Journal Name: Journal of Health Science and Development
Article Type: Research
Received date: 23 July, 2021
Accepted date: 11 October, 2021
Published date: 2024-02-01
Citation: Chau I, Dastagir N (2021) Demographics of Syncope in Regional Australia. J Health Sci Dev Vol: 4, Issu: 2 (18-22).
Copyright: © 2021 Chau I et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Background: Syncope is one of the commonest presentations to the Emergency Departments. There is limited data on the incidence of syncope in regional Australia. Syncope is classified by its etiological causes and each cause is characterized by different clinical features and prognosis. Identifying the cause of syncope patients is essential to preventing patient morbidity and mortality. Investigating the demographics of syncope in regional Australia may lead to better outcome.
Methods:178 patients were identified and studied after presenting with syncope to the Grafton Hospital. The causes of syncope and clinical features were recorded. Each group of syncope causes was compared against each other. Contingency test (Fisher’s exact test) was used to examine the significance for categorical data.
Results:The age-adjusted causes of syncope showed a significant rise in cardiac syncope in patients aged above 60 (P=0.03) whereas patients below 30 were more likely to suffer from reflex syncope (P=0.0001). There are considerable overlaps such as prodromal symptoms or prior positions of patients between different types of syncope. 77 from 178 Patients (43.3%) would be classified as high risk. 18 out of 24 (75%) cardiac syncope patients were classified as high-risk, whereas barely more than 35% (18 out of 51) of patients with reflex syncope were highrisk. Patients with cardiac syncope were more likely to be admitted or referred for further evaluation such as telemetry, Holter monitor and echocardiogram (P=0.0001). Cause-adjusted mortality showed that patients with orthostatic syncope had significantly worse outcome compared to other groups (P=0.04), cardiac syncope patients were not associated with increased mortality (P=0.37).
Conclusion:The current study showed that Syncope is a frequent diagnosis within the emergency department. The incidence of syncope of unknown cause remains very high despite extensive investigations. Clinical features such as prodromal symptoms, prior position or activities leading to syncope did not show significantly difference between causes, therefore are unreliable resources in determining the cause of syncope. Orthostatic syncope was associated with the highest mortality rate therefore we recommend paying particular attention, specialist referral and more extensive investigations in patients with orthostatic syncope.
Keywords:
Syncope, Regional Australia, Cardiac Syncope.
List of Abbreviations:
ED – Emergency Department.
Background: Syncope is one of the commonest presentations to the Emergency Departments. There is limited data on the incidence of syncope in regional Australia. Syncope is classified by its etiological causes and each cause is characterized by different clinical features and prognosis. Identifying the cause of syncope patients is essential to preventing patient morbidity and mortality. Investigating the demographics of syncope in regional Australia may lead to better outcome.
Methods:178 patients were identified and studied after presenting with syncope to the Grafton Hospital. The causes of syncope and clinical features were recorded. Each group of syncope causes was compared against each other. Contingency test (Fisher’s exact test) was used to examine the significance for categorical data.
Results:The age-adjusted causes of syncope showed a significant rise in cardiac syncope in patients aged above 60 (P=0.03) whereas patients below 30 were more likely to suffer from reflex syncope (P=0.0001). There are considerable overlaps such as prodromal symptoms or prior positions of patients between different types of syncope. 77 from 178 Patients (43.3%) would be classified as high risk. 18 out of 24 (75%) cardiac syncope patients were classified as high-risk, whereas barely more than 35% (18 out of 51) of patients with reflex syncope were highrisk. Patients with cardiac syncope were more likely to be admitted or referred for further evaluation such as telemetry, Holter monitor and echocardiogram (P=0.0001). Cause-adjusted mortality showed that patients with orthostatic syncope had significantly worse outcome compared to other groups (P=0.04), cardiac syncope patients were not associated with increased mortality (P=0.37).
Conclusion:The current study showed that Syncope is a frequent diagnosis within the emergency department. The incidence of syncope of unknown cause remains very high despite extensive investigations. Clinical features such as prodromal symptoms, prior position or activities leading to syncope did not show significantly difference between causes, therefore are unreliable resources in determining the cause of syncope. Orthostatic syncope was associated with the highest mortality rate therefore we recommend paying particular attention, specialist referral and more extensive investigations in patients with orthostatic syncope.
Keywords:
Syncope, Regional Australia, Cardiac Syncope.
List of Abbreviations:
ED – Emergency Department.
Background
Syncope is defined as transient loss of consciousness, a symptom caused by global cerebral hypoperfusion characterised by sudden onset, short duration and spontaneous complete recovery [1]. Syncope may or may not be accompanied by preceding warning signs, such as light-headedness, nausea and diaphoresis known as ‘presyncope’. These prodromes may also occur alone without subsequent syncope.
