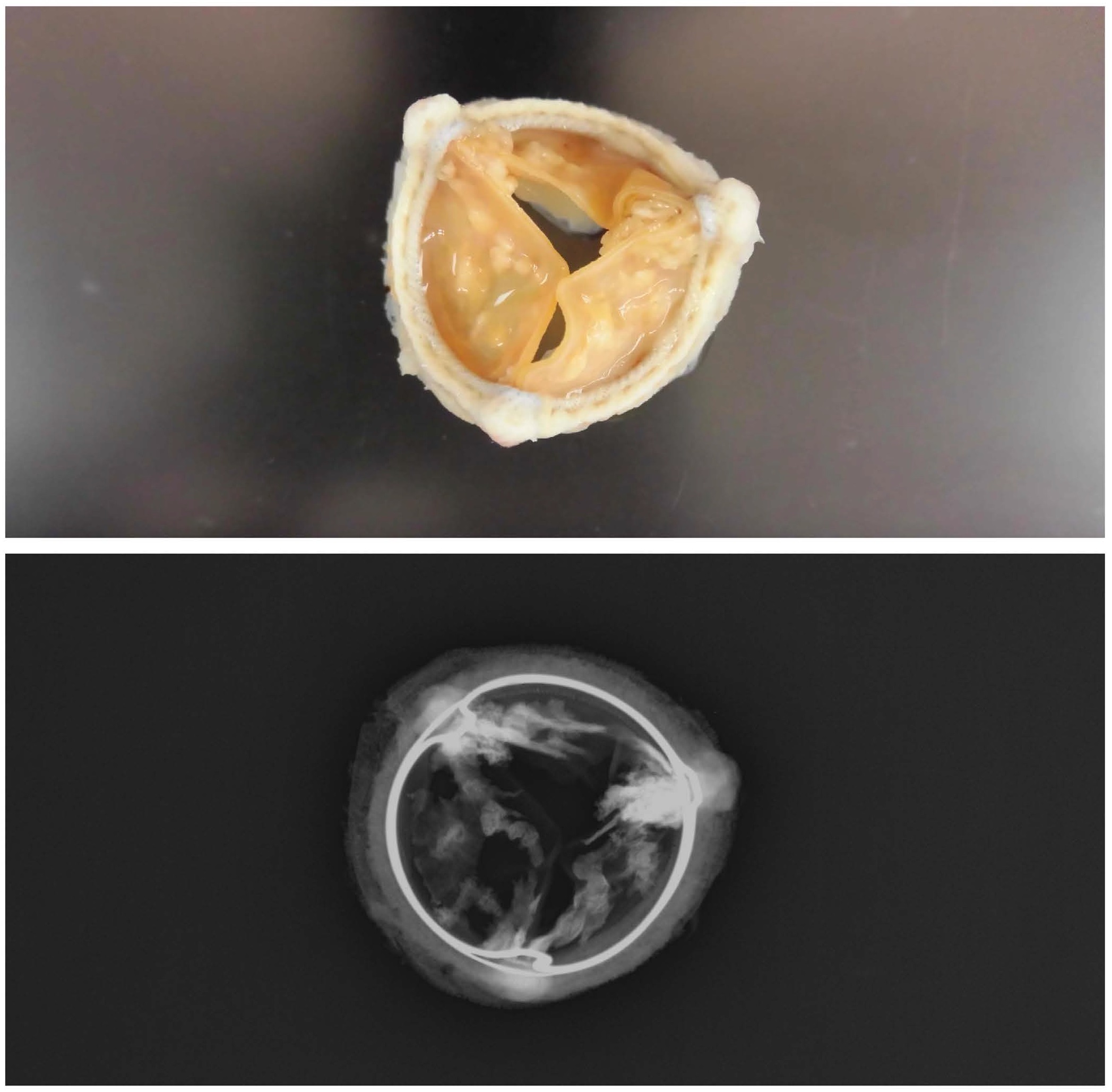
He subsequently underwent a second aortic valve replacement using a mechanical valve that was then followed by coronary artery bypass surgery. Intraoperatively, his bioprosthetic aortic valve leaflets were almost immobile due to significant calcification (Figure 1). He was discharged following a stable postoperative course and continues to receive regular dialysis at another hospital.
Figure 1: Radiologic study of resected bioprosthetic valve with calcification of the three leaflets.
Discussion
Aortic valve calcification (AVC) is a common complication in ESRD patients. AVC occurs more frequently and at a younger age in those with ESRD than in those with normal renal function [2]. Several factors related to CKD-MBD, hypertension, diabetes mellitus, and HD duration might contribute to the rapid progression of AVC [3].
The choice of prosthetic valves used in HD patients is controversial. Cardiac surgeons must weigh the risk-benefit ratio for accelerated bioprosthetic valve deterioration versus morbidity associated with anticoagulation when selecting a mechanical valve. Current European Society of Cardiology guidelines state that the use of bioprosthetic valves may be reasonable in ESRD patients [4], whereas American College of Cardiology/American Heart Association (ACC/AHA) guidelines do not mention ESRD patients when discussing prosthetic valve choice [5].
This lack of clarification must be addressed, as evidenced by our case of a patient who developed rapid calcification in his bioprosthetic aortic valve, despite well-controlled parameters of CKD-MBD. Furthermore, our case emphasizes the importance of regular follow-up and monitoring for
Acknowledgement
We thank our patient and his family for their permission to report this case.
JSDT (2018) The 64th annual meeting of the japanese society for dialysis therary [http://www.jsdt.or.jp/]. [ Ref ]
Umana E, Ahmed W, Alpert MA (2003) Valvular and perivalvular abnormalities in end-stage renal disease. Am J Med Sci 325: 237-242. [ Ref ]
Adragao T, Pires A, Lucas C, Birne R, Magalhaes L, et al. (2004) A simple vascular calcification score predicts cardiovascular risk in haemodialysis patients. Nephrol Dial Transplant 19: 1480-1488. [ Ref ]
Vahanian A, Alfieri O, Andreotti F, Antunes MJ, Barón-Esquivias G, et al. (2012) Guidelines on the management of valvular heart disease (version 2012): the Joint Task Force on the Management of Valvular Heart Disease of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS). Eur J Cardiothorac Surg 42: S1-S44. [ Ref ]
Nishimura RA, Otto CM, Bonow RO, Carabello BA, Erwin II JP, et al. (2014) 2014 AHA/ACC Guideline for the Management of Patients With Valvular Heart Disease: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation 129: 2440-2492. [ Ref ]