Journal Name: Journal of Health Science and Development
Article Type: Research
Received date: 23 August, 2021
Accepted date: 06 September, 2021
Published date: 2024-02-01
Citation: Xiaodong F, Wei Z, Bi T, Cheng G, Bai S, et al. (2021) Depression and Quality of Life among Patients with Secondary Hyperparathyroidism: Mediation Effect of Sleep Quality. J Health Sci Dev Vol: 4, Issu: 1 (12-18).
Copyright: 2021 Xiaodong F, Wei Z et al. This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Background: Secondary hyperparathyroidism (SHPT) is a common and serious complication in patients with renal disease on maintenance dialysis (RDMD) (incidence rate: 30%–80%). The main psychological symptoms of patients with SHPT are depression and poor sleep quality and memory; these seriously affect patient quality of life (QOL). However, there is no large-scale systematic research on the psychological states of patients with SHPT.
Objectives:To analyze a mediation hypothesis through a path analysis, explaining the association of depression with QOL, considering the effects of sleep quality, among patients with SHPT.
Methods:A sample of 320 SHPT patients with total parathyroidism (t-PTX) answered questionnaires concerning sociodemographic status (gender, age, marital status, occupation, degree of education, income, residential area, medical insurance, years of renal failure, and dialysis mode), depression, sleep quality, and QOL. Descriptive statistics, Pearson’s correlation, t test, variance analysis, multiple linear regression analysis, and structural equation modeling (SEM) were performed based on the results of the normality test.
Results:The mean scores for depression, sleep quality, and QOL were 46.04±8.98, 10.94±4.24, and 41.76±8.15, respectively. The prevalence of depression and sleep disorder was 77.81% and 78.13%, respectively. QOL negatively correlated with depression and sleep disorders (r=-0.465, P<0.01; r=-0.468, P<0.01). Sleep quality acted as a mediator between depression and QOL in SHPT patients (mediation proportion: 38.55%). This suggests that it is important to establish selfcare practices, such as improved sleep quality, to improve psychological status.
Conclusion:SHPT patients have high depression levels and poor sleep quality and QOL. It is important to consider the association of sleep quality with depression and QOL in SHPT patients and further to test interventions for minimizing health impacts in this population.
Keywords:
SHPT; Depression; Sleep quality; QOL; Mediation effect.
Abstract
Background: Secondary hyperparathyroidism (SHPT) is a common and serious complication in patients with renal disease on maintenance dialysis (RDMD) (incidence rate: 30%–80%). The main psychological symptoms of patients with SHPT are depression and poor sleep quality and memory; these seriously affect patient quality of life (QOL). However, there is no large-scale systematic research on the psychological states of patients with SHPT.
Objectives:To analyze a mediation hypothesis through a path analysis, explaining the association of depression with QOL, considering the effects of sleep quality, among patients with SHPT.
Methods:A sample of 320 SHPT patients with total parathyroidism (t-PTX) answered questionnaires concerning sociodemographic status (gender, age, marital status, occupation, degree of education, income, residential area, medical insurance, years of renal failure, and dialysis mode), depression, sleep quality, and QOL. Descriptive statistics, Pearson’s correlation, t test, variance analysis, multiple linear regression analysis, and structural equation modeling (SEM) were performed based on the results of the normality test.
Results:The mean scores for depression, sleep quality, and QOL were 46.04±8.98, 10.94±4.24, and 41.76±8.15, respectively. The prevalence of depression and sleep disorder was 77.81% and 78.13%, respectively. QOL negatively correlated with depression and sleep disorders (r=-0.465, P<0.01; r=-0.468, P<0.01). Sleep quality acted as a mediator between depression and QOL in SHPT patients (mediation proportion: 38.55%). This suggests that it is important to establish selfcare practices, such as improved sleep quality, to improve psychological status.
Conclusion:SHPT patients have high depression levels and poor sleep quality and QOL. It is important to consider the association of sleep quality with depression and QOL in SHPT patients and further to test interventions for minimizing health impacts in this population.
