Journal Name: Journal of Health Science and Development
Article Type: Research
Received date: 27 Febuary, 2018
Accepted date: 21 March, 2018
Published date: 23 March, 2018
Citation: Joseph Eldor, Pham V, Tran TP, Nguyen XL, Kien NT, et al. (2018) Local Anesthesia Reversal (LAR) of Total Spinal Anesthesia (TSA) by Lipofundin (Lipid Emulsion). Jor Health Sci Development Vol: 1, Issu: 1 (67-72).
Copyright: © 2018 Joseph Eldor, et al. This is an openaccess article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
These 3 case reports are the first reports in the medical literature regarding the Local Anesthesia Reversal (LAR) of Total Spinal Anesthesia (TSA) by Lipofundin which is similar to Intralipid having soybean oil fatty acids including Linoleic acid.
Keywords:
Local anesthesia reversal (LAR), Total spinal anesthesia (TSA), Lipofundin; Intralipid; Linoleic acid.
Abstract
These 3 case reports are the first reports in the medical literature regarding the Local Anesthesia Reversal (LAR) of Total Spinal Anesthesia (TSA) by Lipofundin which is similar to Intralipid having soybean oil fatty acids including Linoleic acid.
Keywords:
Local anesthesia reversal (LAR), Total spinal anesthesia (TSA), Lipofundin; Intralipid; Linoleic acid.
Case Report 1
A 22 years old, 158 cm of height, 40 kg weight, female, was under Spinal Anesthesia for tibia reconstruction on the right leg. Past medical history was normal. The patient had a right tibia fracture, scheduled for tibia fixation.
Spinal Anesthesia (SA) was performed at L3-4, with Bupivacaine 0.5% hyperbaric. No sedation was given. Baseline BP 126/83 mmHg, HR 90, SpO2 100% (nasal oxygenation 3l/min). SA technique was uneventful and skin incision initiated.
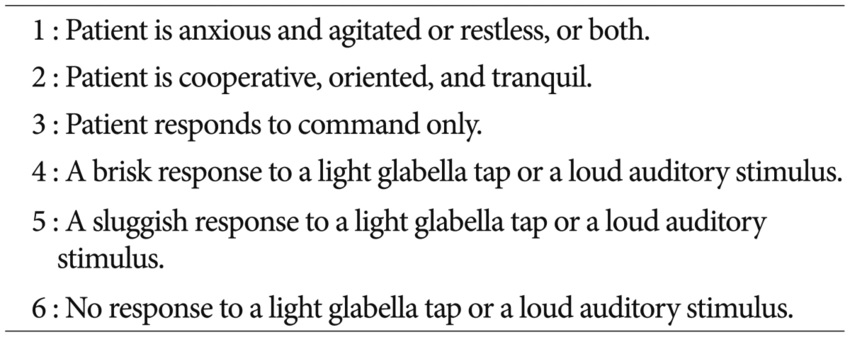
Approximately 5 mins after SA, patient experienced nausea, BP decreased to 90/50, HR 90. The patient got acceleration of 500 ml Crystalloid I.V. 10 min after SA, the patientʼs consciousness was confused, nausea, (Ramsay Score 1), BP 110/80 mmHg, HR 88, SpO2 98%. 20 Min after SA, patient was in a total coma state (Ramsay Score 6), iris was bilaterally small, BP 89/77, SpO2 98%.
(However, while asking and receiving the permission of the patient to include her videos in the article including her face (a signed permission) that was done a few days later, the patient told us that “In fact she was in the “locking syndrome” in which she heard, understood everything that was happening, but could not open her eyes nor talk (as the situation under muscle relaxant without enough sedative in general anesthesia). After the first bolus of Lipofundin she was awake nearly completely, but after that returned to the previous situation. After the second bolus, she felt much better and could respond to open her eyes as described in the report”.)
