Journal Name: Journal of Clinical Research in Diabetes and Medicine
Article Type: Research
Received date: 30 May, 2019
Accepted date: 11 July, 2019
Published date: 26 July, 2019
Citation: Akkati RR, Bathula S (2019) Assessment of Psychological Manifestations and Prevalence of Diabetes Mellitus in Patients with Thyroid Dysfunction. J Clin Res Diabetes Med Vol: 1, Issu: 1 (01-06).
Copyright: © 2019 Akkati RR. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Diabetes mellitus and thyroid dysfunction are quite regularly associated. In diabetic patients the chronicity of thyroid dysfunction is two to three times greater than in patients with no diabetes mellitus, it increases with age and is significantly impacted by autoimmune diabetes and by female gender.
Material and Methods: Patients of all age groups who are known to have thyroid dysfunction were included in our study and also who are known to have thyroid dysfunction together with diabetes mellitus were included in our study.
Results: An entire of 291 cases were collected for assessment of psychological symptoms and a total of 62 cases were collected for determining the prevalence of diabetes mellitus in thyroid patients. Research work was accomplished in patients who encountered the inclusion criteria and found that the utmost frequent manifestations were uniform in patients with subclinical and undisguised thyroid disease and also identified that the prevalence of thyroid dysfunction in patients with diabetes mellitus was greater than the prevalence of diabetes mellitus in patients with thyroid dysfunction.
Conclusion: In conclusion, the levels of depression and stress were found to be little higher in case of hyperthyroidism patients when compared to hypothyroidism patients where the levels of anxiety were found to be almost similar in both cases. Instance of thyroid dysfunction in patients with diabetes mellitus was more than the occurrence of diabetes mellitus in patients with thyroid dysfunction.
Keywords:
Thyroid dysfunction, Anxiety, Depression, Stress and Diabetes mellitus.
Abstract
Diabetes mellitus and thyroid dysfunction are quite regularly associated. In diabetic patients the chronicity of thyroid dysfunction is two to three times greater than in patients with no diabetes mellitus, it increases with age and is significantly impacted by autoimmune diabetes and by female gender.
Material and Methods: Patients of all age groups who are known to have thyroid dysfunction were included in our study and also who are known to have thyroid dysfunction together with diabetes mellitus were included in our study.
Results: An entire of 291 cases were collected for assessment of psychological symptoms and a total of 62 cases were collected for determining the prevalence of diabetes mellitus in thyroid patients. Research work was accomplished in patients who encountered the inclusion criteria and found that the utmost frequent manifestations were uniform in patients with subclinical and undisguised thyroid disease and also identified that the prevalence of thyroid dysfunction in patients with diabetes mellitus was greater than the prevalence of diabetes mellitus in patients with thyroid dysfunction.
Conclusion: In conclusion, the levels of depression and stress were found to be little higher in case of hyperthyroidism patients when compared to hypothyroidism patients where the levels of anxiety were found to be almost similar in both cases. Instance of thyroid dysfunction in patients with diabetes mellitus was more than the occurrence of diabetes mellitus in patients with thyroid dysfunction.
Keywords:
Thyroid dysfunction, Anxiety, Depression, Stress and Diabetes mellitus.