Keywords:
SHPT; Depression; Sleep quality; QOL; Mediation effect.
Introduction
SHPT is a common complication in the end of chronic renal failure, which leads to bone pain, heterotopic ossification, and pruritus. Because of the disorder of calcium and phosphorus metabolism, the decrease of vitamin D receptor activity, the down-regulation of calcium sensitive receptor expression, and the decrease of 1,25(OH)2D3 synthesis, the hyperparathyroidism of parathyroid hormone (PTH) was stimulated [1-3]. High PTH levels can easily lead to multiple system damage, especially cardiovascular events, bone metabolism disorders, nervous system damage, calcification defense, and anemia, which seriously affect the patient survival rate [4,5].
In a previous clinical investigation, we found that SHPT patients have certain personality characteristics, such as paranoia, anxiety, and depression [6]. Negative impacts of sleep insufficiency and poor sleep quality on the physical, emotional, mental, and social domains of life have been reported, both on a short- and long-term basis [7,8]. Furthermore, a bi-directional relationship between sleep and emotions has been demonstrated by Kahn, and has been referred to as a vicious cycle [9]. Thus, sleep disorders are a variable of great importance when considering patients with SHPT, because they may impact several issues, such as memory and concentration impairments, increased symptoms of dialysis discomfort, hypercalcemia, increased risk of falls leading to fractures, and decreased ability to accomplish daily tasks [10]. Therefore, a better understanding of the multitude of factors impacting sleep quality is warranted to promote QOL.
Saei et al. showed that QOL has a strong correlation with depression or anxiety [11]. Markarian et al. proposed a protection model suggesting that poor sleep quality tended to compromise emotional regulation, which in many case, led to depression and nightmares, leading to new deficiencies in QOL and increased temper [12]. Thus, further research is needed to understand the relationship between sleep quality and depression and impact that this relationship may have on QOL [13]. In this study, we tested a mediation hypothesis via SEM, explaining how depression is associated with QOL, considering the effect of sleep quality, among patients with SHPT.
Methods
Participants
A cross-sectional study was conducted at a third-class hospital in Liaoning province, China, from January 2017 to December 2019. The inclusion criteria for the participants were as follows: (a) PTH level > 800 pg/ml; (b) diagnosis of SHPT; (c) hyperparathyroidism in at least one parathyroid gland observed via imaging; (d) ability to understand, read, and write in Chinese; and (e) voluntary participation. And the exclusion criteria was severe cardiac insufficiency and cognitive dysfunction.In all, 325 questionnaires were distributed. Of these, the forms that were missing more than 20% of values or those with low writing quality were excluded from this survey. Finally, 320 questionnaires were considered valid (effective response rate: 98.46%). The application process took place in the department where the participants were informed of the research purpose. Informed consent was obtained from all participants and anonymity confidentiality standards were assured.
Instruments
Measurement of depression: The self-rating depression scale (SDS) was used to evaluate depression by Dr W.K. Zung. This scale is comprises 20 items and 4 dimensions: psychoemotional symptoms, somatic disorders, neuromotor disorders, and psychological disorders. The SDS includes questions that help determine the degree of depression in patients using a 4-point Likert scale that ranges from 1 point (never) to 4 points (always), with the total score ranging from 20 to 80 [14]. In this study, the value of the Cronbach’s α coefficient of internal consistency for the overall scale was 0.842.
Measurement of sleep quality: We measured sleep quality using the Pittsburgh Sleep Quality Index (PSQI). This index comprises 19 items grouped into 7 dimensions (subjective sleep quality, sleep latency, sleep duration, habitual sleep efficiency, sleep disorders, sleep medication, and daytime dysfunction) graded between 0 and 3, with the total score ranging from 0 to 21; a score of ≥7 indicates sleep disorder [15]. In this study, the value of Cronbach’s α coefficient of internal consistency for the overall scale was 0.906.
