Journal Name: Journal of Clinical Case Reports and Trials
Article Type: Research
Received date: 26 November, 2019
Accepted date: 13 December, 2019
Published date: 16 December, 2019
Citation: Guo Q, Liu D, Li L, Liu H, Qiao P, et al (2019) Morphological Changes of Pharyngeal Airway After Incisor Retraction in Bimaxillary Protrusion Growing Patients with Maximum Anchorage. J Clin Case Rep Trials. Vol: 2, Issu: 2 (35-40).
Copyright: © 2019 Guo Q, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Objective: To evaluate the changes of morphology in the pharyngeal airway after incisor retraction in bimaxillary protrusion growing patients with maximum anchorage by three-dimensional (3D) registration and evaluation.
Study Design: Cone beam computed tomography (CBCT) scans of 32 growing patients with bimaxillary protrusion and 32 age- and gendermatched controls were reconstructed. A student t-test was used to compare morphological changes of pharyngeal airway between two groups.
Result: After treatment, both groups showed a general enlargement in pharyngeal airway dimensions. There showed no statistical differences in the change of pharyngeal volume, CSA, LAT/AP and GH between the two groups. However, the experiments showed a significant decrease in the ration of palatopharynx area (PPA) to glossopharynx area (GPA) compared with the control group. A significant correlation was observed among the PPA/GPA, the incisor retraction amount and the hyoid backward amount.
Conclusion: Growing bimaxillary protrusion patients with maximum anchorage showed a potential trend of slower growing speed of palatopharynx than glossopharynx, which may be caused by the backward of the hyoid and retraction of the central incisor.
Keywords
Pharyngeal airway; CBCT; 3D registration; Bimaxillary protrusion.
Abstract
Objective: To evaluate the changes of morphology in the pharyngeal airway after incisor retraction in bimaxillary protrusion growing patients with maximum anchorage by three-dimensional (3D) registration and evaluation.
Study Design: Cone beam computed tomography (CBCT) scans of 32 growing patients with bimaxillary protrusion and 32 age- and gendermatched controls were reconstructed. A student t-test was used to compare morphological changes of pharyngeal airway between two groups.
Result: After treatment, both groups showed a general enlargement in pharyngeal airway dimensions. There showed no statistical differences in the change of pharyngeal volume, CSA, LAT/AP and GH between the two groups. However, the experiments showed a significant decrease in the ration of palatopharynx area (PPA) to glossopharynx area (GPA) compared with the control group. A significant correlation was observed among the PPA/GPA, the incisor retraction amount and the hyoid backward amount.
Conclusion: Growing bimaxillary protrusion patients with maximum anchorage showed a potential trend of slower growing speed of palatopharynx than glossopharynx, which may be caused by the backward of the hyoid and retraction of the central incisor.
Keywords
Pharyngeal airway; CBCT; 3D registration; Bimaxillary protrusion.
Introduction
Bimaxillary protrusion is a common condition characterized by prominent and proclined upper and lower incisors and a protruding profile [1]. In order to acquire a more aesthetics profile, those patients usually seek orthodontic care. And because patients want a straight profile, many orthodontists believe it is necessary to extract premolars, and to place miniscrews to retract incisor with maximum anchorage [2]. Though occlusal harmony and aesthetic appearance is the aim of orthodontic treatment, more attention is being paid to the shape of dentofacial complex, especially the pharyngeal airway. According to varies studies [3-6], the pharyngeal airway plays a key role in ventilation, swallowing, and pronunciation. More and more current researches in orthodontics have focused on the pharyngeal airway and its potential importance to modify the development of oral and maxillofacial (OMF) region [7,8]. Besides, these previous studies have shown that the airway is implicated in developing abnormally long vertical facial dimensions [9,10], and that the retrospective pharyngeal airway analysis needs to be established during incisor retraction [11]. Therefore, the detailed assessment of the pharyngeal airway is still an important basis of routine orthodontic diagnosis and planning [12].
