Journal Name: Journal of Clinical Case Reports and Trials
Article Type: Case Report
Received date: 04 June, 2018
Accepted date: 18 June, 2018
Published date: 25 June, 2018
Citation: Elnaggar TM, El-Kased AF, El-Fol HAEK, El-Elaimy MMA, Alzaqri WA, et all. (2018) Evaluation of Facial Lymph Node Metastasis in Head and Neck Carcinoma. J Clin Case Rep Trials. Vol: 1, Issu: 1 (13-17).
Copyright: © 2018 Elnaggar TM, et al. This is an openaccess article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Back ground and objective: Supramandibular Facial lymph nodes (SFLNs) are one of the unusual sites of lymph nodes metastases. This prospective study investigated possible involvement of SFLNs in cases of head and neck carcinoma.
Patient and methods: It involves 30 neck dissections obtained from 30 patients (22 males and 8 females) with squamous cell carcinoma of the scalp, eyelid, oral cavity, lip, and parotid gland carcinomas, without locoregional recurrence or distant metastases. The tumor site was the scalp (n = 3), eyelid (n = 2), lip (n = 2), parotid (n = 6), tongue (n =5), alveolar margin (n = 5), and buccal mucosa (n = 7).
Result: Histopathological examination of the removed SFLN nodes proved positive for metastases in 9 neck dissections; 2 cases (22.2%) of lip SCC, 3 cases (33.3%) of alveolar margin SCC, and 4 cases (44.4%) of buccal mucosa SCC.
Conclusion: SFLNs are a probable site of lymph node metastases in SCC of the lip, alveolar margin, and buccal mucosa. Careful dissection above the lower margin of the mandible can safely remove these nodes without significant injury of the marginal mandibular branch of the facial nerve.
Keywords
Supramandibular lymph nodes, Facial nodes, Neck dissection, Node metastasis.
Abstract
Back ground and objective: Supramandibular Facial lymph nodes (SFLNs) are one of the unusual sites of lymph nodes metastases. This prospective study investigated possible involvement of SFLNs in cases of head and neck carcinoma.
Patient and methods: It involves 30 neck dissections obtained from 30 patients (22 males and 8 females) with squamous cell carcinoma of the scalp, eyelid, oral cavity, lip, and parotid gland carcinomas, without locoregional recurrence or distant metastases. The tumor site was the scalp (n = 3), eyelid (n = 2), lip (n = 2), parotid (n = 6), tongue (n =5), alveolar margin (n = 5), and buccal mucosa (n = 7).
Result: Histopathological examination of the removed SFLN nodes proved positive for metastases in 9 neck dissections; 2 cases (22.2%) of lip SCC, 3 cases (33.3%) of alveolar margin SCC, and 4 cases (44.4%) of buccal mucosa SCC.
Conclusion: SFLNs are a probable site of lymph node metastases in SCC of the lip, alveolar margin, and buccal mucosa. Careful dissection above the lower margin of the mandible can safely remove these nodes without significant injury of the marginal mandibular branch of the facial nerve.
Keywords
Supramandibular lymph nodes, Facial nodes, Neck dissection, Node metastasis.
Introduction
Tumor lymph drainage is usually along well recognized lymphatic pathways, but rarer lymph node sites can be involved and may be the only site of the disease, particularly in recurrence [1].
Facial lymph nodes are one of the unusual sites of lymph node metastases. They comprise four groups including mandibular, buccinators, infraorbital, and malar. The mandibular lymph nodes are also known as supra mandibular facial lymph nodes (SFLNs) [2,3]. These lymph nodes are mobile structures lying within the soft tissues of the cheek between skin and buccinators muscle at the anterior border of the masseter muscle and are closely related to the mandibular branch of the facial nerve and facial vessels. The presence of facial lymph nodes and their significance in the diagnosis and spread of malignant disease has received little attention in the literature. Facial lymph nodes are one of the unusual sites of lymph nodes metastases in head and neck SCC [4].
There is no consensus whether facial lymph nodes should be included in neck dissection for treatment of head and neck cancer. Facial lymph nodes and their involvement in oral cancer have been discussed in literature since 1971 by Jeffery Robins, but there are no sufficient data in the literature handling these nodes. Adding to the problem, most of the existing studies are based on retrograde studies that do not clarify the exact figures for these nodes [3].