Measurement of QOL: We measured QOL using the brief table of the quality of life measurement scale (QOLBREF). The QOL-BREF, a self-reported scale, has 24 items scored on a 5-point Likert-type scale ranging from 1 to 5, with the total score ranging from 16 to 80 and higher scores indicating better QOL. This index includes four dimensions: physiological, psychological, social relation, and environmental dimensions [16]. The value of the Cronbach’s α coefficient of internal consistency for the overall scale in this study was 0.857.
Statistical analysis
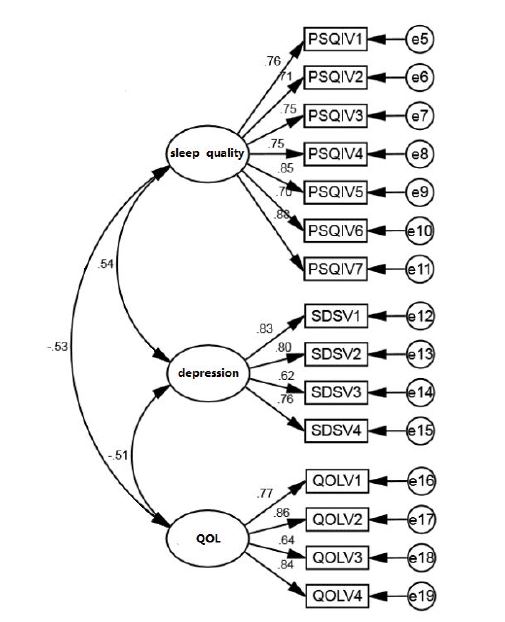
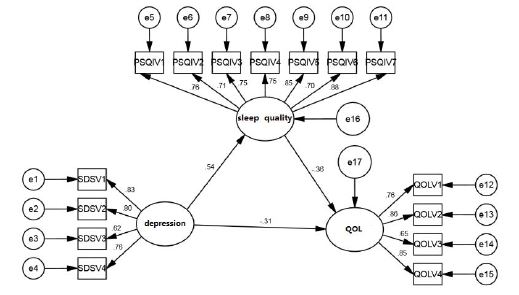
SPSS 21.0 and AMOS 23.0 were used for data entry, data cleaning, and statistical analyses. All study variables were summarized descriptively, including means and standard deviations or frequencies and percentages. Descriptive analysis, t test, variance analysis, and Pearson’s correlation analysis were used to analyze the collected data. We first performed a confirmatory factor analysis, including 3 dimensions and 15 measurement topics (Figure 1; Table 1), and examined their reliability with the Cronbach’s α coefficient. Multiple linear regression analysis was used to test the mediating effect, and the bootstrap method in the AMOS structural equation model was used to further verify the mediating effect. The initial model in this study can be divided into a structural model and a measurement model. Before building the model, the role of each variable and the relationship between variables needed to be determined via the structural model. Following this, it was necessary to measure the model and determine the relationship between each latent variable and its observation variable in advance, as shown in figure 2.
Figure 1:Confirmatory factor analysis model.
Figure 2:Mediating effect of PSQI on SDS and QOL.
Results
Demographic characteristics of participants
There were 320 patients with SHPT in this study (males: 172 (53.8%); females: 148 (46.2%)). The age of the patients ranged from 20 to 70 years. The mean duration of renal failure was 10.71±4.64 years (range: 2–30 years). The mean duration of SHPT was 3.07±2.13 years (range: 1–9 years). Descriptive statistics of the study variables are shown in table 1.
Descriptive statistics
The mean preoperative PTH level was 1729.15±376.20 pg/ml (range: 588–2934 pg/ml). The mean serum calcium level was 2.43±0.19 mmol/L (range: 1.95–2.93 mmol/L). The mean serum phosphorus level was 2.38±0.52 mmol/L (range: 1.30–3.59 mmol/L). The mean SDS score was 46.04±8.98 (range: 20–65). The mean PSQI score was 10.94±4.24 (range: 0–21). The mean QOL score was 41.76±8.15 (range: 25–68). The prevalence of depression and sleep quality was 77.81% and 78.13%, respectively. The comparative statistics for each scale in SHPT patients with different demographic characteristics are shown in table 2.
