Journal Name: Journal of Clinical Case Reports and Trials
Article Type: Case Report
Received date: 30 December, 2019
Accepted date: 24 January, 2020
Published date: 28 January, 2020
Citation: Lazzari O, Napoli M, Lefons ML, Strazzeri V, Cannata S, et al (2020) Percutaneous Endovascular Treatment of one Pseudoaneurysm of an AVF: Description of a Clinical Case. J Clin Case Rep Trials. Vol: 3, Issu: 1 (04-09).
Copyright: © 2020 Lazzari O, et al. This is an openaccess article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Arteriovenous fistula’s pseudoaneurysm percutaneous treatment: a case report
Pseudoaneurysm is a frequent complication of vascular accesses. The following case report highlights diagnosis and treatment of left distal artero-venous fistula pseudoaneurysm, located 3-4 cm above the anastomosis of the efferent vein. Pseudoaneurysm exerted a compressive effect on the mood with consequent blood flow reduction during hemodialysis sessions. Doppler ultrasound evaluation showed a reduction in blood flow rate calculated at the brachial artery level (2-3 cm from the elbow). Pseudoaneurysm was treated in the angiography room through percutaneous endovascular technique (PTA) and the interposition of a covered stent to exclude it. The angiography showed a pre-anastomotic stenosis of the radial artery that had not been detected by ECD; an angioplasty was performed. After the procedure, the angiographic examination of the AVF showed a complete perfusion, while Doppler ultrasound confirmed an adequate blood flow for the hemodialysis session.
Keywords
Angiography, Angioplasty, Pseudoaneurysm
Abstract
Arteriovenous fistula’s pseudoaneurysm percutaneous treatment: a case report
Pseudoaneurysm is a frequent complication of vascular accesses. The following case report highlights diagnosis and treatment of left distal artero-venous fistula pseudoaneurysm, located 3-4 cm above the anastomosis of the efferent vein. Pseudoaneurysm exerted a compressive effect on the mood with consequent blood flow reduction during hemodialysis sessions. Doppler ultrasound evaluation showed a reduction in blood flow rate calculated at the brachial artery level (2-3 cm from the elbow). Pseudoaneurysm was treated in the angiography room through percutaneous endovascular technique (PTA) and the interposition of a covered stent to exclude it. The angiography showed a pre-anastomotic stenosis of the radial artery that had not been detected by ECD; an angioplasty was performed. After the procedure, the angiographic examination of the AVF showed a complete perfusion, while Doppler ultrasound confirmed an adequate blood flow for the hemodialysis session.
Keywords
Angiography, Angioplasty, Pseudoaneurysm
Introduction
Pseudoaneurysm represents a not uncommon complication in the pathology of vascular access for hemodialysis. It is formed by a cavity external to the vessel lumen, without its own wall [1-2], which, on clinical objective examination, looks like a pulsating mass. Its genesis is linked most of the time to inadequate venipuncture / tamponade of the FAV puncture site, with consequent extravasation and formation of a hematoma that sees its feeding through a continuous solution (defined collar) that maintains communication between vessel and cavity itself.
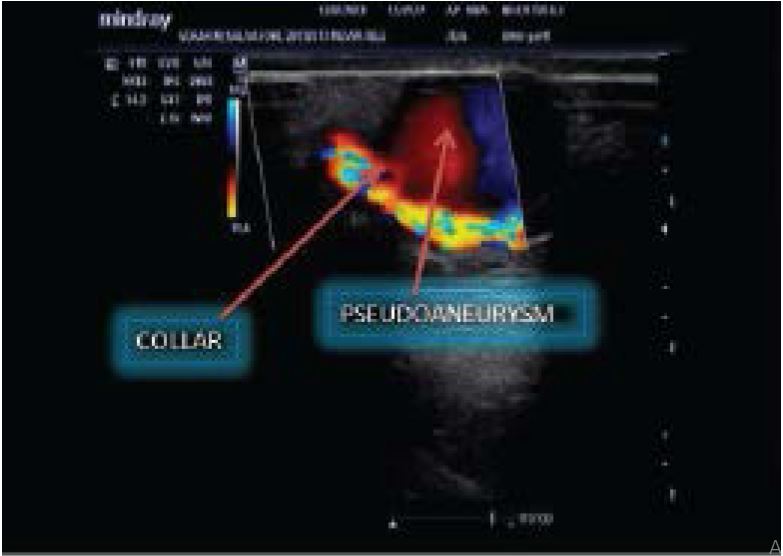
In B-Mode ultrasound the pseudoaneurysm appears as a cavity with anechoic content, with turbulent flow inside. At the eco-color-Doppler (ECD), a turbulent and swirling flow can be observed, with intense aliasing that increases at the collar (Figure 1). Surgery is the treatment of choice for vascular access pseudoaneurysms by hemodialysis, especially if the pseudoaneurysm becomes complicated by infection or thrombosis or if there is a possible risk of rupture [3-5]. Alternative treatments are recently emerging through the use of endovascular percutaneous techniques [6] with which covered stents are used that exclude vascular injury [7-11].