During neck dissection for head and neck cancer, surgeons did not usually extend their dissection above the inferior border of the mandible where supramandibular facial lymph nodes (SFLN) are, but they keep the inferior border of the mandible as the upper limit of their flaps. Thus, although there are many data on metastases in various neck lymph nodes from head and neck SCC, yet there are few data on SFLNs. In fact, surgeons hesitate in handling the supramandubular facial lymph nodes (SMFLN) because of their close relationship to the marginal mandibular branch of the facial nerve (MM/FN) [5].
The mandibular and cervical branches of the facial nerve arise from the cervicofacial division of the facial nerve. Thus, the lower division of the facial nerve passes lateral to the retromandibular (posterior facial) vein within the substance of the parotid gland in more than 90% of cases; in others it passes medial to the vein. Injury to the mandibular branch of the facial nerve results in a very slight drooping of the angle of the mouth. The drooping is not noticeable when the mouth is in response – only when it is in motion (smiling). Depending on the nature of injury, the drooping may be neuropraxia (temporary), or permanent [2].
In this prospective study we evaluated the frequency of facial lymph nodes involvement in cases of head and neck cancer and incidence of injury to branches of facial nerve in case of facial lymph nodes dissection.
Patient and Methods
This prospective study was performed in surgical oncology department, faculty of medicine Menofia University between March 2014 and March 2018 after approval by the hospitals Ethics Committees. It involved 30 neck dissections obtained from 30 patients with head and neck cancers. Patients included had a primary carcinoma in the head and neck. Patients with locoregional recurrence, distant metastases or with neoadjuvent therapy were excluded from the study.
Resection of the primary tumors of the skin, and oral cavity SCC was performed with 1-2 cms safety margins, wide surgical excisions with safety margins, hemiglossectomy, and, or hemimandibulectomy according to the anatomical location of the primary tumor, while total parotidectomy was performed for cases of parotid gland carcinomas. Neck management included modified neck dissection (FND), and, or supraomohyoid neck dissection depending on the primary tumor size, location, clinical presentation, and involvement of cervical lymph nodes.
Postoperatively, patients with unfavorable pathologic features including involved margins, nodal extracapsular extension, > 2 positive cervical lymph nodes, perineural invasion, or lymphovascular permeation were scheduled to receive adjuvant concurrent chemoradiation.
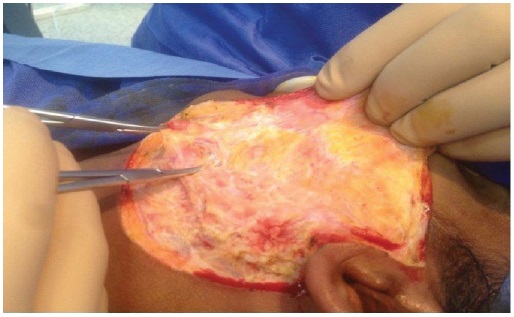
During neck dissection, lymph nodes above the inferior border of the mandible were considered the supramandibular facial lymph nodes (SFLN) Figure 1. They were usually 1-3 nodes lying close to the facial artery and vein. The area was dissected carefully for conservation of the marginal mandibular branch(s) of the facial nerve. For this purpose, we performed the incision 4 cm below the inferior border of the mandible followed by careful dissection (with flap retraction) through superficial layer of the deep cervical fascia, the incision and undermining of the fascia extended to 1.5 cm inferior to the mandible to protect the nerve.
Figure 1: Identification of facial lymph nodes in a case of parotid adenoid cystic carcinoma and its relation to marginal mandibular nerve.
Pathological analysis
The histopathological examination of the primary tumor site, the SFLN and the neck lymph nodes was performed separately to verify the differentiation grade and the nodal micrometastasis. Routine examination of all components of the specimen was done using H&E stained sections after fixation in neutral buffered formalin. The number, size and cut sections of SFLNs were recorded separately. SFLNs were examined by multiple step sections technique and the sizes of metastatic deposits were recorded using the micrometer lens.
