Journal Name: Journal of Health Science and Development
Article Type: Research
Received date: 05 October, 2021
Accepted date: 17 November, 2021
Published date: 2024-02-01
Citation: Chattapadhyay A, Roy N, Gupt R (2021) Current Scenario of Wealth and Child Nutrition in India: Macro and Micro look. J Health Sci Dev Vol: 4, Issu: 2 (23-30).
Copyright: © 2021 Chattapadhyay A et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
The level and relationship of child health, wealth, and basic amenities are changing fast in India. How strong are the relationships of state wealth, i.e., state Gross Domestic Product and basic household amenities like sanitation facilities with child health? Using the published National Family Health Survey 2015-16 at a macro level, the paper compares the change of stunting, underweight and under-five mortality over ten years (National Family Health Survey 2005-06 to 2015-16) and explores how far child health indices are associated with state Gross Domestic Product. Though wealth and child health are positively associated in India, the strength of the relationship is declining over time, indicating that wealth per se may not guarantee the betterment of child health. Undertaking a case study with 510 children in a low-income community of Mumbai, we further establish that the availability of basic facilities and recent infections play a stronger role in determining child nutrition status when household wealth is controlled. Higher-income, more years of schooling, less crowding in a household, covered drainage system, the nonoccurrence of Gastro intestine, and infectious disease are significantly associated with better child nutrition status. Sincere attention to policy on improving basic facilities and living environment to address child health issues has become mandatory. National Health Mission or health programs like Swachh Bharat Abhiyan are good initiatives to focus on improving basic facilities and living environment to address child health issues.
Keywords:
Wealth, Child health, Stunting, Slum, Mumbai
Abstract
The level and relationship of child health, wealth, and basic amenities are changing fast in India. How strong are the relationships of state wealth, i.e., state Gross Domestic Product and basic household amenities like sanitation facilities with child health? Using the published National Family Health Survey 2015-16 at a macro level, the paper compares the change of stunting, underweight and under-five mortality over ten years (National Family Health Survey 2005-06 to 2015-16) and explores how far child health indices are associated with state Gross Domestic Product. Though wealth and child health are positively associated in India, the strength of the relationship is declining over time, indicating that wealth per se may not guarantee the betterment of child health. Undertaking a case study with 510 children in a low-income community of Mumbai, we further establish that the availability of basic facilities and recent infections play a stronger role in determining child nutrition status when household wealth is controlled. Higher-income, more years of schooling, less crowding in a household, covered drainage system, the nonoccurrence of Gastro intestine, and infectious disease are significantly associated with better child nutrition status. Sincere attention to policy on improving basic facilities and living environment to address child health issues has become mandatory. National Health Mission or health programs like Swachh Bharat Abhiyan are good initiatives to focus on improving basic facilities and living environment to address child health issues.
Keywords:
Wealth, Child health, Stunting, Slum, Mumbai
Introduction
Child health is an indicator of development. There is much debate on India’s economic growth and child health, especially on child nutrition. Income is well related to health in three ways (Marmot, 2001): through the gross product, through income of individuals, and through the distribution of wealth over geographic space [1]. (Re) distribution of wealth can improve health. However, if basic community amenities are less (i.e., in a resource-poor setting) or a large section of the society fails to achieve a basic threshold of community amenities, then the individual income, as a determinant of child health, plays a stronger role. Thus our paper questions the following: how far the macro-level wealth determines child health in India? Does the macro association of wealth and health weaken over time? What are the micro-level factors influencing child nutrition in a poor community setting? In a resource poor setting, where the majority hails from low-income households, thus income is somehow standardized, it would be worth seeing the nexus between environment and child health.
Macro study
Preston’s famous log-linear relation between mortality and gross wealth suggests that the strong relation of these two parameters gradually weakens due to other factors that affect the health of a nation [2]. It is not sufficient to assume that economic growth will automatically lead to improved health. On the contrary, Deaton’s analysis in 2007 reveals a weak correlation between height and national wealth [3]. Coffee et al. describe the weakening of the relationship between wealth and health in India in the recent past [4]. They also indicate a negative relation of growth in state net domestic product and change in state-level child health indices, concluding that health is leading to economic growth, rather than vice versa.