One European study found that syncope accounted for less than one percent of presentations to community based Emergency Department (ED) [2]. The incidence of syncope according to age distribution is bimodal, occurring mostly between the ages of 10 to 30 and in those above 65 years of age attributable to different causes [3,4]. Syncope is universally classified by its aetiological causes, in one European study 21.2% were reflex, 9.5% cardiac, 9.4% orthostatic and the rest were of unknown cause [5]. It has also been shown that the outcome of syncope is related to its underlying cause: ranging from reflex syncope, which has a relative benign prognosis to cardiac syncope which has increased risk of death with the latter having a 5-year mortality rate of over 50% [5,6]. Identifying the cause of syncope is therefore of paramount importance in guiding appropriate treatment.
One of the most difficult challenges of identifying the cause of syncope is the history taking itself, because syncope episodes are often unwitnessed or patients are unaware of what has happened. There may however be specific clinical features before and after the event that may give clinicians indications the cause of syncope [7,8].
According to the European Society of Cardiology guidelines, the initial evaluation should be aimed at establishing whether the patient actually had a syncope episode through comprehensive history taking from patients and witnesses [1]. The second aim should be to establish its underlying cause, by physical examination, ECG evaluation and orthostatic challenge test to rule out cardiac and orthostatic causes. The third aim is to stratify the risk of future cardiovascular events and deaths, a similar guideline with management algorithm has also been developed by McDermott [9].
The aim of this study is to identify and present relevant demographic data in all types of syncope, such as their clinical features, morbidity and mortality profile, which may raise clinicians’ awareness and understanding of this common clinical presentation in order to improve management standards and patients’ outcome, particularly in under-resourced or regional hospitals.
Methods
This was a retrospective study aimed at determining the incidence of Syncope who presented to the emergency department at Grafton Hospital with a final discharge diagnosis of syncope in the period between the 1st of January 2010 until the 31st of December 2011.
Once identified, all relevant data which did not include identifiable personal information such as patient demographics, clinical features, initial assessment, further investigations and mortality profile were recorded. Patients were excluded if they did not fulfil the definition of syncope nor had missing data that were deemed too substantial to the Author.
This study was approved by the Human Research Ethics Committee (HREC) and the University of Wollongong (UOW) ethics committee in accordance with the NHMRC National Statement on Ethical Conduct in Human Research. Data collected were extracted into Excel by the Author in a deidentified way, which only contained Medical Record Number (MRN) and patients’ date of birth. No other identifiable personal information of patients or clinicians was recorded.
This study was conducted by a former medical student, Dr. Chau, supervised by consultant physician at the Grafton Hospital, Dr. Dastagir and supported by the Graduate School of Medicine University of Wollongong, Australia.
Data analysis
To compare the baseline characteristics between subgroups or comparison between a subgroup with the rest of the patients. Contingency test (Fisher’s exact test) was used to examine the significance for categorical data, odds ratio with 95% confidence intervals were calculated with the use of logistic regression. No adjustments were made for multiple testing.
Results
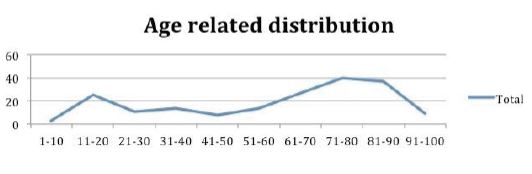
According to our patient records, 257 patients presented to the ED with syncope in Grafton Hospital, NSW between January 2010 and December 2011. 178 of them fulfilled the definition of syncope and confirmed by final ED discharge diagnosis were included in the study. In total 45,897 patients presented to the ED within this two-year period, syncope contributed 0.6% of all ED presentations. The age related bimodal distribution of syncope is illustrated in figure 1, peaking at age 11 to 20 and 61 to 90.
