Journal Name: Journal of Clinical Case Reports and Trials
Article Type: Case Report
Received date: 06 January, 2020
Accepted date: 17 January, 2020
Published date: 05 February, 2020
Citation: Ghargozloo D, Paolo B, Maddalo M, Nadia P, Parafioriti A, et al (2020) Single Leg Muscle Metastases in Breast Cancer Patient: A Case Report. J Clin Case Rep Trials. Vol: 3, Issu: 1 (01-03).
Copyright: © 2020 Ghargozloo D, et al. This is an openaccess article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Introduction
Breast cancer is the first most prevalent cancer in women worldwide. Breast cancer generally metastasizes to bone, lung and liver but may involve other organs. Involvement of skeletal muscle is rare [1], but when it occurs, it usually presents with contiguous involvement of a soft tissue lesion and may appear clinically as a lump or mass. When skeletal muscle metastasis occurs, it is associated with a poor prognosis. We report a case of a breast cancer patient with single muscle metastases diagnosed using Magnetic Resonance Image (MRI) and 18Fluorine-2-fluoro-2-deoxy-dglucose- positron emission tomography (18F-FDG-PET) who is in stable disease six months during treatment.
Case Presentation
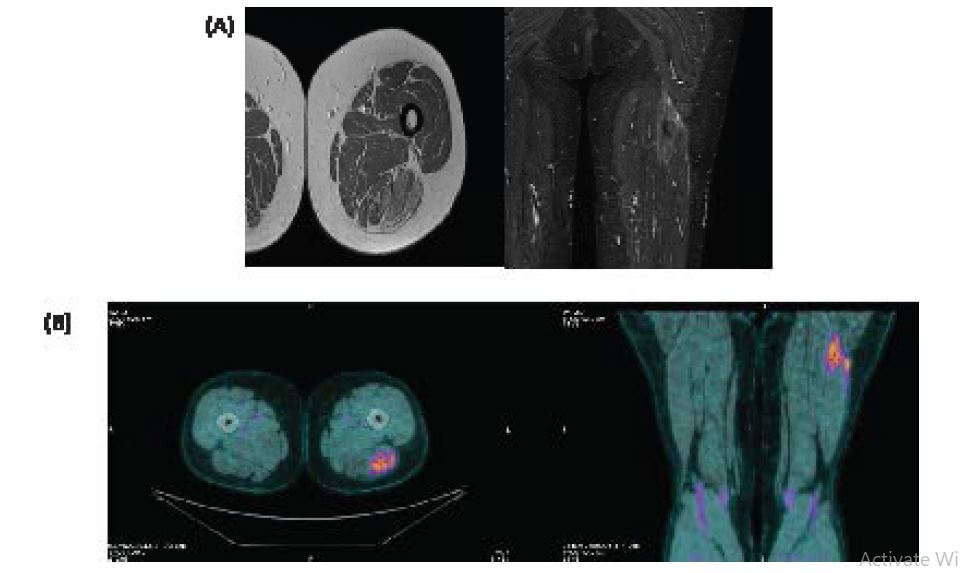
In June 2015, a 61-year-old woman was diagnosed with infiltrating left breast lobular carcinoma (mpT2N1aM0, G3 - ER 35% - PgR neg - cerb-B1 neg – MIB1 25%). She underwent a mastectomy of the left breast with omolateral axillary lymph nodes dissection. She received adjuvant chemotherapy (4 cycles of EC (epirubicin, cyclophosphamide) every 3 weeks plus 12 cycles of Taxol every week), followed by 2 years of endocrine therapy based on anastrozol. In October 2017, local relapse at the level of left axilla was diagnosed: surgery followed by radiotherapy of the left internal mammary nodes, omolateral axilla and supraclavicular lymph nodes was performed and ormonal therapy with Exemestane started. During surveillance, 1 years later (October 2018), the patient presented palpable left axillar nodule (second local relapse surgically removed) and no palpable mass but reported muscle pain in the posterior part of the left leg. A complete imaging assessment was then undertaken and included echography, MRI and 18F-FDG-PET (Figure 1).