The second highest cause of neonatal death in India is infections, while for post neonates and under-five children, mainly diarrhea and respiratory infections, have the major share of death. Child health and mortality, to a great extent, depend on several exogenous factors besides wealth. It is predicted that the global burden of disease and mortality rates could be reduced by about 9.1% and 6.3%, respectively, if we propagate access to safe water, sanitation, and hygiene facilities [5]. In the recent past, the decline in under5 mortality in India is steepest among the lower-income groups, signifying the stronger role of public health care facilities and greater function of basic amenities in reducing the rich-poor gap [6]. However, the poor living condition of the urban lower income group as compared to the rural poor is a matter of concern in India [7]. Hence, we intend to give special focus on the urban poor through a micro-study.
Between 1990 and 2014, as the income of the average Indian rose by an average annual rate of 4.7 percent (in constant 2005 USD), crop yields (kilograms/hectare) of all food grains rose by an average annual rate of about 2.3 percent and 2.5 percent; fewer children died in the first five years of their life on an average annually [8]. Global evidence shows that child undernutrition is only weakly correlated with income. The issue of a child under nutrition is alarming in India, in spite of economic success. This is supported by the fact that in India, 25 percent of the children from the top income quintile were stunted in 2006. India dominates economically in the subcontinent in terms of per capita income. Despite that, nutritional outcomes remain poor, and the indicators for access to improved sanitation and immunization are the lowest in the region. Needless to mention here, the share of health in the union budget has decreased from 0.18 in 2012-13 to 0.12 in 2016-17 [9].
There is the proliferation of recent works on child health and wealth; correlates of child mortality or child nutrition with wealth and income in India. There is a weaker association of child health and wealth at a macro level [10]. East Asian economic miracle is a reflection of health improvement that played a leading role in enhancing economic policies, thus in the entire process of economic development, health is one of the significant predictors of a nation’s wealth [11].
Poor health service delivery in India is the major cause of higher mortality of children aged 1-5. This finding contradicts the conventional narrative of poverty being the primary factor driving differences between mortality outcomes. Mahadevan’s study in the Chittoor district of Andhra Pradesh (1985) three decades ago reveals a high association of house type and household size/crowding with childhood mortality [12]. When family income correlates negatively among the Harijans, it has a positive association among Muslims and Caste Hindus, indicating an opposing influence of income on child health.
Micro study
Thus, besides the economy, many other factors play a key role in child nutrition, especially in resource-poor settings. Children living in the slums are vulnerable to infectious diseases because slum settlements have deplorable living and environmental conditions, which are characterized by inadequate water supply, squalid condition of environmental sanitation, breakdown or nonexistence of waste disposal arrangement, overcrowded and dilapidated habitation, hazardous location, insecurity of tenure, and vulnerability to serious health risks [13]. Poor environmental and housing conditions are the source of heavy disease burden on locality, particularly children because they are vulnerable to infectious diseases [14]. Household hygiene and health-seeking behaviors and care practices are important factors for minimizing the infectious disease and overall morbidity rates among children in the poor urban settlement [15]. According to the Department of Women and Child Development, Government of India (Annual Report, 2007), malnutrition in children is more an interplay of female illiteracy, ignorance about nutritional needs of the infant and young children, and poor access to health care. Thus the need to carry out a micro-study in child nutrition is immense.
Maharashtra, one of the richest states in India, indicates steady improvement in child nutrition. According to National Family Health Survey-4 (2015-16), 34% of children under age five are stunted, which was 46% in 2005-06 (NFHS-3), wasting among children has increased (16.5% to 25.6%). However, there is almost no reduction in underweight among children (37% to 36%) [16]. The recently published Comprehensive Nutrition Survey in Maharashtra (CNSM, 2012) indicates a substantial reduction in the prevalence of stunting from 39% to 23% among children below two years of age. Also, the level of underweight and wasting reflects reduction over the years in CNSM (2012) [17]. However, people living in slums are a different subset, and none of the surveys throw enough light on the nutrition of children living in slums due to its restricted sampling frame [18]. According to the Indian State Hunger Index (ISHI) 2008, Maharashtra’s score was 22.8, which places the state in the 10th position in India, and the state comes in the category of “alarming hunger” at par with the less developed state of Orissa (23.8) (IFPRI, 2009) [19].