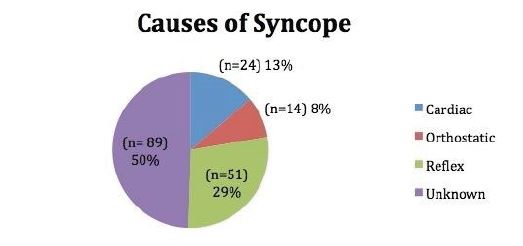
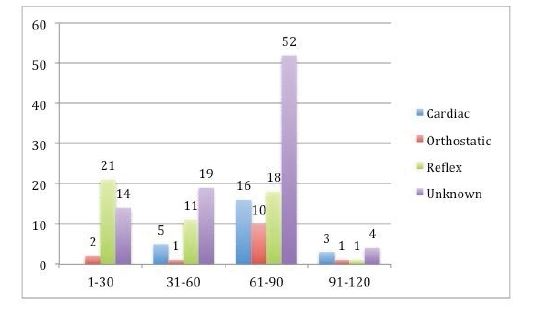
The overall causes and age-adjusted causes of syncope are illustrated in figures 2 and 3, which show a significant rise in cardiac syncope in patients aged above 60 (Odds ratio 3.00 95% CI (1.07 – 8.46), P=0.03) whereas patients below 30 were more likely to suffer from reflex syncope (Odds ratio 4.86 95%CI (2.26 – 10.44), P=0.0001).
The clinical features examined in this study including events leading to and after syncope, previous syncope, initial findings and mortality within two years, these are summarized in table 1.
Clinical features such as prodromal symptoms or prior position of patient did not produce statistical significance to reliably indicate the type of syncope patients might have. There may be considerable overlap in preceding events between different types of syncope.
Prodromal symptoms are more frequently observed in patients with orthostatic syncope, but there is no statistical difference (Odds Ratio 4.36 95%CI (0.94 – 20.1), P= 0.06).
Figure 1:Age related distribution of all cases Syncope.
Figure 2:Causes of Syncope.
Figure 3:Age-adjusted causes of syncope.
The loss of postural tone in syncope means that patients are likely to suffer from subsequent falls, which may lead to physical injury. The immediate sequelae may change or extend management plan. Our study found that up to 28.7% (n=51) patients with syncope have sustained immediate injury. The extent of their injury was not recorded specifically and is not the aim of this study.
Risk stratification is an important element of evaluation to decide whether patients are safe for discharge or whether they warrant admission and further evaluations. In the current study, 77 out of the 178 patients (43.3%) would be classified as short-term high risk. High-risk patients should be referred to specialists or admitted for further investigations. We used this stratification (Appendix 1) to categorize our patients retrospectively based on our demographic data into high or low risk profile using the latest high-risk admission criteria guideline1.
Risk profile vs cause of syncope
We used parametric comparison test to determine if the cause of syncope correlates patients’ risk profile. As shown in Table 1, 18 out of 24, 75% (Odds ratio 4.83 95%CI 1.82-12.86, P=0.0016) of cardiac syncope patients would be classified as high-risk, whereas less than 36% of patients with reflex syncope have had a high-risk profile.
Cause of syncope vs referral/further investigations
A higher proportion of patients with cardiac syncope were admitted or referred for further investigations such as telemetry, Holter monitor and echocardiogram (n= 21/24, 87.5%, Odds ratio 11.59 95%CI 3.31 – 40.56, P=0.0001) compared to other groups.
Cause of syncope vs mortality
Known mortality within two years is shown in Table 1. Records showed that 20 (11.2%) of the 178 patients have died within two years after presenting to hospital with syncope. Patients with orthostatic syncope had the highest recorded proportion of mortality (n=4/14, 28.6% OR 3.7 95%CI 1.04-13.1, P=0.04) followed by cardiac syncope (n=4/24, 16.7% OR 1.73 95%CI 0.52-5.68, P=0.37) and syncope of unknown cause with a considerable mortality rate (n= 10/89, 11.2% Odds ratio 1.0 95%CI 0.39-2.54, P=1.0), whilst reflex syncope had the lowest (n= 2/51, 3.9% Odds ratio 0.25 95% CI 0.06 – 1.11, P=0.07).
Risk profile vs mortality
We also used parametric test to determine retrospectively if short-term high-risk patients were more likely die within two years and vice versa. We found that only 7 out of 77 (9.1%) high-risk patients died within 2 years. 88 from 101 (87.1%) low-risk patients were still alive within 2 years (Odds ratio 0.68, 95%CI 0.26-1.79, P=0.43).
Discussion
This study aimed to assess the demographics of syncope in a regional hospital in Australia. Our data have shown some confounding results in this regard.
Incidence
The incidence of syncope at this ED is slightly lower compared to other literature [2]. One of the explanations is that pre-syncope was not included in this study, due to its variable nature of presenting symptoms within the ED records, we also only selected patients with a final discharge diagnosis of syncope. Patients with syncope may also have other presenting problem such as ‘Falls’, ‘Collapse’ or ‘Dizziness’ or were given other final diagnosis; therefore the real incidence of syncope may be higher. Other patients who have been excluded from the study, despite presenting to the ED with ‘syncope’ as a presenting problem, included patients who presented with dizziness, pre-syncope and did not fulfil the definition of syncope.