Preliminary correlation analyses
The results showed that SDS was significantly (P<0.01) positively correlated with PSQI (r=0.467) and negatively correlated with QOL (r=-0.465). Further, PSQI score was significantly (P<0.01) positively correlated with QOL (r=0.468). Pearson’s correlation analysis results for SDS score, PSQI score, and QOL are presented in table 3.
Testing for mediation effect
The variables were normalized first, and three regression equations were established based on the purpose of this study: Equation 1: QOL as the dependent variable and SDS as the independent variable; Equation 2: PSQI as the dependent variable and SDS as the independent variable; and Equation 3: QOL as the dependent variable, and SDS and PSQI as the independent variables. The results showed that SDS could significantly predict QOL (β=-0.345, P=0.000) and PSQI (β=0.125, P=0.000). When QOL was predicted based on SDS and PSQI at the same time, the predictions were significant (β=-0.234, P=0.000; β=-0.890, P=0.000). This indicated that the direct or indirect effects of SDS on QOL were significant; that is, PSQI plays an intermediary role between SDS and QOL. The results of this analysis are shown in table 4.
SEM models
Confirmatory factor analysis: Three dimensions were included in the confirmatory factor analysis: namely SDS, PSQI, and QOL. Meanwhile, 15 measurement topics were included in all (Figure 1; Tables 5 and 6).
SEM showed the following outcomes: CMIN/DF=2.558 (<3); AGFI=0.861, GFI=0.893, TLI=0.961/0.994, IFI=0.933, and CFI=0.933 (>0.8); and SRMR=0.052 and RMSEA=0.070 (<0.08), indicating that the model fit well.
The standardized factor load of each measurement index of the three dimensions was greater than 0.6, CR was 0.913, 0.841, and 0.862 (i.e., greater than 0.7), the ave was 0.6, 0.572, and 0.613 (i.e., greater than 0.5), suggesting that each variable has good convergence efficiency. The results of confirmatory factor analysis are shown in table 5.
Discriminant validity: In this study, a rigorous AVE method was used to evaluate the validity of the difference. The results showed that the AVE root number of each factor was greater than the standardized correlation coefficient outside the diagonal. The discriminant validity is shown in table 6.
Verification of the mediating effect: Based on multivariate regression analysis, the bootstrap method was used to further test the intermediary effect of PSQI scores. To test the intermediary effect, the establishment of a structural equation model was required; AMOS 23.0 was used to test the model. Figure 2 shows the specific path analysis diagram.
Table 1:Descriptive statistics of the study variables (N=320).
| Attribute | Category | N | Percentage (%) |
|---|---|---|---|
| Gender | Male | 172 | 53.8 |
| Female | 148 | 46.3 | |
| Age (years) | ≤35 | 48 | 15.0 |
| 36–50 | 115 | 35.9 | |
| 51–65 | 128 | 40.0 | |
| ≥65 | 29 | 9.1 | |
| Marital status | Married | 236 | 73.8 |
| Single | 39 | 12.2 | |
| Divorce | 35 | 10.9 | |
| Widowed | 10 | 3.1 | |
| Occupation | Cadre | 12 | 3.8 |
| Worker | 51 | 15.9 | |
| Farmer | 38 | 11.9 | |
| Retired | 87 | 27.2 | |
| Unemployed | 103 | 32.2 | |
| Other | 29 | 9.1 | |
| Education level | Primary school | 25 | 7.8 |
| Junior middle school | 162 | 50.6 | |
| High school | 77 | 24.1 | |
| College | 54 | 16.9 | |
| Master | 2 | 0.6 | |
| Income status | <1000 | 127 | 39.7 |
| 1000–3000 | 157 | 49.1 | |
| 3000–5000 | 25 | 7.8 | |
| >5000 | 11 | 3.4 | |
| Residential area | Rural | 72 | 22.5 |
| Town | 5 | 1.6 | |
| Suburb | 17 | 5.3 | |
| Urban | 226 | 70.6 | |
| Insurance | Railway | 2 | 0.6 |
| New rural | 73 | 22.8 | |
| City | 224 | 70.0 | |
| Provincial | 12 | 3.8 | |
| Own | 9 | 2.8 |
Table 2:Descriptive statistics (N=320).