Mumbai, the capital of Maharashtra, is well known for its skyscrapers and squatters. Large numbers of people live in slums where the living environment is very poor. The poor sanitation and environmental conditions in the slums make their health vulnerable. Understanding this fact, the Slum Rehabilitation Authority (SRA) rehabilitates slum dwellers to better places to live in an improved environment [20]. The question is whether a difference exists in the nutritional status of children living in rehabilitated areas and slums (notified and non-notified)? Slum clusters of Mumbai often hit headline news. Mankhurd, in eastern Mumbai, is one among these clusters where sixteen children died of severe malnutrition within nine months. The Human Development Report of Greater Mumbai of 2009 showed that the M-East ward of Mumbai, where our study area is located, had the highest infant mortality rate (66.47 per 1,000 live births). It is being said that cleanliness in the household is crucial for healthy living. So, rehabilitated areas can be expected to have a cleaner environment than slums. Thus we can expect better child health outcomes in SRA buildings. It is also argued that along with a clean environment, proper knowledge and practices about child care are necessary for better health. So, whether the knowledge and practices of mothers related to child care differ in slums and rehabilitation areas?
The paper is divided into two parts. The first part demonstrates the changes of stunting and underweight among children less than 5 years in different states of India, culling data from NFHS 3 (2005-06) and NFHS 4 (2015-16). Next, we analyze the association of stunting and under-five mortality with standardized SDGP per capita for two time periods, i.e., 2005-06 and 2015-2016. To explore the determinants of child nutrition in the second part, a micro-study is conducted. It is based on the slums of eastern Mumbai. In the above context, we can hypothesize to get a weaker relation of state net domestic product with child health indices (here stunting and under5 mortality) overtime at a macro scenario; and a significant role of (not only income) other factors mainly, hygienic factors of household and community amenities in determining child nutrition in a poor urban commune.
Methods
The macro analysis is based on two rounds of National Family Health Survey (NFHS) data of 2005-06 and 2015-16. NFHS is a large-scale, multi-round survey conducted in a representative sample of households throughout India. The survey is equivalent to Demographic Health Survey (DHS) in India, and it provides state and national level information and estimates for India on a variety of family and health issues, including infant and child mortality, child health, and nutrition. The third National Family Health Survey, or NFHS- 3, was carried out in 2005-2006, and it provides estimates of the nutritional status of children less than five years for all states. NFHS 4 (2015-16) has recently published a factsheet of 15 states with key indices. The latest survey not only provides estimates for states but for districts as well. The paper compares child health (under-five years) of those states where data for two consecutive periods are available. Economic indicator, i.e., Net State Domestic Product (NSDP) at a standardized rate (with a base price of 14-15), is taken from the published data of the Ministry of Statistics and Programme Implementation.
The indices we analyzed here are stunting, the underweight, and the under-five mortality rate (deaths of children below five years of age). Two standard indices of physical growth, such as height for age (stunting) and weight for age (underweight) indices are used besides the under-five mortality rate. Two nutritional status indicators are expressed in standard deviation units (Z-scores) from the median of the reference population. Each index provides different information about the growth and body composition, which is used to assess nutritional status. The height for age index (stunting) indicates linear growth retardation and cumulative growth deficits. Children whose height for age Z-score (HAZ) is below minus two standard deviations (-2 SD) from the median of the reference population are considered short for age (stunted) and chronically malnourished. Wasting, being the indicator of acute malnourishment is not taken into consideration.