Results
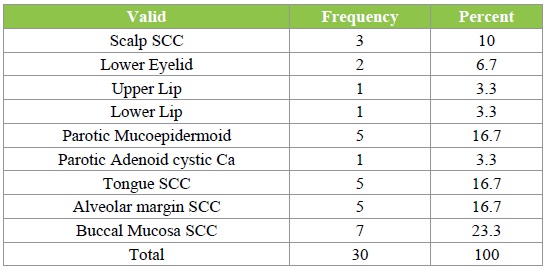
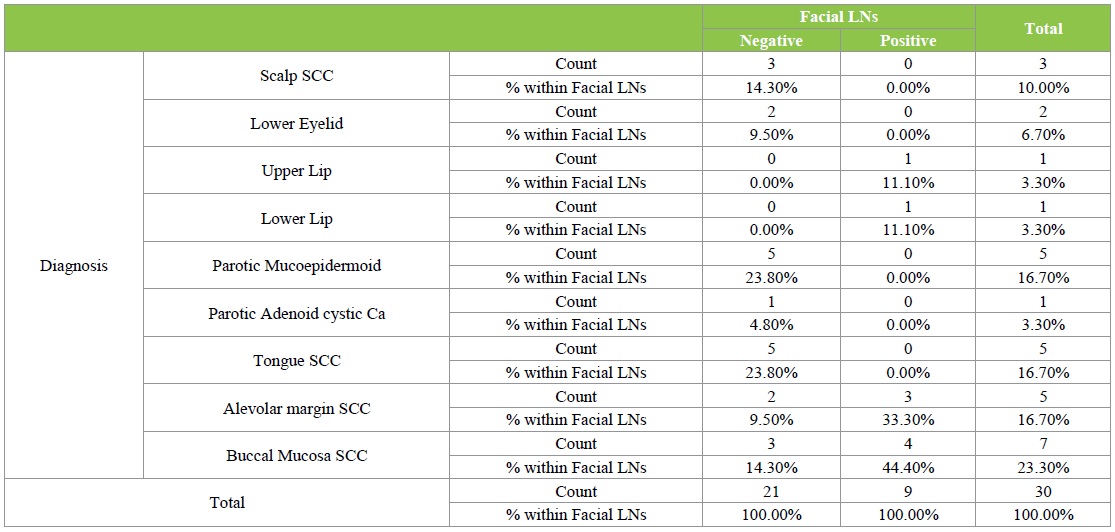
Out of 30 patients; 22 males (73.3%) and 8 females (26.7%) with a male to female ratio of 2.75:1 Table 1. The age of the patients ranged from 39-67 years with a mean of 55.2 + or – 7.6 years. The tumor site was the scalp in 3 cases (10%), lower eyelid in 2 cases (6.7%), lip in 2 cases (6.6%), parotid gland in 6 cases (20%), tongue in 5 cases (16.7%), mucosa of the alveolar margin in 5 cases (16.7%), & buccal mucosa in 7 cases (23.3%) Table 2.
Table 1: Male to female ratio and their frequency.
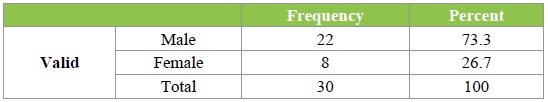
Table 2: Primary site of cancer and its frequency.
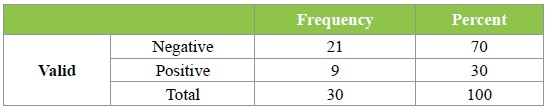
According to the clinical TNM staging system, the tumor size of the primary sites was T1 in 7 patients (23.3%), T2 in 18 patients (60%), T3 in 3 patients (10%), and T4 in 2 patients (6.7%). For clinical neck lymph node involvement, 16 patients had no clinically palpable neck lymph nodes (N0) (53.3%) at the initial examination; the rest of them (14 patients) had clinically palpable neck lymph nodes (N+) (46.6%) Table 3. More precisely, 16 patients fell into category N0, 10 patients in to category (N1), and 4 patients into category (N2) Table 4. Regarding the grade of the primary tumor, it was noticed that 55.6% of grade 2 tumors were accompanied with metastatic facial lymph nodes, this percentage declined to 44.4% in grade 3 tumors, and was 0% in grade 1 tumors.
Table 3: Clinical TNM staging system.
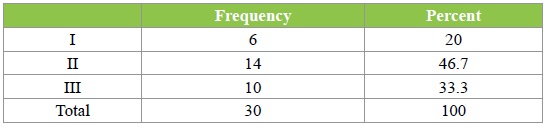
Table 4: Cervical N Staging.