Figure 1:Color-Doppler image of a pseudoaneurysm
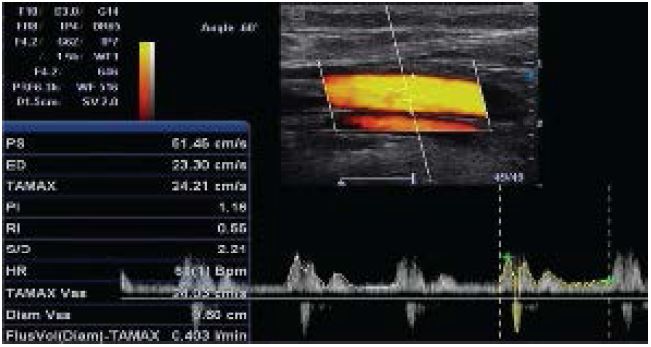
Figure 2:Brachial artery Doppler tracing with diastolic incisions with a flow rate of 403 ml / m and IR 0.55
Figure 3:Skin mapping of the Pseudoaneurysm
Figure 4:Pseudoaneurysm and stenotic cephalic vein
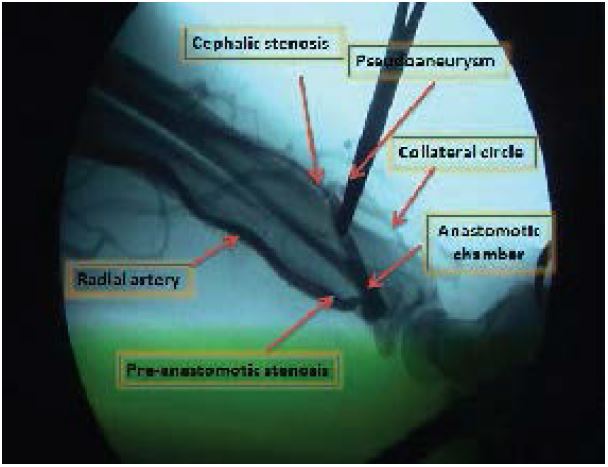
Figure 5a:Angiography of the FAV
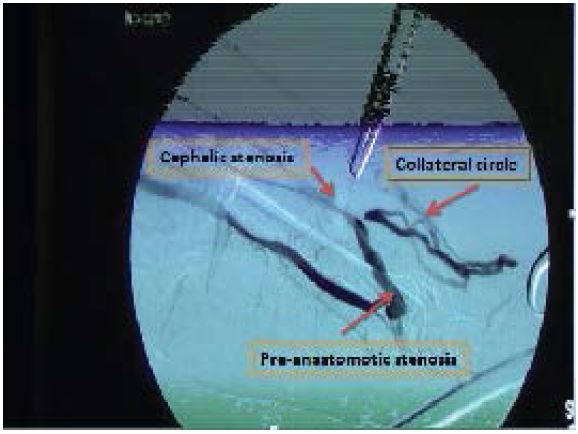
Figure 5b:Subtraction FAV angiography
Figure 6:Intrastent angioplasty performed with a 6 mm balloon. At 15 atm
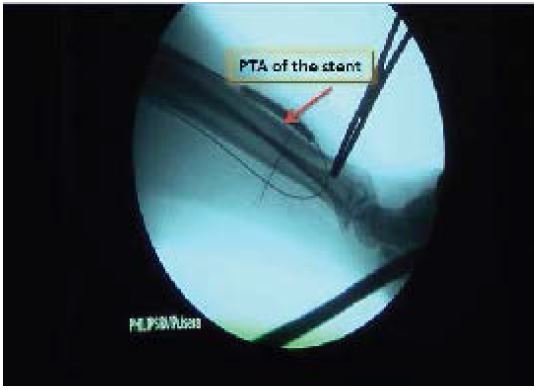
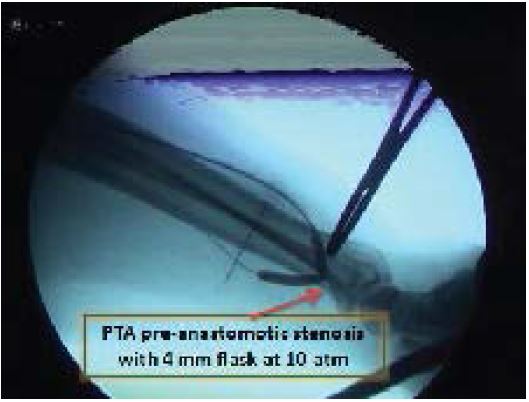
Figure 7a:PTA pre-anastomotic radial artery, anastomotic chamber and first tract of the cephalic with balloon from 4 mm to 10 atm
Figure 7b:Final angiography showing the good channeling of the AVF; the flow is so fast that the opacification is not very evident. The collateral circles seen previously are not found.