The anesthesiologist decided to give 250 ml of Lipofundin 20%. After 60 ml bolus dose, the patient opened her eyes to demand (Ramsay Score 3), but felt tired, nausea, difficult to breath, otherwise hemodynamically was stable (BP 103/74, HR 88, SpO2 98%), Pinprick test lost at neck and upper extremities (C4-5).
Another 60 ml bolus of Lipofundin 20% was added. The patient opened her eyes spontaneously (Ramsay Score 2) for a while, then stayed at Ramsay score 4. Other vital signs were stable: BP 120/77, HR 76, Spontaneous breathing with SpO2 98%. The rest of Lipofundin 20% I.V continued over 30 min. During the incident, surgery was continued and lasted for 50 mins.
At the end of surgery, the Ramsay Score was 3, short of breath decreased, the pinprick test lost at T4-5, vital signs were stable (BP 120/81, HR 78, SpO2 98%) without any vasoconstricting drugs nor respiratory supports (video clip 1).
Video clip 1: https://youtu.be/JmYXsaxInak
At the recovery room, the patient received a second infusion of 250 ml vial of Lipofundin 20% over 60 mins.
At 10 min: Ramsay Score 3, Pinprick test lost at T6, Bromage Score 0, slight myoclonus on upper extremities noted, vital signs were stable (video clip 2).
Video clip 2: https://youtu.be/Jibckg-tpro
At 30 min: Ramsay Score 2, pinprick test lost at T6, Bromage Score 1. (video clip 3).
Video clip 3: https://youtu.be/UuKq5lvWVag
At 60 min: Ramsay Score 2, pinprick test lost at T7-8, Bromage Score 1- 2. (video clip 4).
Video clip 4: https://youtu.be/bQS8l1zsNUY
At 120 min: Ramsay Score 1, pinprick test lost at T 12, Bromage Score 1, no notion of any sign of myoclonus (Figure 1).
Figure 1: RAMSAY Score
Case report 2
A 28 years old, 155 cm height, 62 kg weight, healthy parturient with healthy pregnancy was scheduled for Cesarean Section for her second baby. Her previous Cesarean Section was done under Spinal anesthesia 5 years ago and was uneventfully. The laboratory tests were in normal ranges. Spinal Anesthesia was performed at L3-4 in the sitting position using Bupivacaine 10mg+Fentanyl 25 mcg+Morphine 150 mcg.
Two mins after the SA, BP decreased to 70/40, HR 120, shortness of breath, pale, SpO2 87-90%, (under oxygenation of 5L/min), the voice was lost.
She was given oxygen via mask 10L/min, 30 mg Ephedrine to recover BP, but still experienced shortness of breath and lost voice. The anesthesiologist considered these signs as LAST (Local Anesthetic Systemic Toxicity) and decided to treat the patient by LE 20% (Lipofundin 20%). After a bolus of 100 mL, the skinʼs color improved, SpO2 improved to 100%, BP was stable.
Twenty mins after the Infusion of 250 ml Lipofundin 20%, she regained the voice, no shortness of breath any more, SpO2 100%, BP stable.
The surgery was continued uneventfully for 30 mins. The Apgar score of the newborn was ok.
Case report 3
A 28 years old, 165 cm, 70 kg weight, first pregnancy, healthy, full-term parturient was indicated for a Cesarean Section because the fetal head did not descend.
The first Spinal Anesthesia (SA) was performed in the sitting position at L2-3 with a dose of 8 mg Bupivacaine 0.5 % heavy+50 mcg Fentanyl.
The first SA failed, so she was given another SA in the sitting position in the same level with a dose of 6 mg Bupivacaine 0.5 % heavy.
She was kept in head up position thereafter. Just after lying down on the table, she developed pale, severe dyspnea, BP decreased to 60/30, HR 50, SpO2<80%, sensory touch was lost at the upper extremities. The 500 ml Crystalloid infused rapidly, facial mask ventilation with Oxygen, and 30 mg Ephedrine given I.V to maintain BP (80/60 mmHg). Meanwhile the surgery initiated immediately to take out the neonate.