Introduction
Iodide uptake into the thyroid, oxidation of iodide, iodination and coupling of tyrosyl residues together with cellular uptake, proteolysis of thyroglobulin are the steps involved in synthesis and storage of thyroid hormones whereupon followed by their secretion [1]. Sulfhydryl groups are required for peripheral transformation of T4 to T3 [2]. L-type amino acid transporters and organic anion transporters are involved in uptake and transport of thyroid hormones [3]. The receptors of thyroid hormones belong to nuclear receptor super family that functions by regulating transcription [4]. The principal regulator of serum TSH levels at pituitary is thyroid hormone negative feedback [5]. T4 and T3 play a vital role during pregnancy, neural ballooning and demarcation [6]. The major physiologic effect of these hormones is that they stimulate the metabolism as well as metabolic rate of lipids, proteins and carbohydrates [7]. Mental symptoms like anxiety and depression gets developed in many patients with thyroid dysfunction. Psychiatric symptoms are mainly due to adrenergic hyperactivity and in vulnerable patients these may be due to thyroid autoimmunity process itself [8]. High rate of depression has been observed in patients with primary thyroid disease [9]. Typical elevated cortisol levels and impaired dexamethasone suppression are because of a functional disconnection of the hypothalamus with impairment of inhibitory glucocorticoid feedback pathway from the hippocampus to the hypothalamus [10]. Thyroid function gets dismal in stressful conditions. Thyroid-stimulating hormone secretion is inhibited by stress by the action of glucocorticoids on central nervous system [11]. So there is a need to remark the changes in these variables. Untreated thyroid disorders influence the control of diabetes in many patients [12, 13]. The most likely mechanism that paramount to T2DM in thyroid dysfunction could be ascribed to perturbed genetic expression of redundancy of genes along with physiological deformity leading to plunged glucose usage and jettisoning in muscles, deluge of hepatic glucose output and boomed absorption of splanchnic glucose. These factors lead to insulin resistance. Insulin resistance is also kindred with thyroid dysfunction. Hypothyroidism and hyperthyroidism have been correlated with insulin intransigence which has been appeared to be the crucial cause of impeded glucose metabolism in T2DM [14]. The pathophysiological mechanisms shrouding this linked regulation are increasingly being untangled. They are epitomized in the proclamation of 5’ Adenosine Monophosphate-Activated Protein Kinase (AMPK), a central target not only for the intonation of insulin sensitivity but also for the evaluation of thyroid hormones on appetite and energy disbursement [15]. Subclinical hypothyroidism is linked with an enhanced risk of symptomatic hypoglycaemia [16]. There is a compelling confirmation from independent research that T3 directly elevates islet β-cell mass via thyroid hormone receptor α-dependent pathways [17]. Furthermore, insulin emanation from β-cells is likely controlled by the curtailed mitochondrial T3 receptor p43 [18]. These changes have been kindred with a decline in specific glucose transporters, namely GLUT2 and Kir6.2 and may thus be more broadly conciliated by the control of intracellular glucose availability which may have indications for other actions of T3 [19]. FT3 assists expression of important proteins involved in both glucose and lipid metabolism that may impact insulin secretion [20]. Declined FT3 and FT3/FT4 ratios and elevated FT4 levels were independently related to the prevalence of T2DM among the adult population [21]. Autoimmune thyroid disorders frequently exist in children and adolescents with type 1 diabetes mellitus. The generality of these disorders was 17.6% and of those, the most common was chronic autoimmune thyroiditis. Microsomal auto antibodies are more accurately interconnected with the presence of chronic autoimmune thyroiditis when compared to thyroglobulin auto antibodies. The largest prevalent immunological mechanisms influencing diabetic patients were autoimmune thyroid disorders. The thyroid status of many patients with positive markers was subclinical hyperthyroidism (3%), overt hyperthyroidism (6%), subclinical hypothyroidism (11%), overt hypothyroidism (3%) and euthyroidism (77%). No strong amalgamations of thyroid autoimmunity and other auto immunological disorders like celiac disease or existence of other autoimmune antibodies were identified [22]. The residence of inhibitor of extra thyroidal conversion of thyroxine (T4) to triiodothyronine (T3), dysfunction of the hypothalamo-hypophysial-thyroid axis and the existence of thyroid hormone binding inhibitor are contemplated to be tangled in abnormal thyroid function in patients with diabetes mellitus [23].So, there is a necessity to remark the association between diabetes mellitus and thyroid dysfunction.
Material and Methods
The research work was overseen in patients addressing the outpatient department of endocrinology. A total of 238 subjects for assessment of psychiatric symptoms and 45 subjects to determine the prevalence of diabetes mellitus in thyroid patients were encompassed in the study. Patients with different semblance of thyroid dysfunction who were determined by an endocrinologist were grouped as overt hypothyroidism (n=20(male=03; female=17)), subclinical hypothyroidism (n=190(male=07; female=183)), overt hyperthyroidism (n=22(male=01; female=21)) and subclinical hyperthyroidism (n=06(male=0; female=06)). IHEC approval was obtained after submission of protocol and IHEC No. is MGM/VCOP/PHARMD/017/2018. Patients were explained about the study and informed consent forms were seeked by explaining them in their local language. The study period is 6 months.
Inclusion criteria: Males and females of all age groups diagnosed to have thyroid dysfunction and thyroid dysfunction together with diabetes mellitus were included in our study.
Exclusion criteria: Pregnant women and patients who are already known cases of anxiety and depression were excluded.
Study design: It is a prospective, observational study conducted in outpatient department of endocrinology at Samraksha Diabetes, Thyroid and Endocrine Superspeciality Hospital and Research Centre, Warangal.
