Journal Name: Journal of Cardiovascular Disease and Medicine
Article Type: Research
Received date: 14 September, 2019
Accepted date: 08 October, 2019
Published date: 17 October, 2019
Citation: Randle T, McMahon D, Khalid Y, Dasu N (2019) The Role of CHA2DS2-Vasc Score Vs. Anticoagulation for Predicting Morbidity and Mortality for Ischemic Bowel Disease Secondary to Atrial Fibrillation. J Cardiovasc Dis Med. Vol: 2, Issu: 1 (22-28).
Copyright: © 2019 Khalid Y. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Objective: Atrial fibrillation is a common disorder which can potentially have multiple adverse outcomes. One such outcome is the development of ischemic bowel disease. The aims of this study are: to evaluate the role of CHA2DS2-VASc score as a predictor of higher mortality in patients who have atrial fibrillation and ischemic bowel disease, i.e. if a higher CHA2DS2-VASc score is associated with higher mortality; to evaluate whether being on anticoagulation is associated with a lower mortality for such patients in this population.
Methods: This retrospective study reviewed patients admitted to three community teaching hospitals (health system) from January 1, 2016, through October 15, 2018 with the primary diagnosis of atrial fibrillation and ischemic bowel disease. The subject cohort was gathered via the use of International Statistical Classification of Diseases and Related Health Problems (ICD) 10 codes. Baseline characteristics such as age, sex, CHA2DS2-VASc Score, and mean Cr, subjects use of anticoagulation were analyzed. Hazard ratios, P-values, Confidence Intervals, and a Cox proportional-hazards model for the baseline characteristics were calculated. Kaplan-Meier curves were calculated and then plotted together for subjects on anticoagulation versus those not on anticoagulation. The area under the Receiver Operating Characteristic (ROC) curve was employed to assess the predictive power of CHA2DS2- VASc score for mortality development among ischemic bowel disease patients with atrial fibrillation.
Results: Sixty-five patients were included. The majority of the patients were older than >75 (63%), female (69%), and had established HTN (68%). The mean CHA2DS2-VASc score was 4.25 with p value <0.009. Utilizing the cox proportional-hazards model, the hazard ratios for females, patients with diabetes mellitus, and CHA2DS2-VASc score were statistically significant with p-value <0.05 and hazard ratios with confidence intervals that did not include 1. The area under the curve of ROC was 0.67, indicating a fair-to-poor marker with regards to the predictive power of CHA2DS2-VASc score for mortality development in patients with ischemic bowel disease patients and atrial fibrillation. When examining mortality in patients based on whether or not patients were on anticoagulation, the hazard ratio was 0.3588197057 (CI 0.08873281868) with P <0.05. The Kaplan-Meier curves demonstrate longer survival and less mortality for patients with atrial fibrillation on anticoagulation.
Conclusions: The predictive power of the CHA2DS2-VASc score was relatively low. Our current results show that the CHA2DS2-VASc score had a statistically significant hazard ratio, meaning that a score >4 had increased mortality. Patients on anticoagulation had less mortality than patients not on anticoagulation. Going forward, physicians should opt for anticoagulation in patients with atrial fibrillation unless it is absolutely contraindicated.
Abstract
Objective: Atrial fibrillation is a common disorder which can potentially have multiple adverse outcomes. One such outcome is the development of ischemic bowel disease. The aims of this study are: to evaluate the role of CHA2DS2-VASc score as a predictor of higher mortality in patients who have atrial fibrillation and ischemic bowel disease, i.e. if a higher CHA2DS2-VASc score is associated with higher mortality; to evaluate whether being on anticoagulation is associated with a lower mortality for such patients in this population.
Methods: This retrospective study reviewed patients admitted to three community teaching hospitals (health system) from January 1, 2016, through October 15, 2018 with the primary diagnosis of atrial fibrillation and ischemic bowel disease. The subject cohort was gathered via the use of International Statistical Classification of Diseases and Related Health Problems (ICD) 10 codes. Baseline characteristics such as age, sex, CHA2DS2-VASc Score, and mean Cr, subjects use of anticoagulation were analyzed. Hazard ratios, P-values, Confidence Intervals, and a Cox proportional-hazards model for the baseline characteristics were calculated. Kaplan-Meier curves were calculated and then plotted together for subjects on anticoagulation versus those not on anticoagulation. The area under the Receiver Operating Characteristic (ROC) curve was employed to assess the predictive power of CHA2DS2- VASc score for mortality development among ischemic bowel disease patients with atrial fibrillation.