Clinical features
Reflex syncope is often associated with precipitants such as fear and preceding symptoms such as light-headedness and nausea; while orthostatic syncope is associated with change of posture, dehydration or the use of antihypertensive medications [7]. Cardiac syncope is associated with sitting or lying position, post exertion, absence of preceding symptoms and a history of cardiac disease [8].
Table 1:Demographics and characteristics of all studied patients.
| Characteristics | All Patients (N=178) | Cardiac (N=24) | Orthostatic (N=14) | Reflex (N=51) | Unknown (N=89) |
|---|---|---|---|---|---|
| Mean Age | 51.4 | 72.8 | 67.6 | 44.3 | 60.1 |
| Age > 60 | 105 (58.9) | 19 (79.2) | 11 (78.5) | 19 (37.3) | 56 (62.9) |
| Age < 30 | 37 (20.8) | 0 (0) | 2 (14.3) | 21 (41.2) | 14 (15.7) |
| Position Prior to Syncope | |||||
| Standing | 95 (53.3) | 13 (54.2) | 8 (57.1) | 33 (64.7) | 22 (24.7) |
| Non-Standing | 42 (23.6) | 6 (25) | 3 (21.4) | 11 (21.6) | 41 (46.1) |
| Unknown | 41 (23) | 5 (20.8) | 3 (21.4) | 7 (13.7) | 26 (29.2) |
| Prodromal Symptoms | 107 (60.1) | 14 (58.3) | 12 (85.7) | 31 (60.8) | 50 (56.2) |
| Without Prodromal Symptoms | 71 (39.9) | 10 (41.7) | 2 (14.3) | 20 (39.2) | 39 (43.8) |
| Prior Syncope | 51 (28.7) | 11 (45.8) | 7 (50) | 9 (17.6) | 24 (27) |
| Activity leading to Syncope | |||||
| Situational even prior to syncope (Urination, Defaecation, Fear or change in posture) | 74 (41.6) | 7 (29.2) | 6 (42.9) | 29 (56.9) | 32 (36) |
| Excretion prior to syncope | 25 (14) | 5 (20.8) | 2 (14.3) | 6 (11.8) | 11 (12.4) |
| At rest or unknown event prior to syncope | 79 (44.4) | 12 (50) | 6 (42.9) | 15 (29.4) | 46 (51.7) |
| Abnormal ECG | 54 (30.3) | 12 (75) | 5 (35.7) | 5 (9.8) | 26 (29.2) |
| Postural Hypotension | 20 (11.2) | 2 (8.3) | 12 (85.7) | 3 (5.9) | 3 (3.4) |
| High risk profile | 77 (43.3) | 18 (75) | 5 (35.7) | 18 (35.3) | 36 (40.4) |
| Immediate Injury | 51 (28.7) | ||||
| Admitted or referred for further investigations | 79 (44.4) | 21 (87.5) | 4 (28.6) | 12 (23.5) | 42 (47.2) |
| Mortality | 20 (11.2) | 4 (16.7) | 4 (28.6) | 2 (3.9) | 10 (11.2) |
In our study we found no statistically significant patterns of preceding event in particular prior position or prodromal symptoms to suggest the cause of syncope, as opposed to those that were suggested by previous studies [7,8]. Therefore, we conclude that it is inadequate to determine the cause of syncope based on history of presenting complaint alone. This highlights the importance of assessments such as ECG and orthostatic challenge, which are important tools to rule out specific causes of syncope.
Causes of syncope
An important reason for categorising syncope patients by its cause is due to the fact that different causes of syncope may lead to different management and prognosis.
The distribution of syncope by causes in this study was similar to Ganzeboom, with syncope of unknown cause being close to 50%, followed by reflex, cardiac and orthostatic syncope [3].
Diagnosing Syncope is a diagnostic challenge in itself. The large proportion of patients who presented with syncope of unknown cause prompted the investigators to question whether it is the peculiar nature of syncope: for example, a patient suffered from a syncope episode, but was completely asymptomatic by the time they presented to the ED, despite extensive investigations no apparent cause could be found; or whether practices of clinicians for managing syncope are in line with the current recommended guidelines. For this reason, we investigated whether the practice of ED clinicians for diagnosing syncope was in line with the current recommended guideline. However data concerning management standard of syncope within the ED is beyond the aim this article, we will reveal these results in our future publication.
This group (syncope of unknown cause) of patients is of particular interest for the following reasons: they represent the highest proportion of syncope cause; their underlying cause is unknown therefore the decision for further management is often difficult and lastly the risk that a more insidious problem may lie within this group of patients, such as cardiac abnormalities, which is why we compared this group of patients with reflex syncope (benign course) and cardiac syncope (sinister course) to evaluate its presenting profile and mortality. But we found no statistical difference in their clinical features and mortality profile compared to the rest of the population.