Clinical response assessment: The levels of anxiety and depression were assessed by Hamilton Rating Scale and stress was assessed by Perceived Stress Scale. Patients with parameters of metabolic control such as HbA1C ˃6%, high fasting and post lunch blood glucose levels, TSH ˃4.2OμUI/L, FT4˂0.9ng/dl (in case of hypothyroidism) and TSH ˂0.27μUI/L, FT4˃1.7ng/dl(in case of hyperthyroidism) were contemplated. Autoimmunity was undaunted where anti-TPO levels were higher than 34 IU/ml.
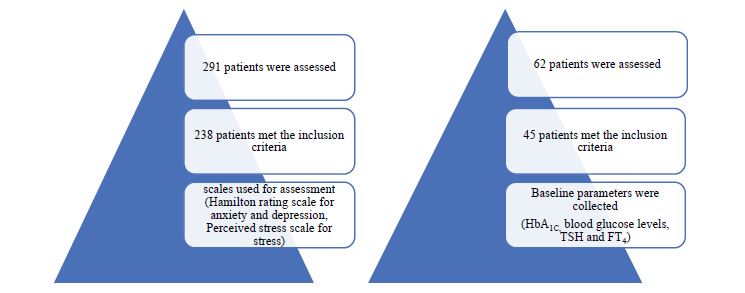
Statistical analysis: Data scrutinization was executed using the excel sheet 2007. All variables were demonstrated as mean ± SD. Assessment values were obtained during the period of treatment. The figure 1 shows the scales and clinical parameters used while assessing the patients.
Results
The values in the table 1 indicate the mean and standard deviation of scores of anxiety, depression and stress in males and females together in case of hypothyroidism, hyperthyroidism and control after receiving the treatment.
Figure 1:Number of patients included in the study.
Table 1:Scores of anxiety, depression and stress.
| Hypothyroidism (mean ± SD) | Hyperthyroidism (mean ± SD) | Control (mean ± SD) | |
|---|---|---|---|
| Scores of anxiety (HARS) | 7.7±3.9 | 7.5±4.3 | 5.0±1.9 |
| Scores of depression (HDRS) | 7.8±4.6 | 8.3±5.1 | 5.3±2.2 |
| Scores of stress (PSS) | 8.2±3.0 | 8.9±2.6 | 6.8±2.3 |
*HARS: Hamilton Anxiety Rating Scale; HDRS: Hamilton Depression Rating Scale; PSS: Perceived Stress Scale. Higher scores in HARS, HDRS and PSS reveal more anxiety, depression and stress.
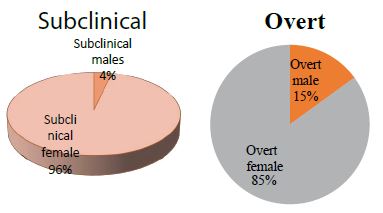
In figure 2 both subclinical and overt hypothyroidism was identified to be more common in females than in males. On terms of subclinical hypothyroidism females engross 96% and males 4%. On other hand in case of overt hypothyroidism females beguile 85% and males 15%.
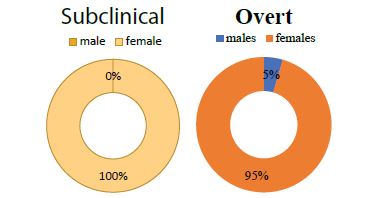
From figure 3 it is clear that hyperthyroidism is typical in female’s juxtaposition to males. Subject to subclinical hyperthyroidism females occupy 100% whereas males 0%. In case of overt hyperthyroidism females hold 95% and males 5%.
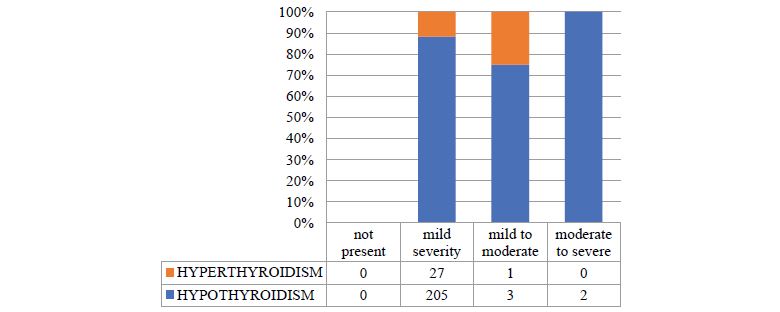
As per figure 4 most patients of hypothyroidism and hyperthyroidism experienced mild anxiety.205 hypothyroidism patients and 27 hyperthyroidism patients are suffering from mild anxiety. Severe anxiety was not observed in hyperthyroidism patients.