Results: Sixty-five patients were included. The majority of the patients were older than >75 (63%), female (69%), and had established HTN (68%). The mean CHA2DS2-VASc score was 4.25 with p value <0.009. Utilizing the cox proportional-hazards model, the hazard ratios for females, patients with diabetes mellitus, and CHA2DS2-VASc score were statistically significant with p-value <0.05 and hazard ratios with confidence intervals that did not include 1. The area under the curve of ROC was 0.67, indicating a fair-to-poor marker with regards to the predictive power of CHA2DS2-VASc score for mortality development in patients with ischemic bowel disease patients and atrial fibrillation. When examining mortality in patients based on whether or not patients were on anticoagulation, the hazard ratio was 0.3588197057 (CI 0.08873281868) with P <0.05. The Kaplan-Meier curves demonstrate longer survival and less mortality for patients with atrial fibrillation on anticoagulation.
Conclusions: The predictive power of the CHA2DS2-VASc score was relatively low. Our current results show that the CHA2DS2-VASc score had a statistically significant hazard ratio, meaning that a score >4 had increased mortality. Patients on anticoagulation had less mortality than patients not on anticoagulation. Going forward, physicians should opt for anticoagulation in patients with atrial fibrillation unless it is absolutely contraindicated.
Introduction
Ischemic bowel disease consists of ischemic colitis, acute mesenteric ischemic and chronic mesenteric ischemia. The major etiology of intestinal ischemia is secondary to arterial embolism or arterial thrombosis in 50-75% of cases [1,2]. Ischemic bowel disease is a frequently misdiagnosed and overlooked disease because of its non-specific clinical manifestations in the early course of the disease and oftentimes throughout the latter course of disease. Thus, ischemic bowel disease has remained a diagnostic challenge for physicians [3]. Mesenteric ischemia, a subset of ischemic bowel disease is a gastrointestinal emergency and contributes to catastrophic outcomes including high mortality rate if the diagnosis is delayed or inappropriately managed [4]. The underlying pathophysiology of mesenteric ischemia is a mismatch of vascular supply and demand of the intestine [4]. The etiology of Ischemic bowel disease, for a significant number of patients, is secondary to atrial fibrillation. There are a multitude of complications associated with atrial fibrillation, an important one being cerebrovascular accident, which is independently a leading cause of morbidity and mortality worldwide [4]. The incidence of cerebrovascular accidents is also increasing, and stroke specifically associated with atrial fibrillation leads to severe neurological deficits with a death rate of around 70% [4,5]. The introduction of the CHA2DS2-VASc score has proved to be of high predictability for calculating the stroke risk for patients with atrial fibrillation [4]. This paper aims to analyze the use of the CHA2DS2-VASc score as a predictor of morbidity and mortality among patients who developed Ischemic bowel disease secondary to atrial fibrillation.