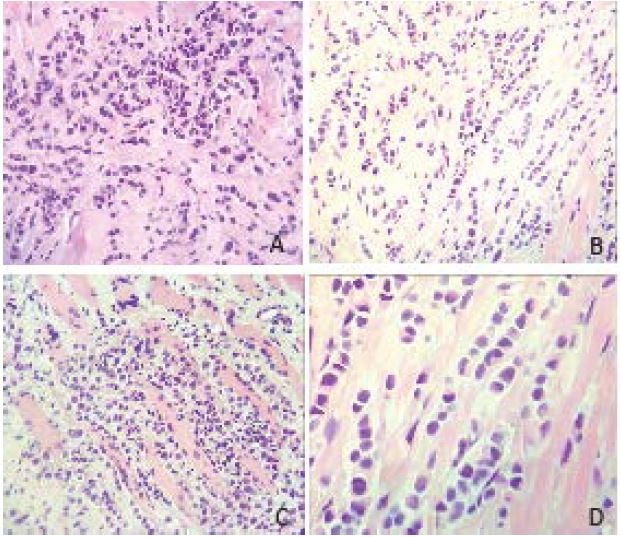
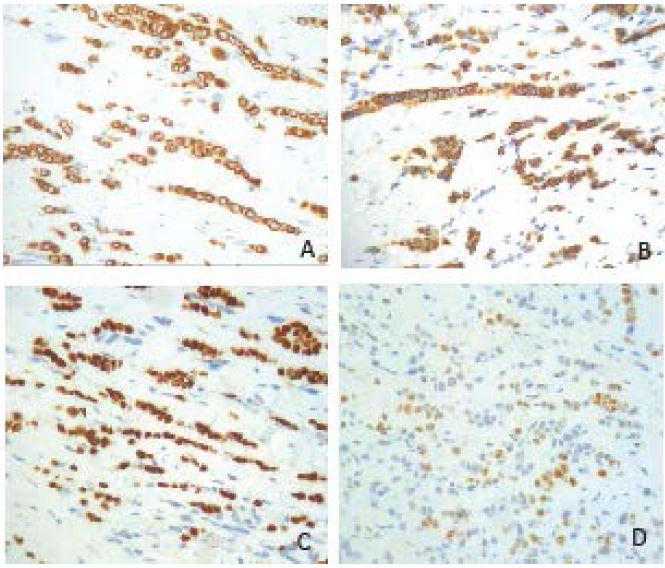
Tumour activity measured by 18F-FDG-PET revealed hypermetabolism in the left posterior part of the left leg (long head of the femoral biceps). Again, after needle cores biopsy, histological analysis was performed and revealed hormone receptors status similar to primary breast cancer (ER 40%, PR neg and HER2 neg, MIB1 30-40%) (Figure 2-3).
In January 2019, a systemic treatment associating Vinorelbine, Cyclophosphamide and Capecitabine was started. Nine month later, stable disease was observed at MRI. The treatment was well tolerated and the only side effect experienced by the patient was fatigue. Restaging with PET demonstrated that muscle metastasis was the only pathological active site, therefore lesion was surgically removed after 10 fractions radiotherapy (2.5 Gy/frac) to “sterilize” surgical bed. Patient have not leg impairment.
Figure 1:(A) Magnetic Resonance of the left leg, showing muscle tissue density lesions in long head of the femoral biceps. (B) F-18 fluorodeoxyglucose (FDG) positron emission tomography/computed tomography, showing femoral biceps muscle mass with increased FDG uptake.
Figure 2:Cores biospy show fibroous (A-B) and skeletal muscle (C) infiltrated by small/medium sized epithelioid neoplastic cells with cord and nest pattern of growth (H&E stain, A-B-C x20, D x40).