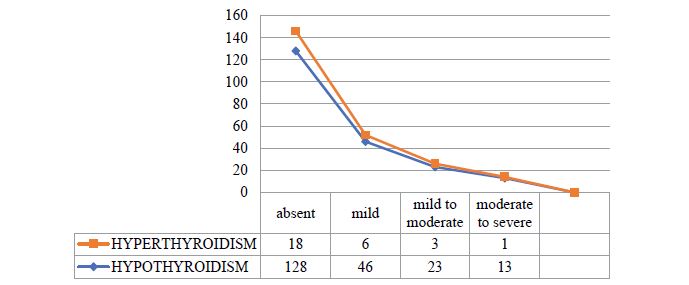
As per figure 5 higher percentage of patient population does not have any depression while minute proportion has mild depression. The fraction of people experiencing moderate and severe depression is found to be equal in case of both hypothyroidism and hyperthyroidism.
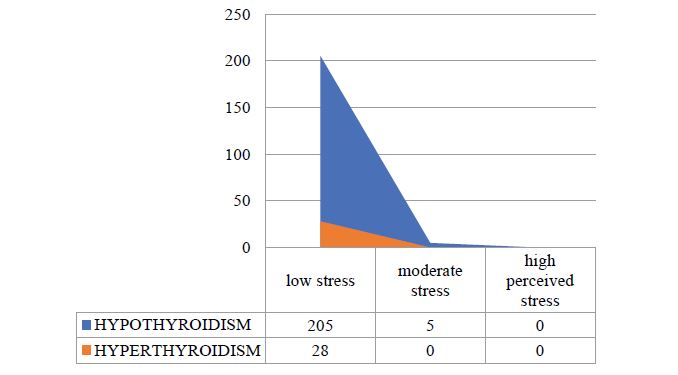
As per figure 6 low stress was identified in significant proportion of patient population of hypothyroidism and hyperthyroidism where as high perceived stress was not seen in both cases. Moderate stress was identified only in case of hypothyroidism.
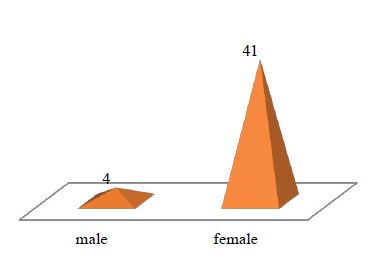
As per figure 7 a total of 45 patients were identified to have thyroid dysfunction plus diabetes mellitus out of which 4 patients were male and 41 patients were female.
Among all the cases, 93% were type 2 diabetes mellitus plus hypothyroidism, 5% were type 1 diabetes mellitus together with hypothyroidism and 2% were type 2 diabetes mellitus plus hyperthyroidism which can be seen in figure 8 beneath.
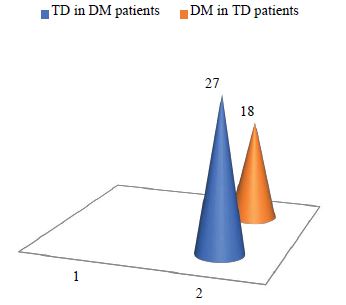
In a total of 45 patients, 27 patients initially have diabetes mellitus and then developed thyroid dysfunction and 18 patients initially have thyroid dysfunction and then developed diabetes mellitus as shown in figure 9.
Figure 2:Gender distribution in hypothyroidism patients.
Figure 3:Gender distribution in hyperthyroidism patients.
Figure 4:Prevalence of anxiety in hypothyroidism and hyperthyroidism.
Figure 5:Prevalence of depression in hypothyroidism and hyperthyroidism
Figure 6:Prevalence of stress in hypothyroidism and hyperthyroidism.
Figure 7:Gender distribution in patients with thyroid dysfunction plus diabetes mellitus.
Figure 8:Prevalence of diabetes mellitus plus thyroid dysfunction.
Figure 9:Prevalence of thyroid dysfunction in patients with diabetes mellitus and diabetes mellitus in patients with thyroid dysfunction.