Approximately half of all cases of intestinal ischemia is caused by occlusive or nonocclusive disease [4]. Occlusive disease may result from arterial thrombosis, arterial embolism, or venous thrombosis. Arterial occlusion is caused as frequently by thrombus as by embolus [6]. In our study we examined clinically significant occlusive and nonocclusive disease, i.e. symptomatic patients who are hospitalized. Even with immediate aggressive intervention, these cases are associated with a mortality rate of 33% [6]. Thus, there is a need for screening tools to diagnose ischemic bowel disease earlier. Hence, our study will analyze both the role of CHA2DS2-VASc score as a predictor of higher mortality, i.e. if a higher CHA2DS2-VASc score is associated with higher mortality among this patient population; as well as to evaluate whether being on anticoagulation is associated with a lower mortality for patients with ischemic bowel disease and atrial fibrillation. Perhaps a higher CHA2DS2- VASc can be used to screen patients more aggressively for ischemic bowel; patients not on anticoagulation could also be considered higher risk and screened earlier. Nonvalvular atrial fibrillation is the most common cardiac arrhythmia, with an overall prevalence of approximately 1% [7]. The risk factors of atrial fibrillation are variable and include valvular heart disease, cardiomyopathy, congenital heart disease, and thyroid dysfunction [8]. Atrial fibrillation is an arrhythmia whose risk increases significantly with age [5]. Consequently, the prevalence of atrial fibrillation is continually increasing due to the aging of the population. Atrial fibrillation affects 1–2% of the general population, but this value is likely underestimated due to its asymptomatic course [5]. In the Rotterdam study involving the European population, the overall prevalence of atrial fibrillation was estimated to be as high as 5.5%, including up to 17.8% prevalence in adults over 85 years of age and the lifetime risk of atrial fibrillation in men and women above 55 years of age was estimated at 24.8% and 22.9%, respectively [5]. The Framingham Heart Study analyzed the impact of atrial fibrillation on the risk of stroke with increasing age, in the American population, and placed the incidence of non-rheumatic atrial fibrillation at 0.5% in the age group of 50-60 years, and 8.8% in the age group over 80 years [5]. With regards to atrial fibrillation and associated mortality, approximately 80% of embolismrelated deaths are from stroke and 20% from another systemic thromboembolism [7]. The 20% of death resulting from systemic thromboembolism includes ischemic bowel disease and is significant. Paroxysmal atrial fibrillation has not generated as much concern as permanent atrial fibrillation, although no significant differences in thromboembolic event rates between atrial fibrillation types exist [9]. The diagnosis of cerebrovascular accidents is readily made, in part due to the advancement of imaging modalities (magnetic resonance imaging and computed tomography), whereas the diagnosis of ischemic bowel disease remains much more challenging even on imaging.
Currently, many physicians and researchers stress the importance of utilizing clinical suspicion in diagnosing patients with acute intestinal ischemia. In one particular study, the rate of suspected acute intestinal ischemia prior to imaging was 31%. The diagnosis likely could have been detected in approximately 97% of radiology reports if the clinician had mentioned to the radiologist, that intestinal ischemia was part of the differential diagnoses. When the suspected diagnosis was not mentioned, the rate of detection was much lower at 81% (P=0.04). [10] Early in the course of massive intestinal infarction, only minimal symptoms may be present: leukocytosis, pain, and confusion may predominate, gastrointestinal bleeding may not be present and abdominal findings are frequently nonspecific [6]. Therefore, prompt diagnosis of acute intestinal ischemia requires a high index of suspicion and awareness of predisposing conditions, including atrial fibrillation [6]. Today, the diagnosis of Atrial fibrillation can often be made reliably with a few exceptions: the ability of echocardiography to detect left atrial appendage thrombi is limited as it oftentimes does not provide ample visualization [11]. However, if clinicians could aggressively risk stratify patients with atrial fibrillation with the CHA2DS2-VASc score and have a higher index of suspicion for patients with a higher CHA2DS2-VASc score, this could potentially significantly increase detection of intestinal ischemia and diagnose it earlier. While clinical symptoms and biological markers of tissue ischemia and acute cell lysis may commonly suggest the diagnosis of mesenteric ischemia, but clearly lack sensitivity and specificity in this setting [12]. Recently the mortality rate for acute mesenteric ischemia had remained close to 80%, despite radiological and surgical advances over the past half century [3]. As mentioned previously, the persistently high mortality rate has been attributed: to the failure in establishing the diagnosis before intestinal gangrene begins; to the high incidence of nonocclusive mesenteric ischemia, and to the progression of bowel infarction even after the primary cause has been corrected [6].
In addition to the importance of changing operative and interventional techniques, the medical management of atrial fibrillation and atherosclerotic disease has changed dramatically over the last decade [13]. Data from multiple national studies have demonstrated a considerable overall increase in the prevalence of statin, antiplatelet, and anticoagulation use over time. However, the use of anticoagulation and antiplatelet therapy, has since plateaued in more recent years. Several studies have also found significant increases in the utilization of ablation, cardioversion, and amiodarone in an effort to maintain sinus rhythm [13]. These combined efforts have been utilized in an attempt to decrease the prevalence of atrial fibrillation and to reduce the risk of adverse cardiovascular and thromboembolic events (particularly embolic events in patients with atrial fibrillation) [13]. Despite many case reports, randomized trials, advances in surgical and interventional treatments, mortality for ischemic bowel disease associated with atrial fibrillation remains high.