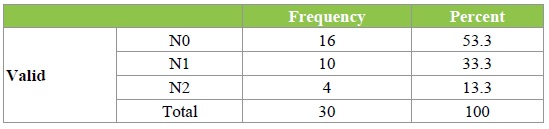
Table 5 shows a trend towards involvement of SFLN in cases of SCC of lips, mucosa of the alveolar margin, and buccal mucosa.
Table 5: Involvement of SFLN in cases of SCC of lips, mucosa of the alveolar margin, and buccal mucosa.
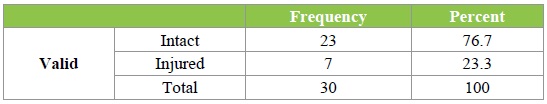
The injury of the marginal mandibular branch of the facial nerve occurred in 7 cases Table 6. The nerve function was regained during the first 2 months postoperatively in 5 cases, which was considered temporary nerve affection. 2 cases retained abnormal lower lip function for the whole 6 postoperative months, which was considered as a permanent injury.
Table 6: Marginal nerve dysfunction after neck dissection.
Histopathological examination of the removed SFLNs proved positive for metastasis in 9 neck dissections; 44.4% were SCC of the buccal mucosa Table 7.
Table 7: Involvement of SFLNS in neck dissection by histopathologic analysis.
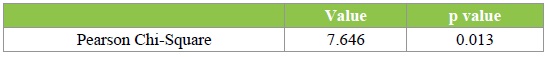
According to Chi-Square Tests, the 7 positive SFLNs showed the.013 of P value Table 8.
Table 8: Ratio of positive SFLNS according chi-square test.
Discussion
The existing literature has not yet elucidated the question of what impact metastasis to facial lymph nodes have on treatment of head and neck carcinoma. Cervical lymph node metastases are the single most important prognostic factor in head and neck cancer patients. Carcinoma of the oral cavity is most often treated by surgical resection and is associated with clinically evident disease in one third of the cases and have a high rate of occult metastatic disease in the N0 neck [6].
The fear that supraomohyoid neck dissection encircling levels I, II, &III, doesn’t satisfy the requirements of a staging dissection in oral cavity SCC has been increasing during the past few years. Many studies investigated whether level IV should be included in the treatment of N0 and even N1 necks of patients with oral cavity carcinoma. It has been evident that each specific site of primary oral cancer should be managed in a specific way in terms of extent of resection, safety margin, extent and pattern of lymph nodes to be included in surgery [7].
The current study raises the question of fear of micrometastases above level I; the supramandibular facial lymph nodes SFLN. By far, there is no consensus on the way of handling facial lymph nodes in cases of oral cavity carcinoma, rather than head and neck carcinoma in general. The subgroup of SFLN is the most interesting group of facial lymph nodes during surgical treatment of head and neck carcinoma, because of their close relationship with critical anatomic structures. The SFLN anatomic location poses serious danger during surgical handling, making the surgical procedures very demanding. Surgical intervention in this region carries a high risk of marginal mandibular nerve injury, result in various functional and cosmetic problems, which has a major impact on the patient’s quality of life.
What hinders the correct evaluation of the facial lymph nodes preoperatively is the fact that our capability of representing them with accuracy on the CT or MRI scans that we carry out before operations is limited. All of the treatment evaluation methods, like palpation and US yield results that are significantly different than those yielded from the histopathological results, suggesting that no pretreatment studies can accurately assess the requirement to histopathologically stage the neck. Ultrasonography findings are more correlated with the pathological findings than palpation, but CT gives the most effective and reliable results when it is combined with US in neck staging. Up to date there is no other diagnostic method that is reliable and show high accuracy for prediction of lymph node involvement other than the histopathological examination of head and neck lymph nodes.
For now, we use US, CT, combined with clinical palpation to determine our final diagnosis. It is not possible to scan level II by using US, however ultrasound can be useful in examination of levels I, and II a where it is difficult to use CT. In addition, CT imaging is necessary for detection of deep cervical lymph nodes. Therefore, CT should be the first choice in detecting metastatic nodes, while US could be performed for a more detailed study of suspected nodes. Management of non-palpable lymph nodes remains controversial and imaging can influence treatment. Therefor greater accuracy is required from the imaging techniques [8].