| Variable | SDS | PSQI | QOL | |||
|---|---|---|---|---|---|---|
| t/F | P | t/F | P | t/F | P | |
| Gender | -3.156 | 0.002 | -2.488 | 0.013 | 2.066 | 0.040 |
| Age | 2.524 | 0.058 | 1.052 | 0.370 | 1.635 | 0.181 |
| Marital status | 0.309 | 0.819 | 1.172 | 0.320 | 5.783 | 0.001 |
| Occupation | 10.076 | 0.000 | 6.021 | 0.000 | 2.339 | 0.042 |
| Education | 2.949 | 0.020 | 0.847 | 0.497 | 0.688 | 0.601 |
| Income | 5.659 | 0.001 | 1.276 | 0.282 | 2.185 | 0.090 |
| Residential area | 0.955 | 0.414 | 0.711 | 0.546 | 0.207 | 0.892 |
| Insurance | 2.884 | 0.023 | 1.252 | 0.289 | 1.866 | 0.116 |
Table 3:Correlation among the main variables (N=320).
| Variable | SDS | PSQI | QOL |
|---|---|---|---|
| SDS | 1 | ||
| PSQI | 0.467** | 1 | |
| PSQI | 0.467** | 1 | |
| QOL | -0.465** | -0.468** | 1 |
| Note:**P<0.01 | |||
Table 4:The moderating effects of PSQI.
| Equation | Dependent variable | Independent variable | β | SE | t | P |
|---|---|---|---|---|---|---|
| Equation 1 | QOL | SDS | -0.345 | 0.037 | -9.365 | 0.000 |
| Equation 2 | PSQI | SDS | 0.125 | 0.013 | 9.428 | 0.000 |
| Equation 3 | QOL | SDS | -0.234 | 0.040 | -5.914 | 0.000 |
| PSQI | -0.890 | 0.148 | -6.015 | 0.000 |
Table 5:Confirmatory factor analysis.
| Variable | Item | Factor load | CR | AVE |
|---|---|---|---|---|
| PSQI | PSQIV1 | 0.763 | 0.913 | 0.600 |
| PSQIV2 | 0.707 | |||
| PSQIV3 | 0.753 | |||
| PSQIV4 | 0.745 | |||
| PSQIV5 | 0.852 | |||
| PSQIV6 | 0.703 | |||
| PSQIV7 | 0.881 | |||
| SDS | SDSV1 | 0.83 | 0.841 | 0.572 |
| SDSV2 | 0.802 | |||
| SDSV3 | 0.617 | |||
| SDSV4 | 0.759 | |||
| QOL | QOLV1 | 0.771 | 0.862 | 0.613 |
| QOLV2 | 0.86 | |||
| QOLV3 | 0.642 | |||
| QOLV4 | 0.839 |
Table 6:Discriminant validity.
| PSQI | SDS | QOL | |
|---|---|---|---|
| PSQI | 0.775 | ||
| SDS | 0.467** | 0.756 | |
| QOL | -0.468** | -0.465** | 0.783 |
| **P<0.01 | |||
Table 7:Results for total, indirect, and direct effects of SDS on QOL with PSQI as a mediator.
| SE | Bias-corrected | Percentile | |||
|---|---|---|---|---|---|
| 95% CI | 95% CI | ||||
| Lower | Upper | Lower | Upper | ||
| Total effect | |||||
| SDS–QOL | -0.511 | -0.701 | -0.342 | -0.680 | -0.323 |
| Indirect effect | |||||
| SDS–PSQI–QOL | -0.197 | -0.345 | -0.104 | -0.331 | -0.096 |
| Direct effect | |||||
| SDS–QOL | -0.315 | -0.524 | -0.109 | -0.506 | -0.088 |
The structural equation model fit results showed the following: CMIN/DF=2.521 (<3); AGFI=0.888, GFI=0.919, TLI=0.941, IFI=0.952, and CFI=0.951 (>0.8); and SRMR=0.051 and RMSEA=0.069 (<0.08), indicating that the model fit well. The results showed that the confidence intervals for both the direct and indirect effects of SDS on QOL did not reach 0. The mediating effect model for PSQI was established, and the mediating effect was -0.197, accounting for 38.55% of the total effect (Table 7).