Previously, there have minimal human studies examining the predictive role of CHA2DS2-VASc score on outcomes for mesenteric ischemia secondary to atrial fibrillation. There have been a few studies which have examined the CHA2DS2- VASc score and its relationship to the incidence of ischemic bowel disease among patients with atrial fibrillation. One retrospective observational study revealed that a CHA2DS2- VASc score >2 predicted significantly worse outcomes for mesenteric ischemia secondary to atrial fibrillation [14]. The specific scores, i.e. 3, 4, 5, etc., however, have not been used to predict outcomes and to examine if a higher score itself correlates to a worse outcome [14]. There is also minimal data on examination of mortality among patients with ischemic bowel disease and atrial fibrillation who are either on full-dose anticoagulation, with warfarin, rivaroxaban, dabigatran, or apixaban, versus those not on anticoagulation. Previous studies have also been limited by not including other risk factors in analysis, such as alcohol use, physical activity level, smoking, etc. We believe this is important data because intestinal ischemia remains one of the most lethal and fatal conditions with high levels or mortality.
Methods
Data Source
This retrospective cohort study used dataset from our hospital system in South New Jersey, and a cohort of patients with ischemic bowel disease and atrial fibrillation was identified based on medical record numbers and International Classification of Diseases - version 10 codes. The study participants were followed up from the index date until they were no longer being followed at our health system or until the end of 06/30/18. This study was approved by the respective institutional review boards.
Sampled Participants
To evaluate the risk of ischemic bowel disease by the CHA2DS2-VASc score, we established an atrial fibrillation cohort and looked for specific characteristics. The baseline characteristics for cohort are listed in Table 1:
Table 1: Baseline Characteristics for Patient Group.
| Variable | Number n (%) |
|---|---|
| Age, year | 65 |
| <64 | 13 (20%) |
| 65-74 | 11 (17%) |
| >75 | 41 (63%) |
| Mean+/-SD | 77.7384615384615/11.831204665889 |
| Sex | |
| Male | 20 (31%) |
| Female | 45 (69%) |
| CHA2DS2-VASc Score | |
| CHF | 17 (26%) |
| HTN | 44 (68%) |
| Diabetes mellitus | 22 (34%) |
| Vascular Disease | 35 (54%) |
| Mean Cr | 1.65184615384615/1.26663788766227 |
| Mean CHA2DS2-VASc Score | 4.24615384615385/1.87941787223106 |
| Mean follow-up, y | 3 |
Study Endpoints
The patients were followed for a total of 3 years: until death occurred, until the patients were lost to follow up, or until they were no longer followed in the hospital system.
Statistical Analysis
The proportional distributions of demographic status, and the comorbidities were compared. The continuous data was compared with Student’s t-test. The incidence density rates of mortality were calculated. To present the risk of mortality in patients with both atrial fibrillation and ischemic bowel disease stratified by all of the baseline variables, the Hazard Ratios (HRs) and 95% Confidence Intervals (CIs) were estimated with univariable and multivariable Cox proportional hazard models. Cumulative incidence curves of mortality were plotted with the Kaplan–Meier method, and the differences in curves between the group with anticoagulation versus the group without anticoagulation were examined using a log rank test. For the CHA2DS2-VASc score, this study also quantified the area under the curve for the ROC curve in order to determine if the CHA2DS2-VASc score could be a useful marker to predict morbidity and mortality for patients with both ischemic bowel disease and atrial fibrillation. All statistical analyses were performed using Microsoft excel, real statistics, and the analysis tool Pak. The level of significance was set at 0.05 using a 2-tailed student t-test.
Design
This is a retrospective observational study, patient records were reviewed and analyzed using qualitative methods. Secondary data collection was based upon data available from previous studies and current hospital databases.