At this time the anesthesiologist was considering intubation, but he decided to use lipid emulsion therapy because he thought that it was LAST (Local Anesthetic Systemic Toxicity) and not a benign hypotension due to SA.
Since of LE 20% (Lipofundin 20%) was unavailable, the anesthesiologist used Lipofundin 10% instead.
After a rapid IV of 250ml of Lipofundin 10% (approximately 10 min), the parturient improved completely: full consciousness, normal spontaneous breathing, SpO2 100% with an oxygen face mask, stable BP, HR without using any vasoconstrictor, the sensory loss estimated at T4. At the end of the surgery (approx. 30 mins) the parturient returned to nearly normal state.
Discussion
Introduction
When a local anesthetic is injected multiple times into the subarachnoid space, it can lead to an extensive block, termed total spinal anesthesia (TSA). The most common cause is an accidental dural injection during an epidural anesthesia [1].
High neuraxial block is a common cause of anesthesiarelated maternal death. Two-thirds of high blocks were caused by accidental intrathecal injection through a presumed epidural catheter [2].
Typical features of TSA include fall in blood pressure, cessation of respiration, loss of consciousness and even cardiac arrest, which can occur within minutes of injecting a spinal drug [3]. Sometimes symptoms are atypical and difficult to identify [4].
The duration and severity of TSA is related to the type and dose of local anesthetic; for example, 0.75% bupivacaine was shown to have a mean duration of action of 1.5 h~3 h [5].
The study was part of the Thai Anesthesia Incidents Study (THAI Study) of anesthetic adverse outcomes. Study complications after spinal anesthesia [6].
During the 12-month period (March 1, 2003 - February 28, 2004), a prospective multi centered descriptive study was conducted in 20 hospitals comprised of seven university, five tertiary, four general and four district hospitals across Thailand. Anesthesia personnel filled up patient-related, surgical-related, and anesthesia-related variables and adverse outcomes of all consecutive patients receiving anesthesia on a structured data entry form. The data were collected during pre-anesthetic, intra-operative, and 24 hr post-operative period. Adverse event specific forms were used to record when these incidents occurred. Data were reviewed by three independent reviewers and analyzed to identify contributing factors by consensus.
This was registry of 40,271 spinal anesthetics from 172,697 anesthetics. The incidence of total spinal anesthesia, neurological complications, suspected myocardial ischemia, or infarction and oxygen desaturation per 10,000 spinal anesthetics were 3.48 (95% CI 1.66-5.30), 1.49 (95% CI 0.30- 2.68), 2.73 (95% CI 1.12-4.35), 0.99 (95% CI 0.39-2.56), and 6.46 (95% CI 3.98-8.94) respectively. This was not different to the incidence in other countries. Risk factors of oxygen desaturation were shorter in height [OR 0.95 (95% CI 0.92-0.97); p < 0.0011, higher ASA physical status [OR 3.37 (95% CI 1.98-5.72); p<0.001] and use of propofol [OR 5.22 (95% CI 1.78-15.35); p=0.003]. Other complications such as seizure, anaphylactic or anaphylactoid reaction, drug error, and pulmonary aspiration were scarce. There was no case of mismatched blood transfusion in the present study.
Incidence of total spinal block, neurological complication, and suspected myocardial ischemia or infarction was uncommon. Risk factors of oxygen destruction were shorter in height, higher ASA physical status, and use of propofol. Some events were considered avoidable and preventable [6].
