Journal Name: Journal of Health Science and Development
Article Type: Analysis
Received date: 28 April, 2021
Accepted date: 23 June, 2021
Published date: 2024-02-01
Citation: Ugarte S, Castillo F, Arellano-Pérez Ó (2021) Is it Safe to Use a Single Ventilator for Two or More Patients? An Evaluation of the Technical Performance of the Ventilator. J Health Sci Dev Vol: 4, Issu: 1 (21-23).
Copyright: © 2021 Ugarte S. et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Mechanical ventilation is essential in the SARS-CoV-2 pandemic context. Considering the limited availability of mechanical ventilators due to high costs increased by global demand, the use of a single ventilator for two or more patients has been encouraged. An experimental model that ventilates two test lungs with a single machine has been designed in order to measure possible asymmetries during parallel circuit ventilation under different lung compliance conditions. This paper reports a new version of assessment of the risks involved in ventilating two patients with a single machine. Since some volumetric differences are not monitored by the ventilator itself, the main risks involved are distension or alveolar collapse if used in actual patients that have different thora copulmonary mechanics.
Keywords:
Mechanical ventilation, Lungs, SARS-CoV-2, Pandemic.
Abstract
Mechanical ventilation is essential in the SARS-CoV-2 pandemic context. Considering the limited availability of mechanical ventilators due to high costs increased by global demand, the use of a single ventilator for two or more patients has been encouraged. An experimental model that ventilates two test lungs with a single machine has been designed in order to measure possible asymmetries during parallel circuit ventilation under different lung compliance conditions. This paper reports a new version of assessment of the risks involved in ventilating two patients with a single machine. Since some volumetric differences are not monitored by the ventilator itself, the main risks involved are distension or alveolar collapse if used in actual patients that have different thora copulmonary mechanics.
Keywords:
Mechanical ventilation, Lungs, SARS-CoV-2, Pandemic.
Introduction
The SARS-CoV-2 pandemic has impacted health systems with an exponential increase in bed, professional and intensive care system demands [1]. Mechanical ventilation is essential in the case of patients suffering from severe respiratory failure that require hospitalization in intensive care units (ICUs). Considering the limited availability of mechanical ventilators due to high costs, increased by global demand and based on experiences in Italy and Spain, sharing a single mechanical ventilator with two or more patients has been encouraged [2,3].
Currently, several Scientific Societies have released statements warning about the potential dangers of this strategy. Neyman’s report describes that a single ventilator may be quickly modified to ventilate four test lungs for a limited time, and the volumes delivered in this simulation should be able to sustain four 70-kg individuals [2,4]. Technically, two ventilator circuits can be connected in parallel to one ventilator by adding T-connectors to the inspiratory and expiratory limbs, However, their assessment is that ventilators might not be able to go beyond their initial automatic tube compensation, and volumes delivered would go to lung segments with increased compliance [5]. PEEP could not be screened individually, pressure and volume monitoring would display the average of both patients, and each patient’s deterioration and/ or recovery could occur in different time frames, among several other limitations [5-8]. There is no capacity to safely and effectively control the ventilatory parameters for each patient, as the distribution of tidal volume between the two or more patients is dependent on the characteristics of each patient’s lungs [6]. Another study demonstrated that a single ventilator to support more patients is possible, but that tidal volume cannot be controlled for each subject and depends on inspiratory resistances [5].
Table 1:Comparison of two test lungs without a restrictive component or increase of elasticity (CTL) and then with one lung with a restrictive component or increase of elasticity (ITL), in volume and pressure-controlled modes.