Discussion
In this research work, patients with thyroid dysfunction were scrutinized in terms of depression, anxiety and stress. In previous studies, it was reported that these variables were mostly found in subclinical hyperthyroidism patients [24]. In our study, it is notable that the levels of these variables are almost similar in both hypothyroidism and hyperthyroidism patients. It is postulated that manifestations of thyroid dysfunction, anxiety and depression contemplate central nervous system β-adrenergic impairment [25, 26]. It is delineated that in utmost cases of hypothyroidism and hyperthyroidism, psychiatric symptoms retained with treatment of the thyroid dysfunction [27]. Stress levels were found to be indistinguishable in case of both hypothyroidism and hyperthyroidism. In our study, it is remarkable that levels of psychological symptoms decline significantly as thyroid function returned to normal, despite the actuality that no psychiatric treatment was applied. The symptoms may be abolished by L-thyroxine therapy [28, 29, 30]. In our study, there were outstanding improvements in levels of anxiety, depression and stress in contrast to the levels at the inception of the treatment. Also, the prevalence of thyroid dysfunction in patients with diabetes mellitus and diabetes mellitus in patients with thyroid dysfunction was scrutinized. It is noticeable from the existing literature that insulin resistance bears a crucial role in associating diabetes mellitus and thyroid dysfunction. Few studies have embellished the relationship between TH, TSH and T2DM and signified that T2DM is negatively related to FT3 and positively interrelated to FT4 in males as well as females and women who are with type 1 diabetes mellitus are at greater risk of symptomatic postpartum thyroid dysfunction and accordingly may advantage from routine thyroid function screening at postpartum visits [31, 32]. Our outcomes divulged homogeneous relationship between TSH, T2DM and TH in both females and males.
Conclusion
In conclusion, the thyroid dysfunction (hypothyroidism and hyperthyroidism) was more habitually observed in females than in males. The extent of anxiety was identified to be almost similar in two cases but the levels of depression and stress were little higher in case of hyperthyroidism patients when compared to hypothyroidism patients. Prevalence of thyroid dysfunction accompanying diabetes mellitus was observed more in females than in males. Instance of thyroid dysfunction in patients with diabetes mellitus was more than the prevalence of diabetes mellitus in patients with thyroid dysfunction. So there is a need for early diagnosis of psychological symptoms and prevalence of diabetes mellitus in patients with thyroid dysfunction.
The authors declare that there’s no conflict of interest concerning the publication of paper.
Acknowledgement
I would like to thank my parents who have supported and encouraged me a lot during my project.
Peter Kopp (2012) Thyroid hormone synthesis. In: Werner and Ingbar’s (eds) The Thyroid: A Fundamental and Clinical Text. (10th ed.) Lippincott Williams & Wilkins, Philadelphia; Pp: 48-74. [ Ref ]
Chopra IJ, Solomon DH, Chopra U, Wu SY, Fisher DA, et al. (1978) Pathways of metabolism of thyroid hormones. Recent Prog Horm Res 34: 521-67. [ Ref ]
Jansen J, Friesema EC, Milici C, Visser TJ (2005) Thyroid hormone transporters in health and disease. Thyroid 15: 757-768. [ Ref ]
Zhang J, Lazar MA (2000) The mechanism of action of thyroid hormones. Annu Rev Physiol 62: 439-466. [ Ref ]
Chiamolera MI, Wondisford FE (2009) Thyrotropin-releasing hormone and the thyroid hormone feedback mechanism. Endocrinology 150: 1091-1096. [ Ref ]
Juan Bernal, Jacques Nunez. Thyroid hormones and brain development. Eur J Endocrinol 1995; 133: 390-398. [ Ref ]
WH Dillmann (1985) Mechanism of action of thyroid hormones. Med Clin North Am 69: 849-861. [ Ref ]
Bunevicius R, Prange AJ Jr. (2010) Thyroid disease and mental disorders: cause and effect or only comorbidity? Current Opinion in Psychiatry 23: 363-368. [ Ref ]