Effect of TSA on the Heart and Peripheral Blood Flow
We evaluated the effect of total spinal anesthesia (TSA) on the heart rate and peripheral blood flow variations to evaluate if TSA could influence these parameters as indicators of autonomic nervous function (ANF) [7]. Four patients with intractable pain were treated by TSA by administration of local anesthetics (lidocaine or mepivacaine) into the C7- Th1 vertebral interspace. Power spectrum of heart rate before TSA showed three peaks; low (LO-FR, 0.04-0.095 Hz), mid (MID-FR, 0.095-0.15Hz) and high frequency areas (HI-FR, 0.15-0.3Hz). Spectral peaks of LO-FR and MID-FR disappeared during TSA (P less than 0.001). HI-FR area decreased to 3.3% of the control level (P less than 0.001). Mean peripheral blood flow was changed to 59.9% of the control level (not significant). However, peripheral blood flow variations of LO-FR decreased to 11.3% of the control level (P less than 0.001) after TSA. Furthermore, the vagal discharge disappeared promptly after TSA in dog. These results suggest that TSA depresses the vagal activity as well as the sympathetic activity innervating the cardiovascular system and therefore, heart rate and peripheral blood flow variations are totally eliminated. Thus, we conclude that heart rate and peripheral blood flow variations can serve as valid markers of ANF activity [7].
To test whether acute denervation alters the vascular effects of dopamine and dobutamine, we anesthetized 16 greyhounds and placed them on total cardiopulmonary bypass (CPB) [8]. Eight dogs received total spinal anesthesia before drug testing; eight dogs were tested in the absence of total spinal anesthesia. During dopamine and dobutamine infusions, venous capacitance [determined by the volume of the CPB venous reservoir (VR)] and mean arterial pressure (MAP) were monitored. The CPB pump flows remained constant throughout our studies. Every dog received six increasing doses of both drugs. In the absence of total spinal anesthesia, both dopamine and dobutamine increased VR (decreased venous capacitance) in a dosedependent manner. Dobutamine decreased MAP in a doserelated fashion but dopamine had no significant effect on MAP. After total spinal anesthesia, both dopamine and dobutamine produced greater dose-related increases in VR (i.e., decreases in venous capacitance) than in the absence of spinal anesthesia. Dopamine increased MAP but dobutamine had no significant effect. These data demonstrate how dopamine and dobutamine differ in their effects on the arterial circulation in the presence or absence of spinal anesthesia. The acute denervation of spinal anesthesia altered venous and arterial dose-response relationships of both drugs. Finally, our study demonstrates the effectiveness of dobutamine and, perhaps even more so, dopamine as possible alternatives to ephedrine for the pharmacologic correction of the noncardiac circulatory sequelae of spinal anesthesia [8].
TSA History
Evans described in 1928 the possible complications of spinal anesthesia [9]. Concerning respiratory paralysis, he wrote:” If respiration should cease, keep cool. Raise the lower jaw, pull the tongue forward and begin artificial respiration at a uniform rate. Mouth to mouth insufflation is the most convenient and efficacious method of artificial respiration”. Twenty years before, in September 1908, before the Congress of the International Society of Surgery, in Brussels, Thomas Jonnesco from Bucharest, described his new method of general spinal anesthesia and reported 14 cases operated upon by his method [10]. Bier, who 10 years ago established the first human surgical spinal anesthesia, rejected it [10]. In a later paper in 1910 Jonnesco wrote: “It is an error to confuse lumbar rachianesthesia, conceived by Corning and popularized by Bier, with my method. As I have many times emphasized, my method is a new one and altogether distinctive, because I have generalized spinal anaesthesia, adopting it to all operations on any part of the body” [11]. Patients given high spinal anesthesia frequently either lapse into what appears to be normal sleep or may actually lose consciousness [12-15]. If patients with high spinal anesthesia are given an inhalational anesthetic such as nitrous oxide-oxygen, very low concentrations of anesthetic gases are required to maintain unconsciousness [16]. Reduction in the strength of nociceptive input may contribute to loss of consciousness by diminishing the strength of arousing stimuli arriving at cortical structures [17]. Studies with C14 labeled lidocaine in dogs have shown that the foramen magnum is not a physiological barrier, for autoradiographs and tissue samples reveal the presence of radioactivity in intracranial parts of the CNS after a relatively modest epidural dose [18]. Total spinal anesthesia