Many studies have evaluated the effect of anterior teeth position on the pharyngeal airway morphology in Class I bimaxillary adult patients. Chen and Wang showed that the upper airway especially the oropharynx and hypopharynx became narrower after extraction of four premolars and retraction of the incisors [11,13]. On the contrary, Maaitah reckoned that incisor retraction with the first premolars extraction does not affect upper airway dimensions [14]. However, there have been no studies related to the functional response of the pharyngeal airflow followed by the morphological changes after incisors retraction. The upper airway morphology may have an effect on the pressure and flow rate of the pharyngeal airflow, which are important factors of pharyngeal ventilation function [15,16]. What’s more, mature airways are larger, longer, more elliptical and medio-laterally oriented, less uniform, and less compact, while individuals in growth period have their particular characteristics [17,18]. Therefore, evaluation of the individual changes of pharyngeal morphology and airflow during incisor retraction in growing bimaxillary protrusion patients need to be established.
As the inherent inaccuracies of two dimensional (2D) lateral cephalograms [19,20], three dimensional (3D) analysis was preferred in assessment of hard and soft tissue morphology [21-23].Compared with computed tomography (CT) imaging techniques, CBCT has been used to evaluate upper airway morphology with its ever wider adaptation, which is proven to provide sound and reproducible results [24-26]. 3D models can then be reconstructed based on the CBCT images. With the accurate registration method, pre- and post-treatment 3D models can be superimposed to examine the morphological changes [27].
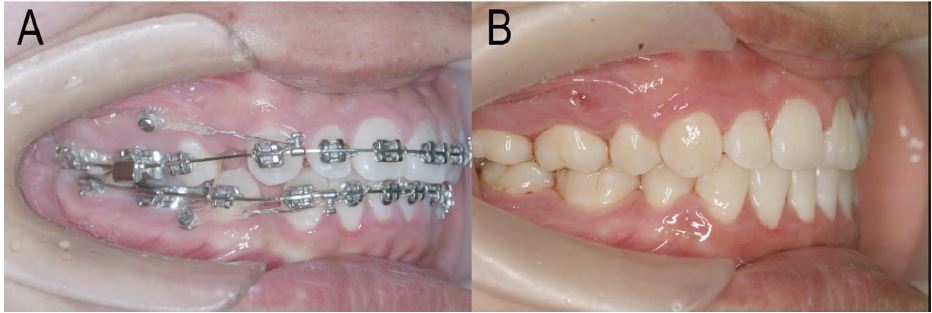
Figure 1:Miniscrews were placed in the interradicular locations between the first molar and second premolar at the attached gingival level height. Miniscrews of pre-treatment (figure A) and post-treatment (figure B) were shown.
The aim of this retrospective study was to clarify the change of pharyngeal airway during incisor retraction in growing bimaxillary protrusion patients with maximum anchorage by 3D registration and evaluation. The individual differences in pharyngeal airway between pre- and posttreatment were also evaluated.
Materials and Methods
Subjects
This research was approved by the Research Ethic Committee from the Stomatology School of Shandong University (Protocol number: GR201801). In this retrospective study, 32 individuals who met the four following criteria were randomly selected from Orthodontic Department of Shandong Stomatology Hospital between 2016 and 2018:
• Chinese growing patients (15 boys aged 10. 65±1.40 years and 17 girls aged 11. 14±1.47 years) with full dentition at initial (excluding the third molars).
• Informed consent including the possible damage of CBCT radiation lesion and miniscrew-methodologies was acquired.
• Pretreatment with Class I molar relationship, interincisal angle less than 124°, upper incisor protrusion more than 7.7 mm and lower incisor protrusion more than 3.0 mm.
• Patients who had medical history including craniofacial deformity, hypopharynx disease, sleep apnea syndrome, adenoidectomy and tonsillectomy were excluded.
• Four first premolars were extracted and four miniscrews (Cibei Medical Company, Ningbo, China. No. 121222) were placed as the anchorage for the translational retraction of the incisors. The patients were treated using oriental preadjusted appliance KOSAKA slot brackets (OPA-K, Tomy, Fukushimaken, Japan. No.936-102L 022), and force of 150g per side of elastic chains were applied from the miniscrew to the upper and lower crimpable hooks to retract the maxillary and mandibular teeth (Figure 1). 32 age- and gender- matched controls (15 boys aged 10.28±1.33 years and 17 girls aged 11. 32±1.51 years) who were treated with impacted teeth traction, but without other traditional orthodontic treatment were also selected randomly. All subjects were visited at 4-6 weeks intervals over a period of 10±3 months.