The results of our study justify the fear of micrometastases including the SFLN, in cases of buccal mucosa, alveolar margin mucosa, and lips SCC. SFLN were positive in 44.4% of buccal mucosa SCC, 33.3 % of alveolar margin SCC, and 100% of lip SCC cases. On the other hand, cases of SCC of the tongue, parotid carcinomas, scalp and eyelid SCC had negative SFLN.
Similar to our findings, Maruyama observed no lymph node metastases histopathologically in the superficial fatty tissues containing the mandibular branch of the facial nerve in 26 cases of T2 tongue carcinoma. Chong and Fan studied the records of 1916 patients with a histologically confirmed nasopharyngeal carcinoma. They reported 0.2% affection of facial nodes in their series [4]. Sheahman et al discovered metastases in 17 cases out of 29 with various types of oral and oropharyngeal carcinoma [9]. Nodal metastases were more frequent in patients with palpable neck lymph nodes. They concluded that the detection of positive facial lymph nodes is linked to a high risk of treatment failure as well as to poor prognosis [4,9].
Pestinis et al reported that patients with SCC of the oral cavity, regardless of their individual characteristics, have 13.9% possibility of metastases in the SFLN. They studied 43 patients [10]. None of them had clinically palpable SFLN at initial examination. The authors speculated that facial lymph nodes may be affected by metastases from submandibular lymph nodes, which are very close and receive lymph from them [10].
Sheahan et al stated as early as 2003, in his study on 76 cases of oral SCC where he dissected the supramandibular facial lymph nodes separately, and he found these nodes diseased in 24% of cases [2]. He found the sites of the primary disease in patients with facial lymph node metastases were retromandibular trigone, floor of mouth, buccal mucosa, and tongue base. He also stated that there was no difference in the T classification of the primary tumor between patients with positive and negative nodes [2].
Yanai et al noted metastases in supramandibular facial lymph nodes in patients previously treated for oral SCC. The primary lesions were in the buccal mucosa, maxillary gingiva, maxillary sinus, and tongue. In their study, the incidence of recurrence to facial lymph nodes was 10% [11].
Harada et al (2008) studied the incidence of facial lymph nodes involvement in oral SCC. He studied a sample of 254 neck dissections. Regardless of the cervical lymph node status [6]. He had positive parotid lymph nodes in 10% of cases when the primary lesions were in the buccal mucosa, lower alveolar margin, and tongue. He recommended the resection of the parotid gland tail enblock with the extraglandular and intraglandular parotid lymph nodes as a routine practice during neck dissection for the management of primary oral SCC of the above-mentioned sites [6,12].
The findings that the possibility of metastases in SFLN is relatively high when the primary sites are in the lower alveolar margin, the buccal mucosa, and the lips is explained by the close anatomical proximity of SFLN to these sites and because of the large number of lymph routes that end at the SFLN region.
Pan et al studied 18 cadaveric halves of the superficial tissues of the head and neck to detect their lymphatic vessels. They produced a map of the head and neck lymphatics to help management of trauma and malignancies in this region. They found that the SFLN drain the buccinator lymph nodes that drain the buccal mucosa. In our study we found a trend towards positivity of the SFLN with higher T stage and less differentiated tumors. This adds more caution so as not to miss these nodes when advanced stages and grades are shown in the primary tumors. This agrees with Pestinis et al, who found that SFLN are usually affected in advanced stages [10].
The main obstacle that makes surgeons hesitate to go above the inferior border of the mandible is the fear of damage of the marginal mandibular nerve that results in various functional problems that can impacts the patient’s quality of life. This should not hinder proper evaluation of the facial lymph nodes in cases at risk of metastases. Careful dissection in the current series yielded 76.7% success rate in handling the marginal mandibular nerve. This should encourage using this technique to avoid the high possibility of nodal involvement that surely out weight the relatively minor risk of nerve affection. Temporary paralysis of the marginal mandibular nerve is usually related to stretch injury from retraction or operative manipulation.
Irrespective of the site of skin incision, skin flaps should be carefully elevated in a plane immediately deep to the platysma muscle (subplatysmal plane), and superficial to the investing layer of the deep cervical fascia. It is not the level of the skin incision that is important, but it is the level of transection of the investing layer of the investing cervical fascia.
