Journal Name: Journal of Multidisciplinary Research and Reviews
Article Type: Research
Received date: 19 November, 2018
Accepted date: 21 June, 2019
Published date: 28 June, 2019
Citation: Tekelehaymanot G (2019) Assessment of Quality of Antenatal Care Service Provision and Associated Factor at Governmental Health Facilities of Harar Town, Eastern Ethiopia, 2017. J Multidis Res Rev Vol: 1, Issu: 1 (46-55).
Copyright: © 2019 Tekelehaymanot G. This is an openaccess article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Background: Antenatal care is comprehensive care that pregnant women receive from organized health care services to promote and maintain optimal health of the mother throughout the pregnancy, labor and puerperium. High quality antenatal care is important to safeguard their health help women maintain normal pregnancies and reduce the rate of maternal and infant morbidity and mortality. Studies conducted to assess quality of antenatal care service which describes the components of antenatal care that the woman receive during her pregnancy and do not describe the factor that affects quality service and also, they do not illustrate the quality service. Therefore, this study tried to fill the gap which was not address by previous studies.
Objective: To assess quality of Antenatal care service and associated factors in Harar town governmental health facilities Harar, Ethiopia from January 30 to February.
Methods: Facility based cross sectional study that employed quantitative method supplemented with qualitative method was used. Exit interview was conducted on clients who had ANC follow up. Observation on the health care provider was performed while providing antenatal care. Indepth interview was conducted on one purposively selected antenatal care provider. Facility infrastructure, supplies and equipment and health care practices during Antenatal clinic was assessed. Collected and checked data were entered in to Epi Data software version 3.02 and exported and analyzed using SPSS version 21. Both Bivariate and multiple logistic regressions were used to observe the association between the outcome variable and associated factors.
Result: Among the Focused Antenatal Component personal history, Blood pressure measurement, Laboratory evaluation and provision of supply were provided for majority of the clients. The overall prevalence of quality of ANC service was 24.3%. Women who had history of still birth 2 times more likely (AOR = 2.936, 95% CI: 1.177 -7.320) Women who had more than four visit were 4.5 times more likely (AOR = 4.592, 95% CI: 1.318 - 12.996), women whose privacy maintain while counseling were 4 times more likely (AOR = 4.110, 95% CI: 1.753 -9.637) having quality of antenatal care services than their encounters.
Conclusion and Recommendation: Generally, the studies showed that majority of clients were not received quality Antenatal care service. Consultation room for keeping privacy should have to maintain for providing quality Antenatal care service by the health facilities.
Keywords
Antenatal care, Quality antenatal care, Quality.
Abstract
Background: Antenatal care is comprehensive care that pregnant women receive from organized health care services to promote and maintain optimal health of the mother throughout the pregnancy, labor and puerperium. High quality antenatal care is important to safeguard their health help women maintain normal pregnancies and reduce the rate of maternal and infant morbidity and mortality. Studies conducted to assess quality of antenatal care service which describes the components of antenatal care that the woman receive during her pregnancy and do not describe the factor that affects quality service and also, they do not illustrate the quality service. Therefore, this study tried to fill the gap which was not address by previous studies.
Objective: To assess quality of Antenatal care service and associated factors in Harar town governmental health facilities Harar, Ethiopia from January 30 to February.
Methods: Facility based cross sectional study that employed quantitative method supplemented with qualitative method was used. Exit interview was conducted on clients who had ANC follow up. Observation on the health care provider was performed while providing antenatal care. Indepth interview was conducted on one purposively selected antenatal care provider. Facility infrastructure, supplies and equipment and health care practices during Antenatal clinic was assessed. Collected and checked data were entered in to Epi Data software version 3.02 and exported and analyzed using SPSS version 21. Both Bivariate and multiple logistic regressions were used to observe the association between the outcome variable and associated factors.
Result: Among the Focused Antenatal Component personal history, Blood pressure measurement, Laboratory evaluation and provision of supply were provided for majority of the clients. The overall prevalence of quality of ANC service was 24.3%. Women who had history of still birth 2 times more likely (AOR = 2.936, 95% CI: 1.177 -7.320) Women who had more than four visit were 4.5 times more likely (AOR = 4.592, 95% CI: 1.318 - 12.996), women whose privacy maintain while counseling were 4 times more likely (AOR = 4.110, 95% CI: 1.753 -9.637) having quality of antenatal care services than their encounters.
Conclusion and Recommendation: Generally, the studies showed that majority of clients were not received quality Antenatal care service. Consultation room for keeping privacy should have to maintain for providing quality Antenatal care service by the health facilities.
Keywords
Antenatal care, Quality antenatal care, Quality.
Introduction
Background: Roemer and Anguilar, defined quality as “…proper performance (according to standards) of interventions that are known to be safe, that are affordable to the society in question, and the ability to produce an impact on mortality, morbidity, disability, and malnutrition [1]. Quality care includes efficiency, efficacy, effectiveness, equity, accessibility, comprehensiveness, acceptability, timeliness appropriateness, continuity, privacy and confidentiality [2] Antenatal care is a goal-oriented antenatal care approach and Quality of ANC implies when the care meets the standards of ANC set by the country [3]. High quality antenatal care is important to safeguard women’s health and helps women to maintain normal pregnancies and reduce the rate of maternal morbidity and mortality [4].