The reported case examined highlights how endovascular percutaneous treatments with stent placement under angiographic guidance can be used to close a pseudoaneurysm formed following puncture of the fistula not adequately buffered at the efferent artery of a FAV, which determined a stenosis of the vessel and a reduction in the flow of the arteriovenous fistula assessed by the eco-colordoppler. This situation compromised the patient’s dialysis effectiveness since the dialysis flows were insufficient.
Case report
64-year-old patient, with 2nd degree obesity and BPCO, chronic uremic from likely nephroangiosclerosis, carrier of mechanical mitral valve in oral anticoagulant treatment with INR maintained between 2 and 3. In December 2012 he is subjected to packaging of a left distal FAV, which appears to be working well. After about 40 days, once the FAV has matured, regular hemodialysis treatment begins with good blood flows.
After about 2 months, there is a reduction in dialysis blood flows and also the presence of an expansion at 3-4 cm from the anastomotic chamber. This dilatation also appeared after an ineffective attempt at venipuncture. For this reason, the patient undergoes an ECD study of the AVF: the flow rate of the AVF measured by calculating the flow of the brachial artery to the elbow [12,13] is 403 mL / m ‘(Figure 2), a clearly lower than the 950 mL / m ‘detected only 15 days before. The examination also shows a cephalic vein which, 3-4 cm from the anastomosis, appears to be compressed by a pulsating mass corresponding to the aneurysmal dilation observed objectively (Figure 3).
Then the ECD study allows to diagnose pseudoaneurysm of the cephalic vein, which exerts a compressive effect on the tract immediately downstream of the pseudoaneurysm collar, as shown in Figure 4.
PTA and stenting in the angiography room
The case study is completed with an angiographic examination that shows a stenosis 3-4 cm from the anastomotic chamber, a stenosis determined by the pseudoaneurysm, with the presence of numerous collaterals circles whose direction of blood flow is partly towards the hand and partly towards the elbow. Not documented in the previous ECD study, there is also a pre-anastomotic radial artery stenosis (Figure 5A, B). Later, as shown in the images shown here (Figure 6 and Figure 7), we proceed to percutaneous angioplasty (PTA) of the stenosis [14] and to place a covered stent at the level of the collar of the pseudoaneurysm that causes its exclusion from the flow (Figure 8) and to an angioplasty of the radial artery in the pre-anastomotic site (Figure 7). The angiographic control, performed after the procedure, documents the disappearance of the collateral circles previously highlighted and a good channeling of the FAV (Figure 7), while the ECD after PTA highlights a low resistance spectral tracing, with a good representation of the diastolic flow.
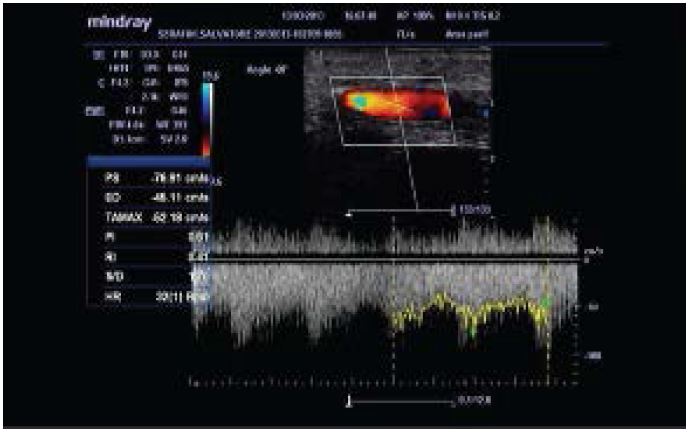
The flow rate measured in the brachial artery is 1000 mL / m ‘, with an IR of 0.4 (Figure 9). The patient is placed in a follow-up that foresees a quarterly ECD check in the first year and then every 6 months and, after an initial increase to 1300 mL / m ‘, the brachial artery flow rate has remained stable at 1000mL / m ‘with IR always stable between 0.4 and 0.42. No phenomenon of restenosis until the patient’s death from cardio-vascular complications, which occurred 2 years after the operation, with the FAV well-functioning.