has been used as a method of general anesthesia for abdominal surgery [19] and for the treatment of intractable pain [20]. Gillies and Morgan described a patient in whom a total spinal anesthesia resulted after 18 ml of inadvertent subarachnoid injection of 0.5% bupivacaine [21]. Spontaneous respiration was noted 120 minutes later, and consciousness regained after further 65 minutes. Return of respiration after 17 ml 1.5% lignocaine which resulted in total spinal analgesia occurred after 45 minutes and consciousness after further 80 minutes [22]. Four patients with intractable pain were treated by total spinal anesthesia. Power spectral analysis of heart rate and peripheral blood flow variations were studied. Vagal activity was depressed as well as the sympathetic activity innervating the cardiovascular system, so the heart rate and peripheral blood flow variations were totally eliminated [23]. Total spinal block can be elicited even after an epidural test dose like the 36-year-old parturient of Palkar et al. who developed hypotension and extensive sensory and motor block including respiratory paralysis and aphonia after injection via the epidural catheter of 3 ml lidocaine 1.5% (45 mg) with 1:200,000 epinephrine (15 microgram) [24]. The patient remained fully conscious and alert and spontaneous respiration recommenced in five minutes. Three patients were studied to determine the changes in regional skin temperature and blood flow during extensive sympathetic blockade following total spinal anesthesia. The temperature of the truncal area, arm and leg decreased by 1-degree C, whereas the temperature of the hand and foot increased by 3 degrees C [25]. Total spinal block was induced by 2% lidocaine in adult mongrel dogs. Heart rate, mean arterial pressure, cardiac index and left ventricle dp/dt max decreased significantly [26]. Ephedrine 0.5 mg/Kg elevated HR, MAP, LV dp/dt max and SVR [27]. Total spinal anesthesia blocks the vagus as well as the sympathetic nervous system and decreases heart rate variation, suggesting that neural control of the heart via the autonomic nervous system is abolished after total spinal anesthesia [25]. Matsuki et al. described a patient with primary aldosteronism who was anesthetized by total spinal anesthesia using an epidural catheter inserted at L3-4 into the subarachnoid space [28].
The trachea was intubated after intravenous injection of thiopentone 250 mg and suxamethonium 40 mg, and oxygen 3 liters/minute and nitrous oxide 2 liters/minute inhaled.
The intraoperative course was smooth and intraoperative muscle relaxation excellent. Adrenaline, noradrenaline and dopamine in the plasma remained within normal ranges. Mets et al. described a case of an unplanned version of CSEGA (Combined Spinal Epidural General Anesthesia):A 24-year-old parturient received an epidural analgesia during labor [29]. Then she was scheduled for cesarean section for failure to progress. A total dose of 30 ml 0.5% bupivacaine was administered incrementally via the epidural catheter which resulted in a patchy block that was inadequate for surgery. Twenty minutes after the last injection of epidural local anesthetic a spinal anesthesia was done which resulted in a high block that necessitated tracheal intubation and ventilation. Controlled ventilation maintained with 50% N2O and 0.5% isoflurane in oxygen until delivery of the baby after which the isoflurane was stopped and 70% N2O in oxygen was administered. No further muscle relaxation was required for the remainder of the operation which lasted 45 minutes. The patient was extubated at the end of the operation uneventfully.
CSF Lavage
High or total spinal anesthesia commonly results from accidental placement of an epidural catheter in the intrathecal space with subsequent injection of excessive volumes of local anesthetic. Cerebrospinal lavage has been shown to be effective at reversing the effects of high/total spinal anesthesia but is rarely considered in obstetric cases. Here, we describe the use of cerebrospinal lavage to prevent potential complications from high/total spinal anesthesia after unintentional placement of an intrathecal catheter in a labouring obstetric patient [30].
A 34-yr-old female presented to the labour and delivery unit in active labour. Epidural anesthesia was initiated, and after the first bolus dose, the patient experienced lower extremity motor block and shortness of breath. A high spinal was confirmed, and cerebrospinal lavage was performed. In total, 40 mL of cerebrospinal fluid (CSF) were exchanged for an equal volume of normal saline. The patient’s breathing difficulties and motor block resolved quickly, and a new epidural catheter was placed after removal of the spinal catheter. Pain control was effective, and the patient delivered a healthy baby.