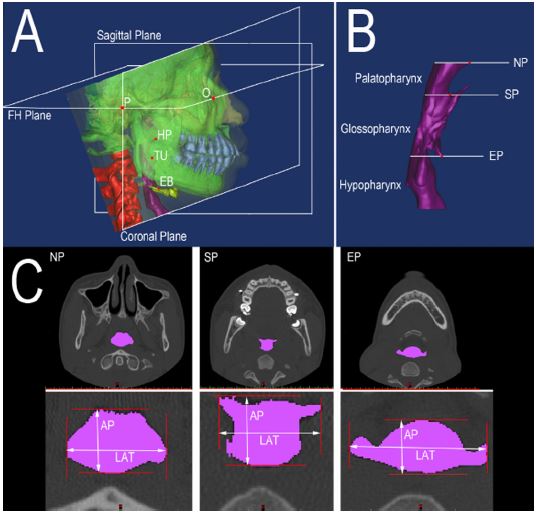
Figure 2:3D model of the upper airway was reconstructed. A: Definition of the spatial coordinate system. B. Region of pharyngeal airway. C. Axial crosses section of pharyngeal airway.
CBCT data acquirement
The whole skull CBCT scanning with 0.4 mm slices was performed in Week One after implanting all miniscrews (Time One: T1), and post-treatment (Time Two: T2) with natural head posture and maximum intercuspation during the awake periods of patients at the end of eupnoea respectively, which were undertaken in the same way by 3D eXam scanner (Kavo Dental GmbH, Bieberach, Germany. No. ICU081294) at a 0.30-voxel resolution. All patients were asked to maintain the resting position of the tongue tip, which was in contact with the anterior part of the hard palate without touching the anterior teeth. The CBCT scanning was performed perpendicularly to the apicalcoronal direction on each slice with the lateral scanogram of the head position (scan time: 8.9 seconds, 120 kV, 5 mA). The data were exported as Digital Imaging and Communications in Medicine (DICOM) format.
3D visual model reconstruction
All 3D models were constructed from CBCT images. The bone, teeth and pharyngeal airway morphology structures were respectively separated by threshold based on Hounsfield Unit (HU) in MIMICS 16.01 (Materialism’s Interactive Medical Image Control System) software. In order to include the alveolar regions and exclude tooth structure, a lower limit of 392 HU and a higher limit of 1900 HU were defined. The tooth excluding bone structure was separated with a lower limit of 1500 HU and a higher limit of 3725 HU, and the pharyngeal airway part was around -1024 HU to -259 HU. The separated and independent masks were created for each part, which generated following individual geometrical files and 3D models. All 3D masks were exported as Stereolithography (STL). To build 3D models of the pharyngeal airway before and after incisor retraction, T1 and T2 CBCT data were imported into MIMICS 16.01 software. Once segmented, all of the sections were also reconstructed respectively (Figure 2A).
Registration of pre- and post-treatment models
The investigator used landmark-derived superimposition method in order to make the surfaces of the two models approximate to each other as much as possible. Then, the investigator used ICP (Iterative closest point) algorithm based regional registration in Mimics with the craniobase as the reference [28]. After registration, we imported the saved mimics file into 3-matic Research 9.0 (Materialise, Leuven, Belgium). Accuracy and reproducibility of the superimpositions were assessed only in the crown portion of the model to measure RMS (Root mean square) value between the models [29,30]. A color scale image, a mean, and a standard deviation can be obtained. Then the RMS can be via this formula: √(x^(-2)+σ^2 ) , where x̅ is mean, and σ is the standard deviation. A registration with a RMS value ≤0.4 mm was considered successful, which is the size of the voxel generated by the CBCT machine.
Table 1:Descriptive statistics and comparison of pharyngeal airway between T1 and T2 in two groups (T1, pretreatment; and T2, post-treatment).