Figure 8:Ultrasound image in post-procedure B-Mode
Figure 9:Eco-color-doppler plot was completely different from the pre-procedure. The flow rate had increased to 1000 ml / min and the IRs had decreased to 0.4
Discussion
The case described here suggests the following three main critical considerations:
• venipuncture was certainly the cause of the formation of the pseudoaneurysm, but the doubt remains that the stenosis, which we initially attributed to the compression of the pseudoaneurysm, was instead an organic stenosis responsible in turn for a hypertension of the flow, with consequent formation the pseudoaneurysm, which had not been adequately investigated at the ECD due to the artifacts present and produced by the same;
• it can be seen from Figure 7 B, the stent implanted to close the collar of the pseudoaneurysm also corrected the stenosis immediately downstream of the collar;
• the ECD study, probably excessively focused on the diagnosis of pseudoaneurysm, misses an important fact: the pre-anastomotic stenosis of the radial artery.
Therefore, this clinical case confirms how often the integration between ultrasonography and angioradiology is strongly necessary in the study of the pathology of the FAV for hemodialysis. It is proven experience that surgery with traditional surgery is the first choice in the treatment of pseudoaneurysms, especially when pseudoaneurysms are complicated by infections and / or thrombosis [3,5,7]. Although, endovascular percutaneous techniques are becoming increasingly popular as valid alternative techniques, thanks to the availability of devices such as cover-stents [3,4,6,13]. These do not aim to replace classical vascular surgery, which always remains the gold standard, but play an alternative role very useful in particular selected cases, thanks to the minimally invasive nature of the intervention they require and, last but not least, to the possibility that the FAV is left to be used quickly for hemodialysis treatment.
Disclosures
Financial support: No financial support was received for this submission.
Conflict of Interest: The authors have no conflict of interest.
Segoloni Gp, Mangiarotti G, Pacitti A (1998) La chirurgia degli accessi vascolari per emodialisi. In aspetti tecnici in Nefrologia. Genova: Forum Service ED 6: 92-93. [ Ref ]
Napoli M (2010) Eco-Color-Doppler & Accessi Vascolari per Emodialisi. Wichtig Editore3 :47-58. [ Ref ]
Anna Mudoni, Marina Cornacchiari, Maurizio Gallieni, Carlo Guastoni, Damian McGrogan,et al (2015) Aneurysms and pseudoaneurysms in dialysis access. Clin Kidney J 8: 363-367. [ Ref ]
Shah AS, Valdes J, Charlton-Ouw KM, Chen Z, Coogan SM, et al (2011) Endovascular treatment of haemodialysis access pseudoaneurysms. Society for Vascular Surgery 55: 1058-1062. [ Ref ]
Spergel Lm (2006) Treatment of AV Shunt Aneurysms// Pseudoaneurysms. Surgical Revision. J Vasc Access7: 212-213. [ Ref ]
Saad TF (2006) Treatment of AV Shunt Aneurysms/Pseudoaneurysms. Percutaneous Revision. J Vasc Access 7: 2013-2015. [ Ref ]
K. Gugliuzza (2006) Shunt Aneurysms/Pseudoaneurysms: etiology and when to treat. J Vasc Access 7: 210-211. [ Ref ]
Napoli M (2010) Eco-Color-Doppler & Accessi Vascolari per Emodialisi. Wichtig Editore 5: 92-96. [ Ref ]
Alexandra Guerra, Alain Raynaud, Bernard Beyssen, Jean‐Yves Pagny, Marc Sapoval, et al (2002) Arterial percutaneous angioplasty in upper limbs with vascular access devices for haemodialysis. Nephrol Dial Transplant 17: 843-851. [ Ref ]
Kim CY, Guevara CJ, Engstrom B, Gage SM, O’Brien PJ, et al (2012) Analysis of infection risk following covered stent esclusion of pseudoaneurysms in prothetic arteriovenous haemodialysis access grafts. J Vasc Interv Radiol 23: 69-74. [ Ref ]
Peden Ek (2011) Role of stent for treatment of failing haemodialysis accesses. Seminar Vasc Surg 24: 119-127. [ Ref ]
Lomonte C, Casucci F, Antonelli M, Giammaria B, Losurdo N et al (2005) Is there a place for duplex screening of the brachial artery in the maturation of arteriovenous fistulas? Semin Dial1 8: 243-246. [ Ref ]
Napoli M, Prudenzano R, Russo F, Antonaci AL, Aprile M, et al (2010) Juxta-Anastomotic Stenosis of Native Arteriovenous Fistulas: Surgical Treatment versus Percutaneous Transluminal Angioplasty. J Vasc Access 113: 346-351. [ Ref ]
M. Napoli, R Prudenzano, E Sozzo, D Mangione, V Martella, C (2012) Stenting in distal artero - venous fistolae Stenosis: preliminary reports. Giornale di Tecniche Nefrologiche e Dialitiche 24: 40-45. [ Ref ]