We show that exchange of CSF for normal saline can be used successfully to manage a high spinal in an obstetric patient. Our results suggest that CSF lavage could potentially be an important and helpful adjunct to the conventional supportive management of obstetric patients in the event of inadvertent high or total spinal anesthesia [30].
High spinal block carries significant morbidity and mortality risk. The predisposing factors are modifiable to reduce the incidence but unintentional high block secondary to migrated epidural catheter is still a possibility.
Our patient had received a combined spinal epidural anesthetic for surgery in the lithotomy position with 15 mg of 0.5% hyperbaric bupivacaine deposited intrathecally and repeated hourly boluses of 8 ml/hour of isobaric bupivacaine throughout surgery. The position of epidural catheter was confirmed with a test dose of 3ml 2% preservative free lignocaine before the first epidural injection. The last epidural medication was 0.25% bupivacaine 6ml given at the time of skin closure.
Subsequent to this injection, the patient started complaining of heaviness of breath in a low-pitched voice. His vital signs were stable (HR 92 bpm; BP 110/56 mmHg) prior to this episode. Blood pressure decreased to 85/56 mm Hg with a HR of 78 bpm. A colloid 6% HES infusion was started. The possibility of a pulmonary embolism or cranial migration of epidural drug in lithotomy position was considered. The patient could support his airway and low volume tidal breathing was observed clinically. Ventilation was gently assisted with BMV with 100% O2. The epidural catheter showed CSF on aspiration.
The technique of CSF lavage to reverse the high spinal anesthesia was employed. Slowly, CSF was removed in aliquots of 10 ml each time and replaced with 10 ml of isotonic saline. This procedure was repeated for 5 times following strict asepsis and keeping a careful watch on the patient’s haemodynamics. Prompt improvements in single breath count from 4 to 12, hand grip and end tidal capnogram of spontaneous breathing was noticed. The sensory level of analgesia regressed from T2 toT4 over 15 mins and T10 by 25 mins. He was administered iv paracetamol 1 gm and tramadol 50 mg to combat pain, which was his next complaint half an hour after CSF lavage. The spinally migrated epidural catheter was removed in lateral position and patient was monitored for next 72 hours for meningeal signs, respiratory or cardiovascular deterioration and post dural puncture headache [31].
TSA due to Intercostal Nerve Block and Interscalene Nerve Block and Cervical Epidural Block
Intercostal nerve block is a recognized way of providing analgesia at thoracotomy. There is a rare association between intercostal nerve block and the complication of total spinal anesthesia. This may arise inadvertently by injection into a dural cuff extending outside the intervertebral foramen. We report our experience with a patient who sustained this life-threatening complication [32]. The patient required postoperative ventilation until the neurologic deficits resolved. The operator must be aware that intercostal nerve block runs the rare but potentially fatal risk of total spinal block [32].
We report a catastrophic postoperative complication of a prolonged interscalene block performed under general anaesthesia [33]. The course of the anaesthetic was uneventful, and the patient remained stable during his stay in the recovery area with the operative extremity paralysed and insensate. No further local anaesthetic was administered until later that day when the patient received 10 ml bupivacaine 0.25% through the catheter. Upon completion of the top-up dose, no change in the patient’s status was noticed. The patient was next assessed 6.5 h later when he was found dead in his bed. A post-mortem CT scan revealed the catheter to be sited intrathecally, presumably the result of dural sleeve penetration [33].
We present a case of unintentional total spinal anesthesia, which occurred during cervical epidural block [34]. A 34-year-old man with complex regional pain syndrome of the right upper arm was treated with epidural block at C7-T1 interspace. Immediately after test-dose injection of ropivacaine 1.5 ml, he complained of paraesthesia of his upper extremities. He developed difficulty talking and breathing. Subsequently he showed a complete paralysis with the loss of consciousness, respiratory arrest, and bilateral mydriasis. Mandatory ventilation was started, and endotracheal tube was placed. Eighty minutes after the injection of ropivacaine, he recovered consciousness and spontaneous respiration resumed. Checking adequate ventilation, his trachea was extubated. Neurological dysfunction was not seen thereafter. Although test-dose injection is recommended especially in high-risk patients and case of difficulty of epidural space identification, it does not fully prevent complications. For cervical epidural block, local anesthetics should either be given at small doses or not be given as long as a possibility of spinal injection is remaining [34].