Cardiac syncope will generally require further diagnostic tests, such as Holter monitoring or echocardiography, depending on the extent and type of diseases these tests may lead to further treatment such as valve replacement or pacemaker insertion, in cases of aortic stenosis and arrhythmic heart disease in order to prevent premature death related to these conditions [1].
Cause of syncope vs mortality
Cardiac syncope is often associated with a high mortality and treatment of underlying cardiac condition is required whereas reflex syncope is associated with a benign course and generally no treatment is required [7]. On the contrary, our study found that orthostatic syncope was associated with the highest mortality, followed by cardiac syncope and syncope of unknown cause. This may be due to the fact that the more sinister course of cardiac syncope has been well documented and often referred (referral rate 87.5%) for further diagnostic tests and subsequent treatment; whereas the lack of apparent danger of orthostatic syncope may have prevented further investigations, yet the insidious nature of orthostatic syncope demonstrated the highest mortality within all patient subgroups.
Conclusion
The current study indicated that the incidence of syncope in this ED is comparable with previous research. Syncope of unknown cause represents the largest proportion of patients. History and clinical features such as prodromal symptoms are not reliable indicators in determining the underlying cause of syncope. Thorough assessment including physical examination, ECG and Orthostatic Challenge should be used to rule out specific causes of syncope. Cardiac syncope should be referred or admitted for further investigations. We found that orthostatic syncope was associated with the highest mortality rate, contrary to previous studies. Therefore, we recommend paying particular attention, specialist referral and more extensive investigations in patients with orthostatic syncope.
Declarations
Ethics approval and consent to participate
This study was approved by the Human Research Ethics Committee (HREC) and the University of Wollongong (UOW) ethics committee in accordance with the NHMRC National Statement on Ethical Conduct in Human Research. As this was a retrospective study, no consent from patients was obtained.
Availability of data and materials
Data collected were extracted into Excel by the Author in a de-identified way, which only contained Medical Record Number (MRN) and patients’ date of birth. No other identifiable personal information of patients or clinicians was recorded. The datasets used and/ or analysed during the current study are available from the corresponding author on reasonable request.
Competing interests
The author declare that they have no competing interests.
Funding
No funding was received for this study.
Author’s contributions
IC collected and analysed the data regarding presentation of syncope in the emergency department and wrote this manuscript. ND had the original idea of this study and supervised this study. All authors read and approved the final manuscript.
Acknowledgments
We thank Dr. Susan Thomas at the Graduate School of Medicine, University of Wollongong for her contribution in proof-reading and providing assistance in statistical analysis of this study.
Author’s information
IC was a former medical student at the University of Wollongong, Australia, whilst this study was being conducted. At the time of submission of the manuscript he is an intensive care physician trainee.
ND is a consultant physician at the Grafton Base Hospital, NSW, Australia.
Brignole M, Moya A (2018) Practical Instruction for the 2018 ESC Guidelines for the diagnosis and management of syncope. The Task Force for diagnosis and management of syncope of the European Society of Cardiology (ESC). European Heart Journal 39: 1883-1948. [ Ref ]
Olde Nordkamp LR, van Dijk N, Ganzeboom KS (2009) Syncope prevalence in the ED compared to general practice and population: a strong selection process. Am J of Emerg. Med Mar 27: 271-279. [ Ref ]
Ganzeboom KS, Colman N, Reitsma JB (2003) Prevalence and triggers of syncope in medical students. Am J Cardiol 91: 1006-1008. [ Ref ]
Colman N, Nahm K, Ganzeboom KS, Shen WK, Reitsma J, et al. (2004) Epidemiology of reflex syncope. Clin Auton Res 14(Suppl 1): i9-i17. [ Ref ]
Soteriades ES, Evans JC, Larson MG (2002) Incidence and prognosis of syncope. N Engl J Med 347: 878-885. [ Ref ]
Kapoor WN (1990) Evaluation and outcome of patients with syncope. Medicine 69: 160-175. [ Ref ]
Brignole M, Alboni P, Benditt DG (2004) Guidelines on management (diagnosis and treatment) of syncope – update 2004. Eur Heart J 25; 2054-2072. [ Ref ]
American College of Emergency Physicians (2001) Clinical policy: critical issues in the evaluation and management of patients presenting with syncope. Ann Emerg Med 37: 771-776. [ Ref ]
McDermott D, James VQ (2020) Approach to the adult patient with syncope in the emergency department. UpToDate. [ Ref ]