Results
A total of 65 patients with both atrial fibrillation and ischemic bowel disease (acute mesenteric ischemia, chronic ischemic bowel disease, etc.), were enrolled in this study at our hospital system comprising 3 different hospitals with 3 different patient populations. The majority of the patients were older than >75 (63%), female (69%), and had established HTN (68%) [Table 1]. The mean CHA2DS2-VASc score was 4.25 with p value <0.009.
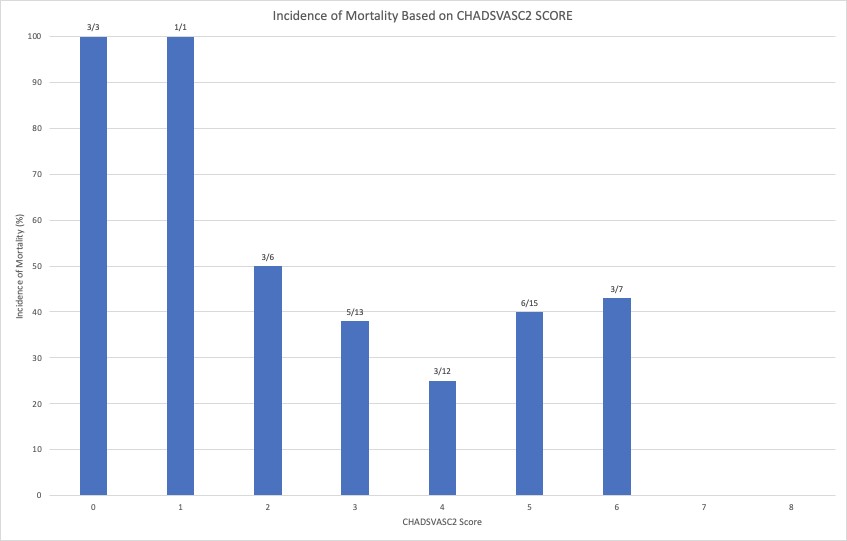
A cox proportional-hazards model (a regression model used for investigating the association between the survival time of patients and one or more predictor variables), was used to analyze the baseline characteristics of the patients via the real statistics software for excel. Cox regression analysis revealed the following characteristic in Table 2 for each patient: Based on the cox proportional-hazards model, only the hazard ratios for females, patients with diabetes mellitus, and CHA2DS2-VASc score >4 were statistically significant with p-value <0.05 and hazard ratios with confidence intervals that did not include 1. These results show that females were 3.37 times more likely to experience mortality, patients with diabetes were 2.64 times more likely to experience mortality, and the lower the CHA2DS2-VASc <4, the lesser the mortality (38% less) than a higher CHA2DS2-VASc score. However, the observed results showed that the incidence of mortality was actually higher in patients with lower CHA2DS2-VASc score <4 than patients with higher CHA2DS2-VASc score >4. The following histogram illustrates the incidence rate of mortality in terms of percentage: (Figure 1)
Table 2: Hazard Ratios, P-values, and Confidence Intervals for Baseline Characteristics
| Variable | Number n (%) | P-value | HR w/ CI |
|---|---|---|---|
| Age, year | 65 | ||
| <64 | 13 (20%) | ||
| 65-74 | 11 (17%) | ||
| >75 | 41 (63%) | ||
| Mean+/-SD | 77.7384615384615/11.831204665889 | 0.87 | 0.99 (0.96-1.04) |
| Sex | |||
| Male | 20 (31%) | ||
| Female | 45 (69%) | 0.02 | 3.37 (1.14-9.92) |
| CHA2DS2-VASc Score | |||
| CHF | 17 (26%) | 0.98 | 1.01 (0.47-2.87) |
| HTN | 44 (68%) | 0.36 | 1.57 (0.59-4.12) |