| AC/VC (tidal volume programed 900 ml, 20 breaths per minute, PEEP 8 cmH2O) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Minute ventilation ml/min | Tidal volume exhaled (ml) | Pressure (cmH2O) | ||||||||
| Pre test | SD | Post test | SD | Pre test | Post test | Pre test | SD | Post test | SD | |
| Control test lung (CTL) | 8540 | ±77.9 | 12902 | ±41.5 | 427 | 645.1 | 24 | ±0.5 | 47 | ±0,7 |
| Intenventional test lug (ITL) | 9598 | ±78.9 | 4774 | ±409.7 | 478.4 | 238.7 | 24 | ±0.5 | 47 | ±1.2 |
| AC/PC (Inspiratory pressure of 20 cmH2O, 20 breaths per minute, PEEP 8 cmH2O) | ||||||||||
| Minute ventilation ml/min | Tidal volume exhaled (ml) | Pressure (cmH2O) | ||||||||
| Pre test | SD | Post test | SD | Pre test | Post test | Pre test | SD | Post test | SD | |
| Control test lung (CTL) | 10164 | ±5.5 | 10468 | ±494.1 | ±508.2 | 523.4 | 28.4 | ±0.9 | 27.6 | ±0.5 |
| Intenventional test lug (ITL) | 10562 | ±8.4 | 780 | ±50 | ±528.1 | 39 | 28.6 | ±0.5 | 27.4 | ±0.5 |
| AC/VC: volume-controlled assisted modality; AC/PC: pressure-controlled assisted modality; SD: standard deviation. | ||||||||||
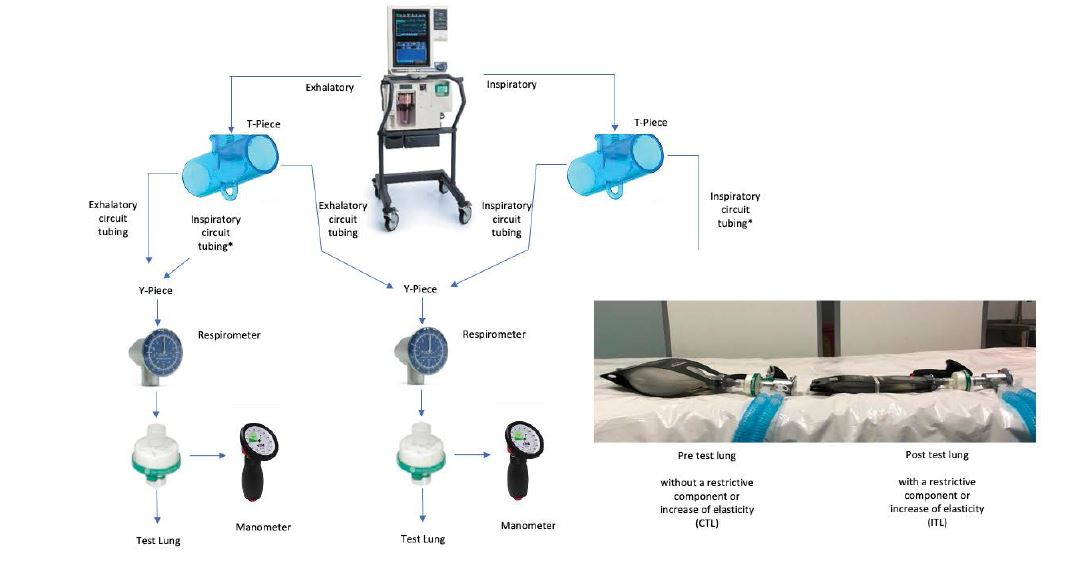
Diagram of the arrangement of the measuring instruments. A Puritan Bennett 840 (Covidien IIc, USA) mechanical ventilator was used, with two test lungs, two pressure gauges and two respirometers proximal to the test lungs, and 2 Disposable Ventilator Breathing Circuit Corrugated Tubes.
Since March 16th, Chile has entered phase 4 of the pandemic [9]. In this scenario, an experimental model has been designed to study ventilation on two test lungs with a single machine to measure possible asymmetries during parallel circuit ventilation in the case of different lung compliance.
Method
A Puritan Bennett 840 (Covidien IIc, USA) mechanical ventilator was used, with two EasyLungTM test lungs (Imtmedical, Switzerland), each holding a compliance of 25 ml/mbar and a maximum volume of 1000 ml, 2 respirometers (Wright Haloscale, Spire), 2 pressure gauges (VBM), and 2 Disposable Ventilator Breathing Circuit Corrugated Tubes. External elastic bands were used on test lungs to increase elasticity (described in the results as post test). Ten measurements were taken on each condition; first with 2 lungs without a restrictive component or with no increase of elasticity (CTL), described in the results as pre test, and then with one lung with a restrictive component or increase of elasticity (ITL), in volume and pressure-controlled modes. Tidal volume, maximum pressure and minute volume were measured (Table 1). The analysis was carried out using student’s t-test to determine differences between pressurecontrolled and volume-controlled modes, and between the control test lung (CTL) and the interventional test lung (ITL). Significance level was greater than 0.0001.