In contrast, underweight (weight for age) is a combined indicator of stunting and wasting and a widely used child health indicator in India at the policy level. Svedberg and Nandy et al. introduced another measure named Composite Index of Anthropometric Failure (CIFA), arguing that this measure can sufficiently estimate the overall prevalence of undernutrition. Das Gupta et al. opine that CIAF provides better under-nutrition status than currently used weightfor- age Z score measurement. The under-five mortality rate is the death between birth and below five years of age, expressed per 1,000 live births, and is an excellent measure of child health.
The micro-study is conducted in the slums (both notified and non-notified) and rehabilitation areas of eastern Mumbai to identify the factors affecting child nutrition besides income. The selected area hails from Mumbai East Ward. The sample size for this study was determined based on the proportion of children stunted in the Mumbai slum (47.4%) as per NFHS-3 (2005-06). We collected information of 510 children cutting across rehabilitation areas (168 children), notified slum areas (174 children), and 168 children from the non-notified slum areas. In each selected area that was segmented, house listing was done for households with at least one child under five years, and then random sampling methods were applied to select households for interview.
Bivariate and multivariate (logistic regression) techniques are used for this study. At the macro level, we plotted the association of SGDP and child health. While to see the determinants of child nutrition at micro studies; we applied five logistic regression models. Model-1 includes background characteristic average monthly income, years of schooling, age, caste, religion, number of children, birth weight, mother BMI. Model-2 shows the determinants of child stunting by living environment indicators, i.e., family member in the household, drainage system, toilet facility, and social relationship. Model-3 includes food consumption and facilities available like consumption of non-vegetarian, distance to milk shop. Model-4 incorporates knowledge,child care practices, and recent diseases related to the child (gastro intestine, respiratory problem, any infection among children in last two weeks before the survey). In Model-5, all variables are considered simultaneously to understand the overall effect of a different set of variables mentioned above on child stunting.
Results
Change in State level child health indices: 2005-06 to 2015-16
State-level indices like under-five mortality rate, stunting, and underweight indicate improvement of child health. Comparing two subsequent NFHS data sets, i.e., 2005-06 and 2015-16, we could say that both indices of undernutrition (stunting and underweight) have improved 5- 10 percentage points across India. Some less developed states like Madhya Pradesh, Bihar, and Meghalaya need better programmatic emphasis as close to 45 percent of children are in these states are stunted. At the same time, states like Orissa, Chhattisgarh, and MP have shown a remarkable reduction of under-five mortality. States with higher levels of undernutrition experience sharper reduction over time. However, Assam has experienced an increase of 7 percent point under-weight children, i.e., from 29.8 percent to 36.4 percent over the past ten years (Table 1).
The coefficient of variation (CV), which is the extent of variability in relation to the population’s mean, is given in the last row of table 1. In all three parameters of child nutrition, CV has reduced, indicating better unanimity in deviation of state values from the total mean. The maximum reduction is observed in child underweight. In 2005-06, when CV was 52.4, it came down to 26.2 in 2016-17. Similarly, distinct reduction of CV is observed for wasting- from 36.9 to 19.7 over a decade. However, the reduction of CV in stunting is marginal, indicating a wide variation of state values from the total mean stunting of India (Table 1).