Next, a hypothesis test was conducted. SDS had a significant positive effect on PSQI (β=0.539, P<0.05), and the hypothesis was tenable. PSQI and SDS scores had a significant negative effect on QOL (β=-0.365, P<0.05; β=- 0.315, P<0.05, respectively), and the hypothesis was tenable. The path coefficient is shown in table 8.
Table 8:Path coefficient.
| Path | Standardization coefficient | Non standardized coefficient | SE | CR | P | Hypothesis | ||
|---|---|---|---|---|---|---|---|---|
| PSQI | <-- | SDS | 0.539 | 0.355 | 0.042 | 8.363 | *** | Tenable |
| QOL | <-- | PSQI | -0.365 | -1.131 | 0.215 | -5.25 | *** | Tenable |
| QOL | <-- | SDS | -0.315 | -0.642 | 0.143 | -4.487 | *** | Tenable |
Discussion
The present study found that 77.81% patients with SHPT have depressive symptoms and 78.13% have sleep disorders, which were significantly higher percentages than the norm for other disease [17]. Most of SHPT patients in this sample (60.94%) slept between 3 to 4.5 hours, which is a lower duration than that recommended by WHO. The variation in prevalence may be attributed to a number of factors including differences in disease, severity of disease, basic health level, illness duration, economic situation, and screening instruments used [18]. In addition, a vast majority of SHPT patients have skin pruritus, bone pain, and electrolyte disorder coupled with long-term dialysis, leading to disturbances of various bodily systems, such as sleep disturbances, fatigue, loss of energy, and poor appetite, complicating the screening process [19,20]. Our results suggested that a large proportion of patients with SHPT had depression and sleep disorder, which would lead to poor QOL, influence prognosis, delay discharge, increase the incidence rate of acute heart failure, and increase perioperative mortality. This highlights the importance of timely recognition and effective management of depression and sleep disorders [21].
There were significant differences in the SDS score among patients with different genders, occupations, income statuses and insurances. This may be because most male patients are unable to work because of hemodialysis and are under more pressure; this finding in our study was consistent with the results reported by Marlous [22]. PSQI scores were significant different among SHPT patients with different genders and occupations; this may be associated with the perception of low probability of achieving life goals that are meaningful to an individual. The QOL significantly differed among SHPT patients with different genders, marital statuses, and occupations, which may be because the patients with a good job and high social status generally receive good dialysis equipment and are administered cinacalcet and lanthanum carbonate to alleviate SHPT.
The result of Pearson’s correlation analysis showed that SDS, PSQI, and QOL were significantly correlated with each other. This was consistent with the results obtained by Brandolim et al. and laid the foundation for subsequent analyses of mediating effects [23]. The present study aimed to conform whether sleep quality mediates the relationship between depression and the QOL among patients with SHPT.
The results of confirmatory factor analysis showed that each variable has good convergence and differentiation validity, and the initial model was established to lay the foundation for further empirical verification of intermediary effect. This study presented novel findings concerning the protective role of QOL for depression among patients with SHPT and explained how sleep quality worked as a mediator. To the best of our knowledge, this is the first study evaluating the mediating role of sleep quality between depression and QOL in SHPT patients. The SEM used in this study demonstrated that PSQI was capable of mediating the relationship between SDS and QOL. Accordingly, Liu et al. showed that sleep disorder has been observed to have a longterm negative impact on the physical, mental, emotional, and social life domains [24]. Regression analysis showed that depression had a negative predictive effect on QOL, that is, the higher the SDS score, the poorer the QOL, which was the same as that reported by Kim [25]. Consistently, previous studies have demonstrated that QOL and sleep quality were predictors of depression [26]. A longitudinal study including outpatients with chronic renal failure reported that lower baseline sleep quality was associated with greater increases in depression over time [27].