Results
Ventilator automatic tube compensation (ATC) was performed to evaluate pressurization and compliance of two parallel connected circuits. The test was successful.
Distensibility decrease in one of the test lungs (under identical basal conditions) ensued a smaller volume delivery than the one its counterpart achieved in volumecontrolled mode (p <0,0001) and pressure-controlled mode (p <0,0001), while this difference was greater in pressurecontrolled mode (Figure 1). System pressure increased on both circuits in volume-controlled mode. Maximum pressure difference between test lungs was not significant in either volume-controlled assisted modality (p >0.9999) nor pressure-controlled assisted modality (p: 0.1679).
Discussion and Conclusion
In the situation where the demand exceeds the supply and there are not enough ventilators, one might expect that the lack of ventilators would immediately and inevitably increase the mortality [6]. This report is an attempt to approach the risks of ventilating two patients with a single machine and to determine if this option should be considered or not in the ongoing pandemic situation. Tidal volumes, pressures and flows were initially similar in both modes, however, by adding a restrictive element to one of the test lungs, we proved that volumes delivered to them were different, and that maximum pressure increased in the volume-controlled mode. Regarding this, Laffeay describes in his report that pressure-controlled modes are implemented more safely because changes in the compliance, resistance, or both in one patient’s chest will have a smaller effect on the tidal volume delivered to the other patient when a fixed inflation pressure is provided [7]. Another study demonstrated that when a single ventilator is used to support more patients, tidal volume cannot be controlled for each subject and it depends on inspiratory resistances [6]. Our result coincides with what is described in the literature, considering that the method to replicate ventilation for two patients is the same, and taking into account that the brand and model of ventilator varies, the programming of mechanical ventilation and the variables measured may have some variation. Since certain differences in volumes are not monitored by the ventilator, there are risks of distension or alveolar collapse if a single machine is used in actual patients with different thoraco pulmonary mechanics [2,10].
Kallet R, Robinson L (2020) Resources. SARS CoV-2, Guidance Document. AARC. [ Ref ]
SCCM (2020) Consensus Statement on Multiple Patients Per Ventilator. Society of Critical Care Medicine (SCCM). [ Ref ]
University of Vermont. PulmCrit - Splitting ventilators to provide titrated support to a large group of patients. EMCrit Project. [ Ref ]
Neyman G, Irvin CB (2006) A single ventilator for multiple simulated patients to meet disaster surge. Academic emergency medicine : official journal of the Society for Academic Emergency Medicine 13: 1246-1249. [ Ref ]
de Jongh F, de Vries HJ, Warnaar R, Oppersma E, Verdaasdonk R, et al. (2020) Ventilating two patients with one ventilator: technical setup and laboratory testing. ERJ open research 6: 00256-2020. [ Ref ]
Laffey JG, Chikhani M, Bates DG, Hardman JG (2020) Supporting more than one patient with a single mechanical ventilator: useful last resort or unjustifiable risk?. British journal of anaesthesia 125: 247-250. [ Ref ]
Tonetti T, Zanella A, Pizzilli G (2020) One ventilator for two patients: feasibility and considerations of a last resort solution in case of equipment shortage. Thorax 75: 517-519. [ Ref ]
Petersen LG, Friend J, Merritt S (2020) Single ventilator for multiple patients during COVID19 surge: matching and balancing patients. Crit Care 24: 357. [ Ref ]
Coronavirus en Chile pasa a fase 4 y Presidente anuncia cierre de fronteras. Ministerio de Salud – Gobierno de Chile. [ Ref ]
COVID-19 en España: la presión en las UCI, principal reto en un contexto de posible cambio de tendencia en los contagios. Medscape. [ Ref ]