| Experiments (n=32) | Controls (n=32) | p | |||
|---|---|---|---|---|---|
| (T2-T1)/T1% (percentage) | |||||
| Mean | SD | Mean | SD | ||
| VOL | 26.85 | 19.42 | 28.13 | 13.97 | 0.098 |
| CSA | 7.41 | 2.62 | 7.65 | 2.83 | 0.076 |
| LAT/AP | 6.46 | 2.64 | 8.61 | 3.99 | 0.071 |
| GH | 3.76 | 1.05 | 3.54 | 1.13 | 0.423 |
| PPA/GPA | -18.09 | 2.14 | 9.23 | 5.77 | 0.001 |
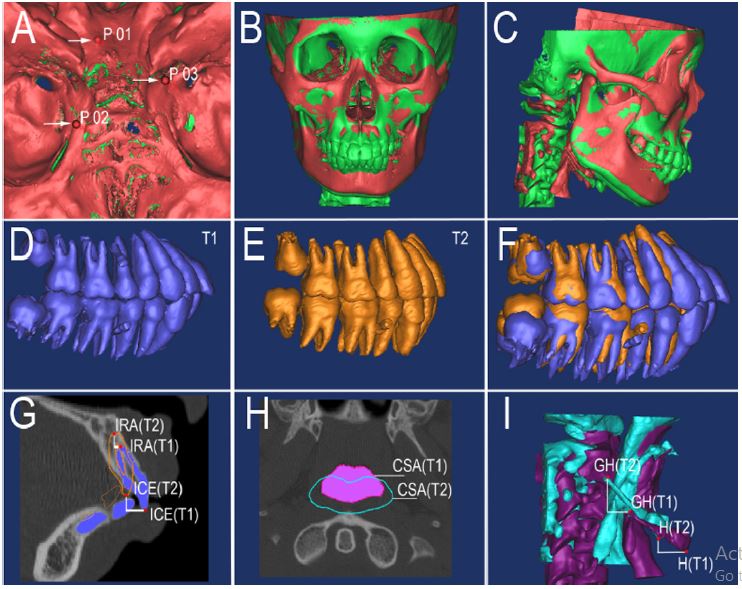
Figure 2:The pre- (T1) and post-treatment (T2) data of patients was registered. A: STL registration with cranial base. B-C: Registration of pre- (green) and post- (red) models. D-F: Pre- (purple) and post- (yellow) models of the teeth. G-I. Changes in the teeth, cross-sectional areas of the pharyngeal airway and displacements of the hyoid bone between the T1 and T2 models were measured.
3D Measurement
In this study, the palatopharynx was defined as the region between the hard palate and the end of the uvula; the glossopharynx lay between the end of the uvula and the epiglottis; and the hypopharynx was below the epiglottis (Figure 2B). The anterior boundary of the pharyngeal airway was defined by soft palate, base of the tongue, and the anterior wall of the pharynx [31,32]. Three crosssectional planes were used to evaluate the area of the airway and identify on the 3D model [18]. The area measurements included NP, SP, and EP area (Figure 2C). The landmarks, cross-sectional planes and pharyngeal airways identified on each 3D model were shown in Supplementary Table 1.
After 3D reconstruction, the pharyngeal volume (VOL) and cross-section area (CSA) were obtained. The ratio of lateral width (LAT) to anteroposterior width (AP), and palatopharynx area (PPA) to glossopharynx area (GPA) was computed in construction of cross-section. After registration and numerical simulation, the changes of pharyngeal morphology and flow field were obtained in 3D geometric models for inter-patient comparison (Figure 3). The hyoid retraction in the horizontal (X-H) and vertical (Y-H) direction, and the central incisor retraction at edge (X-ICE) and root (X-IRA) in the horizontal direction, and the genial tubercle to hyoid distance (GH) were measured in 3D registration models. All parameters mentioned are defined in Supplementary Table 2 [33]. Every subject was measured for three times by the same investigator, and then the measurements were averaged.
Statistical Analysis
All collected data were organized, and descriptive statistics (means, standard deviations, and ranges for pre- (T1) and post-treatment (T2) records) were performed in SPSS software (version 22.0, SPSS Inc., Chicago, IL, USA). For each individual, variables of pharyngeal airway, hyoid and central incisor was described as (T2-T1)/T1% and differences between controls and experiments were assessed with t-tests. Relationships among variables were assessed by the Pearson correlation coefficient. The error of the method, which was based on double measurements at a 2-month interval, was calculated for 32 randomly selected patients for 3D linear measurements (as described by Houston [34]) and was calculated as follows: s=√Σ (d)2/2n (where ‘d’ indicates deviations between the two measurements and ‘n’ indicates the number of paired objects). The error for 3D linear and cross-sectional area measurement was 0.26 mm and 0.13 mm2 (SDs of d are 0.14 mm and 0.07 mm2), respectively [23]. The statistical difference was not significant between the two measurements by t-test at the significance level of α=0.05.