| Diabetes mellitus | 22 (34%) | 0.04 | 2.64 (1.04-6.66) |
| Vascular Disease | 35 (54%) | 0.74 | 1.16 (0.47-2.87) |
| Mean Cr | 1.65184615384615/1.26663788766227 | 0.0001 | |
| Mean CHA2DS2-VASc Score | 4.24615384615385/1.87941787223106 | 0.009 | 0.62 (0.43-0.89) |
| Mean follow-up, y | 3 |
Figure 1
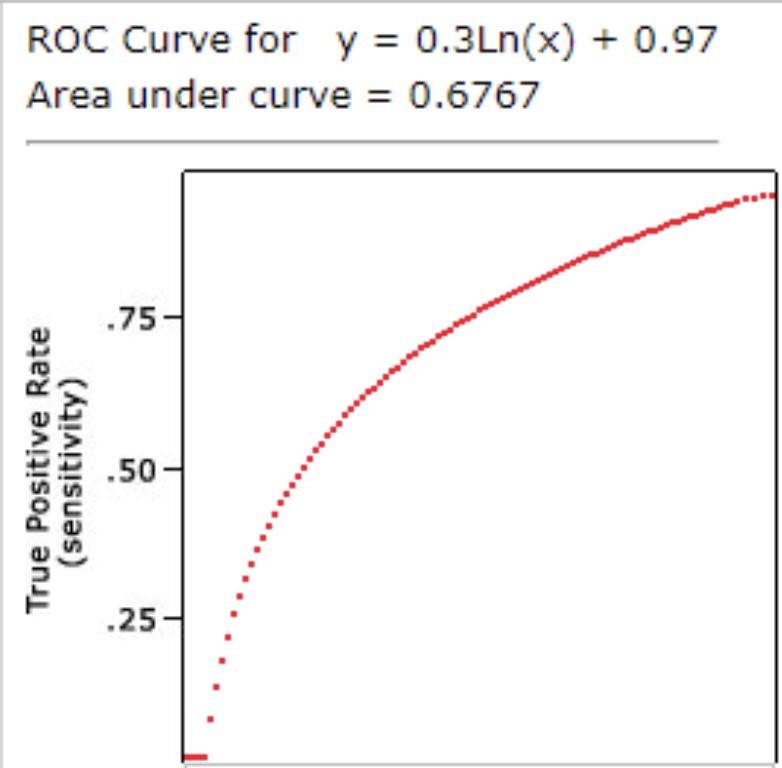
The area under the Receiver Operating Characteristic (ROC) curve was used to assess the predictive power of CHA2DS2-VASc score for mortality development among ischemic bowel disease patients w/ atrial fibrillation. The results were the following: (Figure 2)
Figure 2
The area under the curve of ROC was 0.67 indicating a fair-to-poor marker.
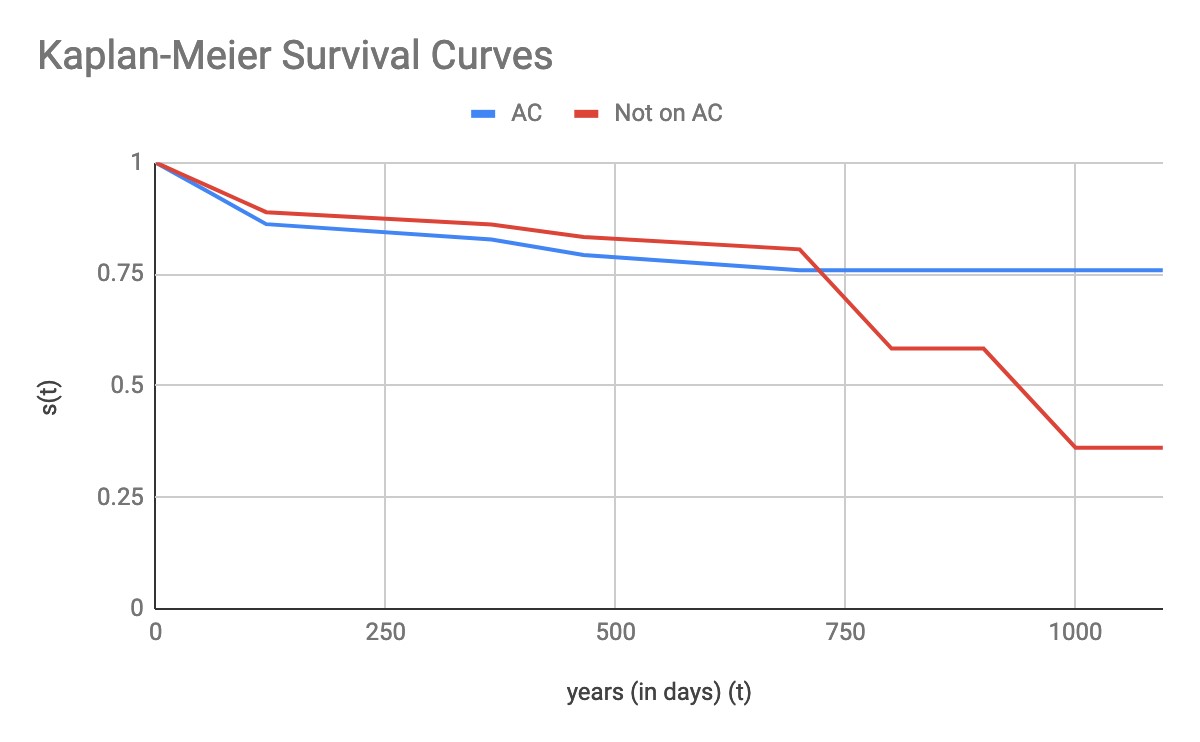
When examining mortality in patients based on whether or not patients were on anticoagulation, the hazard ratio was 0.3588197057 (CI 0.08873281868) with P <0.05 for patients on anticoagulation, meaning that patients on anticoagulation had 64% less mortality than those not on anticoagulation. Finally, utilizing the log-rank test, Kaplan-Meier curves were calculated and then plotted together for patients on anticoagulation and those not on anticoagulation: (Figure 3)
Figure 3
The Kaplan-Meier curves demonstrate longer survival and less mortality for patients with atrial fibrillation on anticoagulation. This effect was not seen immediately, but starting at 750 days after following the patients, there was significantly more mortality for patients not on anticoagulation.
Discussion
Ischemic bowel disease can be considered an intestinal disease equivalent in nature to ischemic heart disease, comparatively, ischemic bowel disease has a high-mortality rate despite the latest advances in imaging modalities and in healthcare [15]. The results of our study demonstrate that both the CHA2DS2-VASc score and whether or not a patient is on anticoagulation can help risk stratify patients with atrial fibrillation who are at a much higher risk for ischemic bowel disease. Using this information, clinicians can have an even higher index of suspicion for detecting ischemic bowel disease earlier. The cox proportional hazards model revealed that