Musselman DL, Nemeroff CB (1996) Depression and endocrine disorders: focus on the thyroid and adrenal system. Br J Psychiatry Suppl 30: 123-128. [ Ref ]
Jackson IM (1998) The thyroid axis and depression. Thyroid 8: 951-956. [ Ref ]
Helmreich DL, Parfitt DB, Lu XY, Akil H, Watson SJ (2005) Relation between the hypothalamic-pituitary-thyroid (HPT) axis and the hypothalamic-pituitary-adrenal (HPA) axis during repeated stress. Neuroendocrinology 81: 183-192. [ Ref ]
Grassetto G, Rubello D (2008) Thyroid disorders and diabetes mellitus. Minerva Med 99: 263-267. [ Ref ]
Mirella Hage, Mira S Zantout, Sami T Azar. Thyroid disorders and diabetes mellitus. J Thyroid Res 439463: 7. [ Ref ]
Wang C (2013) The relationship between type 2 diabetes mellitus and related thyroid diseases. J Diabetes Res. [ Ref ]
Duntas LH, Orgiazzi J, Brabant G (2011) The interface between thyroid and diabetes mellitus. Clinical endocrinology 75: 1-9. [ Ref ]
A Mohn, S Di Michele, R Di Luzio, S Tumini, F Chiarelli (2002) The effect of subclinical hypothyroidism on medical control in children and adolescents with Type 1 diabetes mellitus. Diabetic Medicine 19: 70-73. [ Ref ]
Lin Y, Sun Z (2011) Thyroid hormone potentiates insulin signaling and attenuates hyperglycaemia and insulin resistance in a mouse model of type 2 diabetes. Br J Pharmacol 162: 597-610. [ Ref ]
Blanchet E, Bertrand C, Annicotte JS, Schlernitzauer A, Pessemesse L, et al. (2012) Mitochondrial T3 receptor p43 regulates insulin secretion and glucose homeostatis. FASEB J; 26: 40-50. [ Ref ]
Alexander Iwen K, Schroder E, Brabant G (2013) Thyroid hormones and the metabolic syndrome. Eur Thyroid J 2: 83-92. [ Ref ]
Jansen MS, Cook GA, Song S, Park EA (2000) Thyroid hormone regulates carnitinepalmitoytransferasel alpha gene expression through elements in the promoter and first intron. J BiolChem 275: 34989-34997. [ Ref ]
Gu Y, Li H, Bao X, Zhang Q, Liu L, et al. (2016) The relationship between thyroid function and the prevalence of type 2 diabetes mellitus in euthyroid Subjects. J Clin Endocrinol Metab 102: 434-442. [ Ref ]
Roldan MB, Alonso M, Barrio R (1999) Thyroid autoimmunity in children and adolescents with type 1 diabetes mellitus. Diabetes Nutr Metab 12: 27-31. [ Ref ]
Suzuki Y, Nanno M, Gemma R, Tanaka I, Taminato T, et al. (1994) The mechanism of thyroid hormone abnormalities in patients with diabetes mellitus. Nihon Naibunpi Gakkai Zasshi 70: 465-470. [ Ref ]
Surks MI, Ortiz E, Daniels GH, Sawin CT, Col NF, et al. (2004) Subclinical thyroid disease: scientific review and guidelines for diagnosis and management. JAMA 291: 228-238. [ Ref ]
Stern RA, Prange AJ (1995) Neuropsychiatric aspects of endocrine disorders. In: Kaplan HI, Sadock BJ, (eds.) Comprehensive Textbook of Psychiatry. Baltimore MD: Williams & Wilkins. pp. 241-251. [ Ref ]
Whybrow PC, Prange AJ (1981) A hypothesis of thyroid-catecholaminereceptor interaction, its relevance to affective illness. Arch Gen Psychiatr 38: 106-113. [ Ref ]
Whybrow PC, Bauer M (2000) Behavioral and psychiatric aspects of thyrotoxicosis. In: Sidney C. Werner, Sidney H. Ingbar (eds.) The Thyroid: A Fundamental and Clinical Text. Philadelphia: Lippincott Williams & Wilkins: Pp. 673-678. [ Ref ]
Nyström E, Caidahl K, Fager G, Wikkelsö C, Lundberg PA, et al. (1988) A double-blind cross-over 12-month study of L-thyroxine treatment of women with ‘subclinical’ hypothyroidism. Clin Endocrinol 29: 63-75. [ Ref ]
Jaeschke R, Guyatt G, Gerstein H, Patterson C, Molloy W, et al. (1996) Does treatment with L-thyroxine influence health status in middle-aged and older adults with subclinical hypothyroidism? J Gen Intern Med 43: 744-749. [ Ref ]
Haggerty JJ Jr, Stern RA, Mason GA, Beckwith J, Morey CE, et al. (1993) Subclinical hypothyroidism: a modifiable risk factor for depression? Am J Psychiatry 150: 508-510. [ Ref ]
Boucai L, Hollowell JG, Surks MI (2011) An approach for development of age-, gender- and ethnicity-specific thyrotropin reference limits. Thyroid 21: 5-11. [ Ref ]
Gerstein HC (1993) Incidence of postpartum thyroid dysfunction in patients with type 1 diabetes mellitus. Ann Intern Med 118: 419-23. [ Ref ]