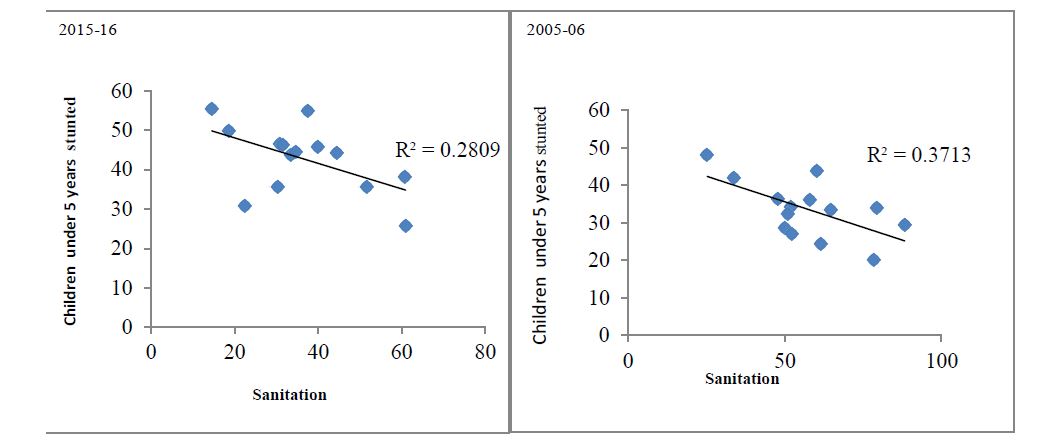
Association of child health with SGDP and sanitation
Figure 1 reveals the association of nutrition indices with state GDPs (SGDP) at two-time points, i.e., 2005-06 and 2015- 16. Simple linear regression analysis shows the strength of association with R2. Though stunting and underweight indicators have a positive association with SGDP, the association with SGDP has become weaker over time. For instance, in 2005-06, the explanatory power of the negative association (R2) of SGDP and child stunting has declined from 0.41 to 0.34. Similarly, the strength of association for underweight and SGDP has reduced from 0.23 to 0 .14 from 2005-06 to 2015-16. However, with the availability of sanitation facilities, a stronger relationship over time is evident. For instance, the R2 value of the association for sanitation and child stunting was 0.28 in 2005-06 and it has increased to 0.37 in 2015-16. So, the analysis suggests that when relations of nutrition indices are becoming weaker with SDGP over time, the availability of sanitation facilities is becoming stronger with child stunting.
Figure 1:Regression Analysis Showing Association of child health with SDGP Sanitation over time.
Table 1:Scenario of Child Health (under-5 years) in India: NFHS 2005-06 and 2015-16.
| Under-five mortality | Percent stunted | Percent underweight | ||||
|---|---|---|---|---|---|---|
| 2005-06 | 2015-16 | 2005-06 | 2015-16 | 2005-06 | 2015-16 | |
| Haryana | 52.0 | 41.0 | 45.7 | 34.0 | 39.6 | 29.4 |
| Punjab | 52.0 | 33.0 | 36.7 | 25.7 | 21.6 | 24.9 |
| Rajasthan | 85.0 | 51.0 | 43.7 | 39.1 | 39.9 | 36.7 |
| Uttarakhand | 56.0 | 47.0 | 44.4 | 33.5 | 26.6 | 38.0 |
| Chhattisgarh | 90.0 | 64.0 | 52.9 | 37.6 | 47.1 | 37.7 |
| Madhya Pradesh | 93.0 | 65.0 | 50.0 | 42.0 | 60.0 | 42.8 |
| Bihar | 84.0 | 58.0 | 55.6 | 48.3 | 55.9 | 43.9 |
| Orissa | 91.0 | 49.0 | 45.0 | 34.1 | 40.7 | 34.4 |
| West Bengal | 59.0 | 32.0 | 44.6 | 32.5 | 38.7 | 31.5 |
| Assam | 84.0 | 56.0 | 46.5 | 36.4 | 29.8 | 36.4 |
| Manipur | 42.0 | 26.0 | 35.6 | 28.9 | 22.2 | 13.8 |
| Meghalaya | 70.0 | 40.0 | 55.1 | 43.8 | 48.8 | 29.0 |
| Sikkim | 40.0 | 32.0 | 38.3 | 29.6 | 19.7 | 14.2 |
| Tripura | 59.0 | 33.0 | 35.7 | 24.3 | 39.6 | 24.1 |
| Goa | 20.0 | 13.0 | 25.6 | 20.1 | 25.0 | 23.8 |
| Gujarat | 61.0 | 43.0 | 51.7 | 38.5 | 44.6 | 39.3 |
| Maharashtra | 46.0 | 29.0 | 46.3 | 34.4 | 37.6 | 35.2 |
| Karnataka | 54.0 | 32.0 | 43.7 | 36.2 | 37.6 | 35.2 |
| Tamil Nadu | 35.0 | 27.0 | 30.9 | 27.1 | 29.8 | 23.8 |
| CV (%) | 35.5 | 32.8 | 36.9 | 19.7 | 52.4 | 26.2 |
Table 2:Prevalence of under nutrition and CIAF1 among children by type of localities M (East) ward Mumbai.