TSA is not LAST
Look on the following CHECKLIST FOR TREATMENT OF LOCAL ANESTHETIC SYSTEMIC TOXICITY {LAST) : https://www.asra.com/content/documents/asra_last_ checklist_2018.pdf
It is based on The Third American Society of Regional Anesthesia and Pain Medicine Practice Advisory on Local Anesthetic Systemic Toxicity . Executive Summary 2017. Reg Anesth Pain Med 2016; 43: 113-123.
Look on the second page under Risk Reduction (Be sensible):
- Second point: “ Local anesthetic blood levels are influenced by site of injection and dose”.
- Fourth point: “Aspirate the syringe prior to each injection while observing for blood in the syringe or tubing”.
In other words: LAST refers to LA>BLOOD>ST
It has nothing to do with TSA…
Of course, the LA in the blood can have “altered mental status, neurological symptoms or signs of cardiovascular instability...”
These 3 case reports are the first reports in the medical literature regarding the Local Anesthesia Reversal (LAR) of Total Spinal Anesthesia (TSA) by Lipofundin which is similar to Intralipid having soybean oil fatty acids including Linoleic acid.
Conclusion
These 3 case reports are the first reports in the medical literature regarding the Local Anesthesia Reversal ( LAR) of Total Spinal Anesthesia (TSA) by Lipofundin.
Hodgkinson R (1981) Total spinal block after epidural injection into an interspace adjacent to an inadvertent dural perforation. Anesthesiology 55: 593-595. [ Ref ]
Davies JM, Posner KL, Lee LA, Cheney FW, Domino KB (2009) Liability associated with obstetric anesthesia: a closed claims analysis. Anesthesiology 110: 131-139. [ Ref ]
Gillies ID, Morgan M (1973) Accidental total spinal analgesia with bupivacaine. Anaesthesia 28: 441-445. [ Ref ]
Siddik-Sayyid SM, Gellad PH, Aouad MT (2012) Total spinal block after spinal anesthesia following ongoing epidural analgesia for cesarean delivery. J Anesth 26: 312-313. [ Ref ]
Wilkinson GR, Lund PC (1970) Bupivacaine levels in plasma and cerebrospinal fluid following peridural administration. Anesthesiology 33: 482-486. [ Ref ]
Charuluxananan S, Thienthong S, Rungreungvanich M, Chanchayanon T, Chinachoti T, et al. (2007) The Thai Anesthesia Incidents Study (THAI study) of morbidity after spinal anesthesia: a multi-centered registry of 40,271 anesthetics. J Med Assoc Thai 90: 1150-1160. [ Ref ]
Goda Y, Kimura T, Goto Y, Kemmotsu O (1989) Power spectral analysis of heart rate and peripheral blood flow variations during total spinal anesthesia. Masui 38: 1275-1281. [ Ref ]
Butterworth JF, Austin JC, Johnson MD, Berrizbeitia LD, Dance GR, et al. Effect of total spinal anesthesia on arterial and venous responses to dopamine and dobutamine. Anesth Analg 66: 209-214. [ Ref ]
Evans CH (1928) Possible complications with spinal anesthesia. Their recognition and the measures employed to prevent and to control them. Am J Surgery 5: 581-593. [ Ref ]
Jonnesco T (1909) Remarks on general spinal analgesia. Br Med J 2: 1396-1401. [ Ref ]
Jonnesco T (1910) Concerning general rachianesthesia. Am J Surgery 24: 33. [ Ref ]
Koster H, Kasman LP (1929) Spinal anesthesia for the head, neck and thorax: its relation to respiratory paralysis. Surg Gynecol Obstet 49: 617. [ Ref ]