Limitations
This study presented a major limitation with regard to sample size. First, brain structure changes in long-term dialysis patients and whether such changes cause depression and sleep disorders temporarily were unknown. Second, this study included a relatively small cohort (320 patients with SHPT), and consequently this specific group may be underrepresented, limiting the generalizability of the findings. Further, the number of total parathyroidectomy patients was less. We can form a national Multi Center Alliance to solve this problem. Third, this was a cross-sectional study; a longitudinal study should be conducted on this topic in the future.
Conclusions and Recommendations
Sleep quality is suggested to be an intermediary variable that can alleviate the effect of depression on QOL. Our findings indicate that detection and management of depression and treating sleep disorders should be a part of the comprehensive approach for treating patients with SHPT. Medical staff should guide family members to actively participate in all aspects of the patients’ life and treatment, grasp the psychological function of patients in a timely manner, and improve patient care. Encouraging patients to participate in more social activities can buffer the negative effects of various pressures on the body and mind, improve sleep quality, and reduce depression and other psychological disorders. Measures such as setting up Wechat groups for SHPT patients for answering their medical problems and concerns (e.g., concerns about adjusting blood calcium levels) online after discharge and ensuring regular follow-up within the group should be undertaken. The department should carry out the corresponding mental health surveys regularly and undertake timely interventions in patients with severe pain, pruritus, sleep disorders, and depression tendency, and take positive and effective measures to improve mental health in time.
Disclosure Statement
No potential conflicts of interest were reported by the authors.
Funding
This study was supported by the Foundation for Guidance plan of Liaoning Natural Science.
Michael P, Paul Dennis M (2020) Current Understanding of Mineral and Bone Disorders of Chronic Kidney Disease and the Scientific Grounds on the Use of Exogenous Parathyroid Hormone in Its Management. J Bone Metab 27: 1-13. [ Ref ]
Bao-Shan Z, Jia-Shuo L, Li Hong (2020) Clinical study on the status of transient thyrotoxicosis after surgery for secondary hyperparathyroidism patients with end-stage renal disease and normal thyroid function. Eur J Med Res 25: 7-12. [ Ref ]
Josep D, Alicia M (2020) Epidemiology and management of parathyroid gland disorders in Spain over 15 years: A retrospective multicentre analysis. PLoS ONE 15: 1-10. [ Ref ]
Mariadelina S, Alessandra FP, Giorgio F (2020) Secondary Hyperparathyroidism and Hypertension: An Intriguing Couple. J Clin Med 9: 62-69. [ Ref ]
Thadhani Ravi I, Rosen Sophia, Ofsthun Norma J (2020) Conversion from Intravenous Vitamin D Analogs to Oral Calcitriol in Patients Receiving Maintenance Hemodialysis. Clin J Am Soc Nephrol 15: 384-391. [ Ref ]
Claudia B, Tatjana S, Dobrindt Eva M (2020) Is There a Gender Difference in Clinical Presentation of Renal Hyperparathyroidism and Outcome after Parathyroidectomy?. Visc Med 36: 34-40. [ Ref ]
Alexander Melannie, Ray Meredith A, Hébert James R (2016) The National Veteran Sleep Disorder Study: Descriptive Epidemiology and Secular Trends, 2000-2010. Sleep 39: 1399-1410. [ Ref ]
Han Jin P, P Min Seok K, Eun-Cheol P (2018) Association between sleep disorder and panic disorder in South Korea: Nationwide nested casecontrol study of data from 2004 to 2013. Psychiatry Res 260: 286-291. [ Ref ]