| Rehabilitation Areas | Notified Slum Area | Non-notified Slum | Total | |
|---|---|---|---|---|
| Stunting | 44.0 | 61.5 | 70.2 | 58.6 |
| Wasting | 10.1 | 8.6 | 14.3 | 11.0 |
| Underweight | 30.4 | 40.8 | 52.4 | 41.2 |
| CIAF1 | 52.4 | 67.8 | 76.8 | 65.7 |
| N | 168 | 174 | 168 | 510 |
| 1CIAF-Composite index of anthropometric failure define as children not in anthropometric failure and counts all children who have single or multiple anthropometric failure (stunting, wasting, or underweight). | ||||
Prevalence of under nutritional status of children under age five years is estimated (Table-2), out of 510 children. As observed, 58.6% of children are stunted, 10.9 % are wasted, and 41.2% are underweight. Study examines the under nutritional status of children by type of locality. It shows that stunting (70.2%), wasting (14.2%), and underweight (52%) among children are substantially higher in non-notified slum areas, compared to notify areas (stunting 61.3%, wasting 8.6%, and underweight 40.8%). In rehabilitation areas, 44.1% are stunted, 10.1% are wasted, and 30.4% are underweight (Table 2).
The composite index of anthropometric failure (CIAF) shows that 65.7% of children suffer from anthropometric failure. Prevalence of anthropometric failure (CIAF) is higher in non-notified areas (78%) followed by notified areas (68%) and rehabilitation (52%) areas. Children who are severely stunted (below -3 SD the median of the reference population) are more than two-fifth (42.3) in non-notified slum areas and 33.9% are from notified areas, and 16% are from rehabilitation areas. Similarly, six percent children are wasted in non-notified areas followed by five percent in rehabilitation areas and 2.3% in notified areas. In the context of underweight, severity is higher in non-notified slum (19.6%), followed by notified slum (13.8%) and it is five percent in rehabilitation areas (Table 2). Figure 1 shows the four curves i. e. height-for-age, weight-for-height, weight-for age graph against the normal curve. All curves are shifted towards the left of the standard normal curve, indicating significant under nutrition in slums of eastern Mumbai. However, wasting is not as prevalent as stunting and underweight. Stunting among children is concentrated more where household income is less than Rs 10000 per month, supporting the macro finding that household income is crucial for child nutrition.
1-CIAF-Composite index of anthropometric failure define as children not in anthropometric failure and counts all children who have single or multiple anthropometric failure (stunting, wasting, or underweight).
Multivariate logistic regression model estimates determinants of child nutritional status, controlling household income to assess the factors determining child stunting, besides income (Table 3). There are five models estimated to show the individual, household and communitylevel determinants of child nutrition. In model 1, the average monthly income is significantly negatively associated to stunting among children only when the income is above 16000 per month(OR-0.405), indicating that in a resourcepoor setting there could be many more indices determining child nutrition, besides higher household income.
More than six members in the household (OR-1.564) and open drainage system are positively associated with stunting (model 2). Not eating non-vegetarian food items and providing milk shop away from home (200 and above meters) are also significantly associated with stunting in model 3. In model 4, less knowledge related to child care (OR-0.499) and suffering from gastrointestinal disease (OR-1.529) have significantly higher odds with child undernutrition.
Table 3:Odds of not being stunted among children (aged less than 5 yrs) in Slums of Eastern Mumbai.