Table 2:Pearson Correlation Coefficient Analysis between Some Parameters (T1, pretreatment; and T2, post-treatment; n=32).
| Experiments | |||||
|---|---|---|---|---|---|
| (T2-T1)/T1% | LAT/AP | PPA/GPA | X-H | Y-H | |
| X-ICE | r | 0.44 | -0.827 | 0.803 | 0.337 |
| p | 0.088 | 0.048 | 0.001 | 0.156 | |
| X-IRA | r | 0.221 | -0.472 | 0.788 | 0.335 |
| p | 0.257 | 0.072 | 0.002 | 0.157 | |
| (T2-T1)/T1% | LAT/AP | PPA/GPA | X-ICE | X-IRA | |
| X-H | r | 0.241 | -0.854 | 0.803 | 0.788 |
| p | 0.238 | 0.043 | 0.001 | 0.002 | |
| Y-H | r | 0.34 | -0.349 | 0.337 | 0.335 |
| p | 0.153 | 0.146 | 0.156 | 0.157 |
Results
Descriptive statistics and comparison of pharyngeal airway between T1 and T2 in two groups is presented in Table 1. The amount of upper incisor retraction in the incisal edge and the apex were 7.52±1.72 mm and 2.75±1.46 mm respectively, and the position of the hyoid was backward by 2.47±0.67 mm and 8.08±2.69 mm in the horizontal and vertical direction, respectively. Both groups showed an increase in VOL, CSA, LAT/AP and GH. The ratio of PPA/GPA reduced significantly in the experiments, whereas raised obviously in the controls, with a statistical significance for this value. The change amount of pharyngeal VOL, CSA showed no statistical differences between two groups. A significant correlation was observed in central incisor retraction amount in edge, the hyoid backward amount in the horizontal direction and the change of PPA/GPA (0.8<|r|<1, p<0.05) (Table 2).
Discussion
In this study, we evaluated the pharyngeal morphology in growing bimaxillary protrusive patients after incisor retrusion with maximum anchorage via CBCT data. As patients involved in the research are in the growth period, the upper airway of both groups became larger, wider, and longer after treatment. The change amount of pharyngeal dimension after incisor retrusion showed no differences between two groups. However, the ratio of PPA/GPA in the experimental group is significantly decreased compared with the control group. Besides, a significant correlation is observed among the amount of teeth retraction, hyoid backward movement and PPA/GPA in the experimental group, indicating that the distal movement of incisor may lead to a relative constrict in palatopharynx.
The retraction movement of the front teeth group via maximum anchorage may pose a substantial effect on the various tissues, including the constrictive dental arch and the shrinking oral cavity. Meanwhile, from the structural point of view, the palatopharynx is defined as the region between the hard palate and the end of the uvula, which is in accordance with the position of dentition. When incisors were retracted by maximum anchorage in growing patients, the palatopharynx region was expected to change less when compared to the control group. In addition, pharyngeal airway is an irregular soft tissue lumen and bone scaffold [35], the main reason of the decrease of PPA/GPA may be the slower growing speed of palatopharynx than glossopharynx, which is caused by the backward of the hyoid and retraction of the central incisor.
Large samples can figure out the potential trend of population, but were more difficult to collect. On the contrary, individual evaluation seems to be clearer to illustrate the personal changes, which is one of the innovative clinical significances of this research. However, the observation of long-term stability is still needed for each patient in future. According to the data in this study, we explored that orthodontists should not be only concerned with the dentofacial type, but the mechanobiological response of the pharyngeal airway.
Conclusion
The central incisor retraction with maximum anchorage may lead to a relative constrict in palatopharynx and thus a change in pharyngeal shape in growing bimaxillary protrusion patients.
Acknowledgement
We acknowledge all laboratory members for their contributions. This study was supported by grants from National Natural Science Foundation of China (nos. 11602122, 81571010 and 81771102).
Author Contributions
Hongchen Liu designed the research, reviewed and revised the manuscript and approved the final manuscript as submitted, and obtained funding for the project. Qingyuan Guo and Dongxu Liu collected the data, carried out the research, measured and analyzed the data. Liang Li analyzed and discussed the results, and drafted and revised the manuscript. Hong Liu and Pengyan Qiao collected the data, reviewed and revised the manuscript and approved the final manuscript as submitted. Rong Zhang collected the data, and carried out the research. Lingling E provided the CBCT scanning data. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Additional Information
Competing financial interests: The authors declare no competing financial interests.