Hussein G, Manketlew RT 2004 reported that the distance between the lower border of the mandible and the marginal mandibular nerve varies significantly. The nerve may be above the lower border by up to 1.3 cms or below the lower border by 1.7cm [13].
The position of the patient’s head is an important factor to consider during marking of skin incisions in the submandibular region. The neck should always be extended by placing a roll under the shoulders to maintain the extended position. The head is placed where the mandible is placed in the most perpendicular position to the patient’s coronal plane. Hyperextension of the neck carries the nerve more anterior and downward [14].
Conclusion
We conclude that SFLN is a probable site of lymph node metastases in SCC of the lower alveolar margin and buccal mucosa, in addition to the SCC of the lip. This probability increases with the advancement of the tumor and the tumor grade. Careful dissection above the inferior border of the mandible can safely remove these SFLN without significant injury to the marginal mandibular branch of the facial nerve.
Funding
None.
Competing interests
None declared.
Ethical approval
This clinical study had approval.
Patient consent
All patients had consent.
Moulding FJ, Roach SC, Carrington BM (2004) Unusual sites of lymph node metastases and pitfalls in their detection. Clinical Radiol 59: 558- 72. [ Ref ]
Shehan P, Colreavy M, Toner M, Timon CV (2004) Facial node involvement in head and neck cancer. J head neck 26: 531-536. [ Ref ]
Di Nardo LJ (1997) Lymphatics of the submandibular space: an anatomic, clinical, and pathologic study with applications to floor of mouth carcinoma. Thesis, Laryngoscope. [ Ref ]
Chang VF and Fan YF (2000) Facial lymphadenopathy in nasoparyngeal carcinoma. Clinical Radiol 55: 3637. [ Ref ]
Robbins KT, Medina JE, Wolf GT, Wolfe GT, Levine PA, et al. (1991) Standardizing neck dissection terminology. Official report of the Academy’s Committee for head and neck surgery and oncology. Arch Otolaryngol Head Neck Surg 117: 601-605. [ Ref ]
Sivindian R, Kaplam MJ, Lee K, Lebl D, Pinot H, et al. (2000) Long term result of 100 consecutive neck dissection and their implication. Arch Otolaryng Head and Neck Surg 130: 1369-1373. [ Ref ]
Dezinis L, Bolzoni A, Piazza C, Nicolai P (2006) Prevalence and localization of nodal metastases in squamous cell carcinoma of the oral cavity: role and extension of neck dissection. Eur Arch Otorhinolaryngol 263: 1131-1135. [ Ref ]
Hohlweg-Majert B, Metzger MC, Voss PJ, Hölzle F, Wolff KD (2009) Preoperative cervical lymph node size evaluation in patients with malignant head/neck tumors: comparison between ultrasound and computer tomography. J Cancer Res Clin Oncol 135: 753-759. [ Ref ]
Maruyama S (1998) Marginal branch of the facial nerve in submandibular dissection for T2 lingual carcinomas.Nippon Jibiinkoka Gakkai Kaiho 101: 1436-1441. [ Ref ]
Petsinis V, Papadogeorgakis N, Evangelou I, Goutzanis L, Pandelidaki E, et al. (2009) Metastasis to supramandibular facial lymph nodes in patients with squamous cell carcinoma of the oral cavity. J Oral Maxillofac Surg 67: 1401-1408. [ Ref ]
Barry CP, Wong D, Clark JR, Shaw RJ, Gupta R, et al. (1991) Postoperative radiotherapy for patients with oral squamous cell carcinoma with intermediate risk of recurrence. A case matches study. Head Neck 39: 1399-1404. [ Ref ]
Okura M, Kagamiuchi H, Tominaga G, Iida S, Fukuda Y, et al. (2005) Morphological changes of regional lymph node in squamous cell carcinoma of the oral cavity. J Oral Pathol Med 34:214–219. [ Ref ]
Nason RW, Binahmed A, Torchia MG, Thliversis J (2007) Clinical observations of the anatomy and function of the marginal mandibular nerve. Int J Oral Maxillofac Surg 36: 712–715. [ Ref ]
Potgieter W, Meiring JH, Boon JM, Pretorius E, Pretorius JP, et al. (2005) Mandibular landmarks as an aid in minimizing injury to the marginal mandibular branch: a metric and geometric anatomical study. Clin Anat 18: 171-178. [ Ref ]