| Indicators | Model-1 | Model-2 | Model-3 | Model-4 | Model-5 | |
|---|---|---|---|---|---|---|
| Background Characteristics | ||||||
| Average Monthly Income | <6500® | |||||
| 6500-8500 | 0.794 | 0.974 | ||||
| 9000-15000 | 0.734 | 0.947 | ||||
| 16000+ | 0.405** | 0.364* | ||||
| Years of Schooling | No formal&<5® | |||||
| 8-May | 1.013 | 1.416 | ||||
| 9+ | 0.503** | 0.641 | ||||
| Living Environment | ||||||
| Member in the household | <6® | |||||
| 6+ | 1.564** | 1.532* | ||||
| Drainage System | Open® | |||||
| Covered | 0.653** | 0.772 | ||||
| Food Consumption and Provision of Food Shop | ||||||
| Non-veg | Not consume | |||||
| Consume | 0.675* | 0.795 | ||||
| Distance to Milk shop | <200 meter® | |||||
| 200+ meter | 1.552** | 1.458 | ||||
| Knowledge and child care practices | ||||||
| Lower® | ||||||
| Medium | 0.763 | 1.281 | ||||
| Higher | 0.499*** | 0.729 | ||||
| Disease | ||||||
| Gastro Intestine problem | No® | |||||
| yes | 1.529** | 1.782** | ||||
| Respiratory problem | No® | |||||
| yes | 1.303 | 1.136 | ||||
| Any Other Infection | No® | |||||
| yes | 1.333 | 2.275** | ||||
| Localities | ||||||
| Rehabilitation® | ||||||
| Notified Slum | 1.661 | |||||
| Non-notified Slum | 2.833 | |||||
| Log likelihood | -230.55 | -291.10 | -296.76 | -296.33 | -205.11 | |
| ® reference Category, level of significant ***< 0.01, **<0.05, *<0.10. Controlled for child age, caste, religion number of children, BMI, birth weight, availability of toilet, type of drainage, social relationship is controlled. | ||||||
When all variables are considered together in model 5, lower average monthly income, more household crowding, suffering from gastrointestinal diseases and other recent infections of children are significant determinants of child undernutrition. Place of locality (i.e., slums and rehabilitation areas) does not show any marked difference in child nutrition when all necessary variables are controlled. It proves that it is not a place of residence per se ( slums vis a vis rehabilitation areas), many other factors at household level like, recent infections of child, type of food consumption, household crowding, knowledge of child care practices that determine child nutrition.
Discussion
The paper address many pertinent issues related to child nutrition using NFHS date (2005-06 and 2015-16) and analyzing a micro-study of slums of eastern Mumbai.
We explore the following: how far state wealth is related with child health in India; whether such relation is changing over time; what are the micro-level factors influencing child nutrition in a poor community setting; to what extent the level of child nutrition differs in slums and rehabilitation areas where majority hails from low income households. It is worth understanding the nexus between non economic factors and child nutrition [21].
State domestic product and household income, both at the macro /micro level, are important determinants of child nutrition. Yet, the association of macroeconomic factor is losing its strength over time. Child undernutrition situation has improved evidently in almost all states in India. Still, some states need special attention to improve this situation. The variability of child stunting across states against the nation’s average is distinct, has not reduced over the last decade and thus needs special focus to decrease state variability in stunting.
At the micro level, the paper reveals that besides income, important determinants of child nutrition are housing environment like crowding and sanitation facility; type of food consumption and provision of milk shops in the locality; better child care knowledge and disease-free child growth (mainly recent infections). When all necessary factors are controlled, type of slum has no significant association with child undernutrition. Many non-economic factors mentioned above that include cleaner surroundings and provision of based facilities along with knowledge dissemination regarding child care play a crucial role in determining child nutrition.
Our analysis indicates huge investment requirement for improving basic facilities. While the microanalysis proves the benefits of improved living conditions through government rehabilitation programmes for urban poor, yet there is a need ahead to implement housing policy with importance of hygiene and cleanliness awareness which would improve the living environment and health status of children. Interventions may include the betterment of the sanitation facility, knowledge dissemination on necessary child care practices and improved diet, and economic and educational improvement.
Conclusion
The government’s efforts for improvement of living conditions of a large proportion of the urban population living in the slums are evident. However, there is a need ahead to implement housing policy with the importance of hygiene and sanitation awareness, which will improve the children’s living condition and health status. Interventions are necessary to address the widespread under nutrition to improve child health, resulting in a shift in the curves closer to the reference standard. Interventions may include betterment of the surrounding environment, economic improvement, priorities of basic facility, knowledge imparting on basic child care practices by grass root level worker, and improvement in diet. Involvement of community groups with urban local body/authority to monitor and give feedback on services in the community can improve the living and health condition. Target the needs of vulnerable groups, especially children in low-income households. Regular cleaning of drainage, provision of toilet facility, provision of healthy food for the poor are essential short-term goals besides improving mother’s condition and income generation. Only constructing better housing may not solve problems of child nutrition.