mortality was increased in females, patients with diabetes and those with lower CHA2DS2-VASc scores (<4). Moreover, patients in other retrospective studies analyzing this same patient population had a higher mean CHA2DS2- VASc score than those patients, further emphasizing that ischemic bowel disease is usually associated with a delay in diagnosis because of the initial vague clinical presentations [3]. We recommend that it is beneficial for female patients, diabetics, and patients with higher CHA2DS2-VASc scores to be monitored more closely if they have ischemic bowel disease and there needs to be a higher index of suspicion for diagnosing new-onset ischemic bowel disease in patients with atrial fibrillation. For this sample size of 65 patients, hazard ratios for males, age, and vascular disease were not statistically significant. This does not mean that these variables are completely insignificant for future studies. Given a different population and larger sample size, future studies could examine the hazard ratios for male gender, age, and vascular disease. Among several retrospective studies heart failure was the predominant factor causing intestinal hypoperfusion [16]. However, in our study patients with heart failure were not found to have statistically significant hazard ratios. Risk factors for developing ischemic bowel disease among patients with atrial fibrillation include smoking, hypertension, dyslipidemia, higher age, and female sex [17]. We were able to examine all of these risk factors except for smoking.
The receiver operating characteristic area under the curve for CHA2DS2-VASc score as predictor of morbidity and mortality for patients with both atrial fibrillation and ischemic bowel disease was 0.67. Based on standard analysis, this likely means that the CHA2DS2-VASc score is a poor-to-fair predictor based on this population and sample size. However, if the sample size was larger and the power of the study was even higher, we hypothesize that the CHA2DS2-VASc score would likely be an excellent predictor of mortality in this patient population and the area under the receiver operating characteristic curve would be >0.9.