Ramos CJ (2013) Treatment of dental and skeletal bimaxillary protrusion in patient with Angle Class I malocclusion. Dental Press J Orthod 18: 130-137. [ Ref ]
Solem RC, Marasco R, Guiterrez-Pulido L, Nielsen I, Kim S, et al., (2013) Three-dimensional soft-tissue and hard-tissue changes in the treatment of bimaxillary protrusion. Am J Orthod. Dentofac Orthop 144: 218-228. [ Ref ]
Wang W, Di C, Mona S, Wang L, Hans M (2018) Tongue Function: An Underrecognized Component in the Treatment of Obstructive Sleep Apnea with Mandibular Repositioning Appliance.Can Respir J 2018: 2157974. [ Ref ]
Chauhan A, Autar R, Pradhan KL, Yadav V (2015) Comparison of pharyngeal airway dimension, tongue and hyoid bone position based on ANB angle. Natl J Maxillofac Surg 6: 42-51. [ Ref ]
Chen X, Liu D, Liu J, Wu Z, Xie Y, et al. (2015) Three-Dimensional Evaluation of the Upper Airway Morphological Changes in Growing Patients with Skeletal Class III Malocclusion Treated by Protraction Headgear and Rapid Palatal Expansion: A Comparative Research. PLoS One 10: e0135273. [ Ref ]
Jose NP, Shetty S, Mogra S, Shetty VS, Rangarajan S, et al., (2014) Evaluation of hyoid bone position and its correlation with pharyngeal airway space in different types of skeletal malocclusion. Contemp Clin Dent 5: 187-189. [ Ref ]
Soni J, Shyagali TR, Bhayya DP, Shah R (2015) Evaluation of pharyngeal space in different combinations of class II skeletal malocclusion. Acta Inform Medica 23: 285-289. [ Ref ]
Li L, Liu H, Cheng H, Han Y, Wang C, et al., (2014) CBCT Evaluation of the upper airway morphological changes in growing patients of class ii division 1 malocclusion with mandibular retrusion using twin block appliance: A comparative research. PLoS One 9: 1-7. [ Ref ]
Wang T, Yang Z, Yang F, Zhang M, Zhao J, et al., (2014) A three dimensional study of upper airway in adult skeletal class II patients with different vertical growth patterns. PLoS One 9: 1-9. [ Ref ]
Jayaratne YSN, Zwahlen RA (2016) The oropharyngeal airway in young adults with skeletal class II and class III deformities: A 3-D morphometric analysis. PLoS One 11: 1-14. [ Ref ]
Chen Y, Liu H, Wang C, Zhang S, Cao C, et al., (2012) Effect of large incisor retraction on upper airway morphology in adult bimaxillary protrusion patients: Three-dimensional multislice computed tomography registration evaluation. Angle Orthod 82: 964-970. [ Ref ]
Sharma, K, Shrivastav S, Hotwani K, Murrell MD (2014) Orthodontic airway imaging: the cutting edge in treatment planning. Gen Dent 62: 54-59. [ Ref ]
Wang Q, Jia P, Anderson NK, Wang L, Lin J (2012) Changes of pharyngeal airway size and hyoid bone position following orthodontic treatment of Class i bimaxillary protrusion. Angle Orthod 82: 115-121. [ Ref ]
Al Maaitah E, El Said N, Abu Alhaija ES (2012) First premolar extraction effects on upper airway dimension in bimaxillary proclination patients. Angle Orthod 82: 853-859. [ Ref ]
Zhao M, Barber T, Cistulli PA, Sutherland K, Rosengarten G (2013) Simulation of upper airway occlusion without and with mandibular advancement in obstructive sleep apnea using fluid-structure interaction. J Biomech 46: 2586-2592. [ Ref ]
Van Holsbeke C, De Backer J, Vos W, Verdonck P, Van Ransbeeck P, et al., (2011) Anatomical and functional changes of the upper airway of sleep apnea patients due to mandibular repositioning - a large scale study. J Biomech 44: 442-449. [ Ref ]
Silvestrini-Biavati A, Capurro C, Ugolini A, Butti AC, Salvato A (2013) Possible causal relationships between competitive swimming in growing age and three-dimensional dentoalveolar development. Prog Orthod 14: 17. [ Ref ]