Conflict of Interest
There is no conflict of interest between the authors or others.
Marmot M (2001) Inequalities in health. N Engl J Med 345: 134-136. [ Ref ]
Preston Samuel H (1975) The Changing Relation between Mortality and Level of Economic Development. Population Studies 29: 231-248. [ Ref ]
Deaton A (2007) Height, health, and development. Proceedings of the National Academy of Sciences 104: 13232-13237. [ Ref ]
Coffey D, Chattopadhyay A, Gupta R (2014) Wealth and health of children in India: A state-level analysis. Economic Political Weekly 49: 64-70. [ Ref ]
Prüss-Ustün A, Bonjour S, Corvalán C (2008) The impact of the environment on health by country: a meta-synthesis. Environ Health 7: 7. [ Ref ]
You D, Hug L, Ejdemyr S, Beise J. Levels and trends in child mortality. Report 2015. Estimates developed by the UN Inter-agency Group for Child. Levels and Trends in Child Mortality Report 2015 | United Nations Population Division | Department of Economic and Social Affairs [ Ref ]
Chattopadhyay A, Roy TK (2016) Are urban poor doing better than their rural counterpart in India? A study of fertility family planning and health. Demography India 34: 299-312. [ Ref ]
International Institute for Population Sciences. India National Family Health Survey (NFHS-3), 2016-17. International Institute for Population Sciences; 2015. [ Ref ]
Arimah BC, Branch CM (2011) Slums as expressions of social exclusion: Explaining the prevalence of slums in African countries. International Conference on Social Cohesion and Development, Paris. [ Ref ]
Beşer A, Topçu S, Çoşkun A, Erdem N, Gelişken Akyüz R, et al. (2010) Traditional child care practices among mothers with infants less than 1 year old. Hemşirelik Yuksekokulu Elektronik Dergisi 3: 137-145. [ Ref ]
Dasgupta A, Parthasarathi R, Biswas R, Geethanjali A (2014) Assessment of undernutrition with composite index of anthropometric failure (CIAF) among under-five children in a Rural Area of West Bengal. Indian Journal of Community Health 26: 132-138. [ Ref ]
Harrison LH, Moursi S, Guinena AH, Gadomski AM, el-Ansary KS, et al. (1995) Maternal reporting of acute respiratory infection in Egypt. Int J Epidemiol 24: 1058-1063. [ Ref ]
International Food Policy Research Institute (2009) India State Hunger Index report. [ Ref ]
International Institute for Population Sciences (2007) India National Family Health Survey (NFHS-3), 2005-06. [ Ref ]
Mahadevan K, Murthy MS, Reddy PR, Reddy PJ, Gowri V, et al. (1985) Socio-demographic correlates of infant and childhood mortality. Rural demography 12: 21-40. [ Ref ]
Ministry of women and child development, ‘world fit for child’ (2007) Government of India. [ Ref ]
Ndugwa RP, Zulu EM (2008) Child morbidity and care-seeking in Nairobi slum settlements: the role of environmental and socio-economic factors. J Child Health Care 12: 314-328. [ Ref ]
Pongou R, Ezzati M, Salomon JA (2006) Household and community socioeconomic and environmental determinants of child nutritional status in Cameroon. BMC public health 6: 98. [ Ref ]
Registrar General of India census New Delhi (2011) Office of the Registrar General and Census Commissioner. [ Ref ]
Svedberg P (2000) Poverty and Under nutrition: theory, measurement and policy. New Delhi: Oxford India. [ Ref ]
Smith JP (1999) Healthy bodies and thick wallets: the dual relation between health and economic status. Journal of economic perspectives 13: 144-166. [ Ref ]