The hazard ratio for patients on anticoagulation versus not on anticoagulation was 0.3588, This means that at any particular time, patients in the treatment group, (those on anticoagulation), were 64% less likely to experience mortality compared to the control group (patients not on anticoagulation). This result is backed by the Kaplan-Meier survival curves which show less mortality for patients on anticoagulation. These results prove that being on anticoagulation is a protective factor from death for patients with both ischemic bowel disease and atrial fibrillation. Patients with atrial fibrillation with CHA2DS2-VASc score 2 or higher should definitely be placed on anticoagulation unless there are strong absolute contraindications present.
For chronic mesenteric ischemia independent predictors of readmission to hospital at 30 days included non-elective index admission, chronic kidney disease, discharged with home health care, or discharged to a skilled nursing facility [18]. Interestingly, neither female sex, which accounted for 70% of the overall patient population, nor increasing age, was independently associated with readmission [18]. Our project did not separate patients based on acute or chronic ischemic bowel disease; this will need to be investigated in future studies.
Limitations
There were limitations to this study. The patients could have been stratified even further. This study did not include patients with mechanical valves. It did not take into account whether or not the patients were taken for procedures, such as angiography and embolization or exploratory laparotomy, and the impact of procedures on mortality. Whether or not patients were taken for surgery or embolization could have confounded the final results. This could have impacted mortality as patients could have either survived longer or survived for a shorter time, based on the procedure they underwent. The patients could have also been stratified into those with acute ischemic bowel disease versus patients with chronic ischemic bowel disease. We did not take into account whether or not the patients had paroxysmal atrial fibrillation or permanent atrial fibrillation. These are all variables that can be examined in future studies.
The diagnoses were established by the International Statistical Classification of Diseases and Related Health Problems (ICD) codes, and some investigators might challenge the diagnostic accuracy [4]. Another factor that could have limited diagnostic accuracy was that most of the cases of ischemic bowel disease were diagnosed with computed tomography scans (CT), only a few cases were diagnosed with biopsy results or angiography- which is the gold standard. In one study, 35 patients for whom a CT scan was performed at the referring center, 25 were considered to be appropriately diagnosed; however, only 1 was considered to have been appropriately diagnosed in the 19 patients for whom a CT scan was not performed at the referring center [10]. Based on these small results, it is possible that detection bias could have been in our study because almost all patients were diagnosed by CT scan. There is also a lack of data regarding ablation therapy and left atrial occlusion devices in this population. There is a growing experience of direct oral anticoagulants for intracardiac thrombi. Warfarin is still appropriate for patients with prosthetic heart valves and left ventricular assist devices. [19]. Delays in sinus rhythm restoration may accelerate adverse atrial remodeling, leading to earlier arrhythmia recurrence and accelerating referral for AF ablation [20]. We did not examine any other means of treating atrial fibrillation except for anticoagulation. Not many of our patients were treated with ablation or Watchman at our hospital system. Although, it is rare for ischemic bowel disease to occur during optimal anticoagulation therapy, a significant amount of our patients developed ischemic bowel disease while on anticoagulation [21]. Finally, our investigation is a retrospective observational study which inherently has certain methodological drawbacks.
Conclusion
In conclusion, this study is novel because there are very few studies which have investigated the predictive role of CHA2DS2-VASc score and use of anticoagulation to analyze the outcomes, specifically morbidity and mortality for ischemic bowel disease among patients who also have atrial fibrillation. The predictive power of the CHA2DS2-VASc score was relatively low. However, we hypothesize that given a larger sample size of patients and thus more power, the ROC curve for the CHA2DS2-VASc score would be >0.9 and it would likely be an excellent predictor of mortality. Our current results show that the CHA2DS2-VASc score had a statistically significant hazard ratio, demonstrating a score greater than 4 was associated with higher mortality. Patients on anticoagulation also had less mortality than patients not on anticoagulation. Further studies are necessary to confirm our findings. Going forward, we recommend that physicians should opt for anticoagulation in patients with atrial fibrillation and ischemic bowel disease, unless anticoagulation is absolutely contraindicated because being on anticoagulation is likely a protective factor against the morbidity and mortality seen in this patient population.
There are no references