Abramson Z, Susarla S, Troulis M, Kaban L (2009) Age-related changes of the upper airway assessed by 3-dimensional computed tomography. J Craniofac Surg 1: 657-663. [ Ref ]
Bronoosh P, Khojastepour L (2015) Analysis of Pharyngeal Airway Using Lateral Cephalogram vs CBCT Images: A Cross-sectional Retrospective Study. Open Dent J 9: 263-266. [ Ref ]
Jakobsone G, Neimane L, Krumina G (2010) Two- and three-dimensional evaluation of the upper airway after bimaxillary correction of Class III malocclusion. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 110: 234-242. [ Ref ]
Gurani SF, Di Carlo G, Cattaneo PM, Thorn JJ, Pinholt EM (2016) Effect of Head and Tongue Posture on the Pharyngeal Airway Dimensions and Morphology in Three-Dimensional Imaging: a Systematic Review. J oral Maxillofac Res 7: 1-12. [ Ref ]
Alsufyani NA, Flores-Mir C, Major PW (2012) Three-dimensional segmentation of the upper airway using cone beam CT: A systematic review. Dentomaxillofacial Radiol 41: 276-284. [ Ref ]
Guo Q, Zhang S, Liu H, Wang C, Wei F, et al. (2011) Three-dimensional evaluation of upper anterior alveolar bone dehiscence after incisor retraction and intrusion in adult patients with bimaxillary protrusion malocclusion. J Zhejiang Univ Sci B 12: 990-997. [ Ref ]
De Oliveira Ruellas AC, Huanca Ghislanzoni LT, Gomes MR, Danesi C, Lione R, et al. (2016) Comparison and reproducibility of 2 regions of reference for maxillary regional registration with cone-beam computed tomography. Am J Orthod Dentofac Orthop 149: 533-542. [ Ref ]
Lin CC, Chen CC, Chen YJ, Lu TW, Hong SW (2014) A Dental Implant– Based Registration Method for Measuring Mandibular Kinematics Using Cone Beam Computed Tomography–Based Fluoroscopy. Int J Oral Maxillofac Implants 29: 798-806. [ Ref ]
Pauwels R, Araki K, Siewerdsen JH, Thongvigitmanee SS (2015) Technical aspects of dental CBCT: state of the art. Dentomaxillofac Radiol 44: 20140224. [ Ref ]
Haidekker MA (2014) Building a 3D computed tomography scanner from surplus parts. Biomed Instrum Technol 48: 142-151. [ Ref ]
Nanda V, Gutman B, Bar E, Alghamdi S, Tetradis S, et al., (2015) Quantitative analysis of 3-dimensional facial soft tissue photographic images: technical methods and clinical application. Prog Orthod 16: 21. [ Ref ]
Sun L, Hwang HS, Lee KM (2018) Registration area and accuracy when integrating laser-scanned and maxillofacial cone-beam computed tomography images.Am J Orthod Dentofacial Orthop 153: 355-361. [ Ref ]
Lee RJ, Weissheimer A, Pham J, Go L, de Menezes LM, et al., (2015) Three-dimensional monitoring of root movement during orthodontic treatment. Am J Orthod Dentofac Orthop 147: 132-142. [ Ref ]
Miyawaki S, Tawhai MH, Hoffman EA, Lin CL (2012) Effect of carrier gas properties on aerosol distribution in a CT-based human airway numerical model. Ann Biomed Eng 40: 1495-1507. [ Ref ]
He J, Wang Y, Hu H, Liao Q, Zhang W, et al. (2017) Impact on the upper airway space of different types of orthognathic surgery for the correction of skeletal class III malocclusion: A systematic review and meta-analysis. Int J Surg 38: 31-40. [ Ref ]
Kim HY., Min JY, Cho DY, Chung SK, Dhong HJ (2007) Influence of upper airway narrowing on the effective continuous positive airway pressure level. Laryngoscope 117: 82-85. [ Ref ]
Houston WJB (1983) The analysis of errors in orthodontic measurements. Am J Orthod 83: 382-390. [ Ref ]
Lopatienė K, Šidlauskas A, Vasiliauskas A, Čečytė L, Švalkauskienė V, et al. (2016) Relationship between malocclusion, soft tissue profile, and pharyngeal airways A cephalometric study. Medicina (Kaunas) 52: 307-314. [ Ref ]