Discussion
Skeletal muscle metastases rarely occur in patients with breast cancer, likely due to a hostile microenvironment [2]. When skeletal muscle metastases do develop, they often present as isolated, painful soft tissue masses in the involved areas. Haematogenous spread is the most probable pathway suggested for the development of muscle metastases. Typically, these metastases are challenging to evaluate with MRI and/or FDG PET-CT and are often found to have round or oval shapes with well-defined margins [3-4]. Core needle biopsy is necessary to confirm the diagnosis. Differential diagnosis of muscle metastasis is of predominate importance because the treatment approach is pretty different [5]. Differentiation of these metastasis from myopathy, sarcoma, or intramuscular abscess is not easy [6] and misinterpretation due to the heterogeneity of clinical and radiological features, is not infrequent [7-8].
Figure 3:Tumor cells express cytokeratin EA1/AE3 (A), cytokeratin 7 (B), GATA3 (C), Oestrogen receptor (D); this immunophenotype indicates a metastatic carcinoma possibly of breast origin.
This case illustrates a presentation of metastatic breast cancer as single muscle metastasis on left posterior leg. Following patient treatment with chemotherapy, muscle nodule not regressed but a stable disease was achieved without new metastatic localisations and without leg impairment. A relatively low dose radiotherapy and subsequent surgery achieved complete disease response. The prognosis and appropriate treatment of skeletal muscle metastasis are unfortunatly uncertain [9-10]. Possible therapeutic options include radiotherapy and surgical excision. Surgical excision was recommended in selected patients such as those with a painful isolated mass and in patients with a good prognosis. Not very recent publications show than most of the patients die within few months despite the treatment [11]. We treated our patient with chemotherapy, radiotherapy and surgery and obtained a complete response of disease.
Funding
This research received no external funding.
Conflicts of interest
The authors declare no conflict of interest.
Young Woo Kim, Kyung Jin Seo, Su Lim Lee, Ki Wook Kwon, Joon Hur, et al.(2013) Skeletal Muscle Metastases from Breast Cancer: Two Case Reports. J Breast Cancer 16: 117-121. [ Ref ]
Surov A, Hainz M, Holzhausen HJ, Arnold D, Katzer M, et al. (2010) Skeletal muscle metastases: primary tumours, prevalence, and radiological features. Eur Radiol 20: 649-658. [ Ref ]
Alexey Surov, Johanne Köhler, Andreas Wienke, Hubert Gufler, Andreas Gunter Bach, et al.(2014) Muscle metastases: comparison of features in different primary tumours. Cancer Imaging 14: 21. [ Ref ]
Diana Bello-Roufai, Daniele G. Soares, Khaldoun Kerrou,Ahmed Khalil, et al. (2017) Long-term complete response in a breast cancer patient with skeletal muscle metastases diagnosed using 18F-FDG-PET.Oxf Med Case Reports 2017. [ Ref ]
Plaza JA, Perez-Montiel D, Mayerson J, Morrison C, Suster S, et al. (2008) Metastases to soft tissue: a review of 118 cases over a 30-year period. Cancer 112: 193-203. [ Ref ]
Salemis NS (2015) Skeletal muscle metastasis from breast cancer: management and literature review. Breast Dis 35: 37-40. [ Ref ]
Khandelwal AR, Takalkar AM, Lilien DL, Ravi A (2012) Skeletal muscle metastases on FDG PET/CT imaging. Clin Nucl Med 37: 575-579. [ Ref ]
Herring CL Jr, Harrelson JM, Scully SP (1998) Metastatic carcinoma to skeletal muscle. A report of 15 patients. Clin Orthop Relat Res 355: 272- 281. [ Ref ]
Almusarhed M, Eldeeb H (2017) Solitary biceps muscle metastasis from breast cancer. BMJ Case Rep 2017. [ Ref ]
Molina-Garrido MJ, Guillén-Ponce C (2011) Muscle metastasis of carcinoma. Clin Transl Oncol 13: 98-101. [ Ref ]
Mathis S, Fromont-Hankard G, du Boisguéheneuc F, Godenèche G, Mahieu F, et al. (2010) Muscular metastasis. Rev Neurol 166: 295-304. [ Ref ]