Michal K, Gal S, Avi S (2013) Sleep and emotions: bidirectional links and underlying mechanisms. Int J Psychophysiol 89: 21-28. [ Ref ]
Kaufmann Christopher N, Susukida Ryoko, Depp Colin A (2017) Sleep apnea, psychopathology, and mental health care. Sleep Health 3: 244-249. [ Ref ]
Naz Marzieh SG, Fahimeh RT, Tahereh BL (2020) Quality of Life and Emotional States of Depression, Anxiety and Stress in Adolescents with Polycystic Ovary Syndrome: A Cross-Sectional Study. Psychol Res Behav Manag 13: 203-209. [ Ref ]
Markarian Shaunt A, Pickett Scott M, Deveson Danielle F (2013) A model of BIS/BAS sensitivity, emotion regulation difficulties, and depression, anxiety, and stress symptoms in relation to sleep quality. Psychiatry Res 210: 281-287. [ Ref ]
Zhang Yuan, Peters Anya, Bradstreet Joseph (2018) Relationships among sleep quality, coping styles, and depressive symptoms among college nursing students: A multiple mediator model. J Prof Nurs 34: 320-325. [ Ref ]
Tuithof Marlous, Ten Have Margreet, van Dorsselaer Saskia (2018) Course of subthreshold depression into a depressive disorder and its risk factors. J Affect Disord 241: 206-215. [ Ref ]
Pui Hang CE, Yuk Fai WE, Yan Yan KJ (2019) The mediating role of sleep quality in the association between nocturia and health-related quality of life. Health Qual Life Outcomes 17: 181-190. [ Ref ]
Luigi G, Rosangela C, Da Ronch Chiara (2020) Quality of life, level of functioning, and its relationship with mental and physical disorders in the elderly: results from the MentDis_ICF65+ study. Health Qual Life Outcomes 18: 61-73. [ Ref ]
Tang Nicole KY, Mark F, Afolalu Esther F (2017) Changes in Sleep Duration, Quality, and Medication Use Are Prospectively Associated With Health and Well-being: Analysis of the UK Household Longitudinal Study. Sleep 40: 79-89. [ Ref ]
Bei B, Rachel M, Nicholas AB (2017) Too Long, Too Short, or Too Variable? Sleep Intra individual Variability and Its Associations with Perceived Sleep Quality and Mood in Adolescents during Naturalistically Unconstrained Sleep. Sleep 40: 67-75. [ Ref ]
Qiang M, Dechun S, Fen L (2020) Parathyroidectomy Influences Coronary Artery Calcium Score in Asymptomatic Hemodialysis Patients with Secondary Hyperparathyroidism. Am J Nephrol 51: 65-73. [ Ref ]
Dieter H, Maren LN (2020) Treatment of hyperphosphatemia: the dangers of aiming for normal PTH levels. Pediatr Nephrol 35: 485-491. [ Ref ]
Jacques R, Pablo UT, Daniel T (2019) Factors associated with parathyroid hormone control in haemodialysis patients with secondary hyperparathyroidism treated with cinacalcet in real-world clinical practice: Mimosa study. Clin Kidney J 12: 871-879. [ Ref ]
Marlous T, Ten Have Margreet, van Dorsselaer Saskia (2018) Course of subthreshold depression into a depressive disorder and its risk factors. J Affect Disord 241: 206-215. [ Ref ]
Nathália BB, Saul Neves de J, Viseu João N (2018) Depression and quality of life in older adults: Mediation effect of sleep quality. Int J Clin Health Psychol 18: 8-17. [ Ref ]
Yongchuang L, Tiantian L, Ruixue Z (2018) Poor sleep quality and late-life depression among the elderly in urban communities in liaoning, China: A moderated mediation analysis. Arch Gerontol Geriatr 79: 158-163. [ Ref ]
Do Hyoung K, KJi In P, Jung Pyo L (2020) The effects of vascular access types on the survival and quality of life and depression in the incident hemodialysis patients. Ren Fail 42: 30-39. [ Ref ]
Avşar U, Avşar UZ, Cansever Z (2015) Caregiver Burden, Anxiety, Depression, and Sleep Quality Differences in Caregivers of Hemodialysis Patients Compared With Renal Transplant Patients. Transplant. Proc 47: 1388-1347. [ Ref ]
Ting B, Huijun Z (2017) Mediating effect of quality of life on pain and anxiety in middle-aged and elderly glaucoma patients. China public health 33: 509-512. [ Ref ]