Vehrs GR (1934) Spinal anesthesia: Technic and clinical application. St Louis: The C.V. Mosby Co. [ Ref ]
Jones RGG (1953) A complication of epidural technique. Anaesthesia 8: 242. [ Ref ]
Huvos MC, Greene NM, Glaser GH (1962) Electroencephalographic studies during acute subtotal denervation in man. Yale J Biol Med 34: 592. [ Ref ]
Greene NM (1952) Hypotensive spinal anesthesia. Surg Gynecol Obstet 95: 331. [ Ref ]
Kendig JJ (1993) Spinal cord as a site of anesthetic action. Anesthesiology 79: 1161-1162. [ Ref ]
Bromage PR, Joyal AC, Binney JC (1963) Local anaesthetic drugs: Penetration from the spinal extradural space into the neuraxis. Science 140: 392. [ Ref ]
Evans TI (1974) Total spinal anaesthesia. Anaesth Intensive Care 2: 158-163. [ Ref ]
Yamashiro H, Hirano K (1987) Treatment with total spinal block of severe herpetic neuralgia accompanying median and ulnar nerve palsy. Masui 36: 971-975. [ Ref ]
Gillies IDS, Morgan M (1973) Accidental total spinal analgesia with bupivacaine. Anaesthesia 28: 441-445. [ Ref ]
DeSaram M (1956) Accidental total spinal analgesia. A report of three cases. Anaesthesia 11: 77. [ Ref ]
Goda Y, Kimura T, Goto Y, Kemmotsu O (1989) Power spectral analysis of heart rate and peripheral blood flow variations during total spinal anesthesia. Masui 38: 1275-1281. [ Ref ]
Palkar NV, Boudreaux RC, Mankad AV (1992) Accidental total spinal block: a complication of an epidural test dose. Can J Anaesth 39: 1058- 1060. [ Ref ]
Kimura T, Goda Y, Kemmotsu O, Shimada Y (1992) Regional differences in skin blood flow and temperature during total spinal anaesthesia. Can J Anaesth 39: 123-127. [ Ref ]
Kobori M, Negishi H, Masuda Y, Hosoyamada A (1991) Changes in respiratory, circulatory, endocrine, and metabolic systems under induced total spinal block. Masui 40: 1804-1809. [ Ref ]
Kobori M, Negishi H, Masuda Y, Hosoyamada A (1990) Changes in systemic circulation under induced total spinal block and choice of vasopressors. Masui 39: 1580-1585. [ Ref ]
Matsuki M, Muraoka M, Oyama T (1988) Total spinal anaesthesia for a Jehovah`s Witness with primary aldosteronism. Anaesthesia 43: 164- 165. [ Ref ]
Mets B, Broccoli E, Brown AR (1993) Is spinal anesthesia after failed epidural anesthesia contraindicated for cesarean section? Anesth Analg 77: 629-631. [ Ref ]
Ting HY, Tsui BC (2014) Reversal of high spinal anesthesia with cerebrospinal lavage after inadvertent intrathecal injection of local anesthetic in an obstetric patient. Can J Anaesth 61: 1004-1007. [ Ref ]
Ashima S, Kiran G, Padmaja D, Gopinath R (2014) CSF Lavage for high spinal- A technical miracle. BJA: British Journal of Anaesthesia 113. [ Ref ]
Chaudhri BB, Macfie A, Kirk AJ (2009) Inadvertent total spinal anesthesia after intercostal nerve block placement during lung resection. Ann Thorac Surg 88: 283-284. [ Ref ]
Yanovski B, Gaitini L, Volodarski D, Ben-David B (2012) Catastrophic complication of an interscalene catheter for continuous peripheral nerve blockanalgesia. Anaesthesia 67: 1166-1169. [ Ref ]
Hara K, Sata T (2006) Unintentional total spinal anesthesia during cervical epidural block with ropivacaine. Masui 55: 1168-1169. [ Ref ]