Statement of the problem: Globally, by the end of 2015 an estimated 303,000 maternal deaths occurred from pregnancy- or childbirth-related complications among developing regions account for approximately 99% (302 000) of the estimated global maternal deaths. Sub-Saharan Africa alone accounting for roughly 66% (201 000), followed by Southern Asia 66 000 [5]. Antenatal care services in developing countries can have only limited impact on reducing maternal mortality because most of the major causes of maternal mortality in developing country cannot be detected during antenatal period due to less quality of screening and antenatal care service [6]. Poor antenatal care is considered the second most important preventable factor in maternal mortality after substandard obstetric care [7] Few studies conducted to assess quality of service in different area including Ethiopia describe the components of FANC service that the women received during her pregnancy follow up period [8-13]. There for this study was fill the gap which was not address by other researchers
Objectives General
Objective: To assess quality of ANC service provision and associated factors at governmental health facilities of Harar town, eastern Ethiopia from January 30 to February 24, 2017.
Specific Objectives
- To assess level of quality of antenatal care service provided to the pregnant women in Harar town governmental health facilities.
- To identify associated factors with quality antenatal care services in Harar town governmental health facilities.
Methods
Study Area and Study Period: This study was conducted in Harar Town from January 30 to February 24, 2017. There were 20 health posts, 8 health centers and 7 Hospitals, 18 Private for profit clinics, 25 pharmaceutical retails out let, 3 pharmaceutical whole sellers and 2 modern laboratories are available. The study was conducted in 2 Health center and 2 hospitals namely Jenilla and Aratena Health center and Jugal and Hiwot Fana Specialized university hospital of Harar town.
Study Design: Cross-sectional health facility based quantitative supplemented with qualitative method was used.
Source population: All Pregnant women who were taking Antenatal care
For observational part - All Health professional providing antenatal services in MCH unit of governmental Health facilities.
Study population: All antenatal care service users at selected governmental health facilities. Health care providers who are providing Antenatal care service during data collection period. For In-depth interview - One purposively selected providers who have more experience and providing ANC services was interviewed.
Sample size: sample size was determined by the formula of single (P = Proportion of Overall quality of ANC service at Jimma study 66.8%) [14] and double population proportion formula (P1 = 14.6 % and P 2 = 32.6%, 95%, margin of error of 5 % and power of 80%, and using Open Epi Info 7) [15] then comparing the first and second objective, the final sample size was 375.
Sampling procedure: Four governmental Health institutions were included. Sample was allocated proportionately based on their annually patient flow. Individual study subjects at each health facility were selected by systematic random sampling.
Variables of the study
Dependent Variable: Quality Antenatal care service
Independent Variables: Socio-demographic: Age,
Educational status, Ethnicity, Religion, Marital Status,
Occupation, Monthly income,
Client’s characteristics: satisfaction with the care and information given, frequency of ANC Visit Provider’s
characteristics: sex of provide, Weighting time, behavior, Year of service, and respecting the clients, Privacy During consultation, Duration of consultation time
Institution: Availability of Resource, logistic and supply
Service provided: History taking, physical examination, laboratory evaluation, provision of supply to the women, Information provision and advice on danger sign
Data Collection Tolls & Method: pre-tested questionnaire of both open and close-ended and open-ended interview guide and observation checklists were used. Exit interview was conducted on randomly selected clients who had ANC follow up. Health care provider was observed while providing antenatal care. In-depth interview was conducted on one purposively selected antenatal care provider. Infrastructures of the selected health facilities were observed.
Data Quality Control: to assure the quality of the data, properly design data collection instrument was developed and pretest was conducted questionnaires were translated into Amharic and Oromiffa language. Training was given for data collector’s supervisor and data entry clerks prior to the study. Every day, the collected data were reviewed for completeness, consistency and legibility. Supervision was frequently made by 8 supervisors together with the principal investigator
Data Processing and analysis: Epi-Data version 3.1 and SPSS version 21 were used for data entry and analysis. The univariate analysis such as proportions, percentages, ratios, frequency distributions and appropriate graphic presentations as well as measures of central tendency and measures of dispersion were made. Multiple logistic regression analysis were used for better prediction of determinants and to reduce bias due to confounders. Those variables with P- valueless than 0.2 were entered in to multiple logistic regression analysis. Associations with P - value less than 0.05 was declared as statistically significant
Ethical consideration: Ethical clearance was obtained from Haramaya University College of Health Science and the Institution Research Ethics Review Committee. Permission was obtained from study institution. All the participants were informed the purpose, advantages and disadvantages, there have the right to be involved or not. Informed and written consent was obtained from all participants. Confidentiality was maintained by avoiding names and other personal identification.
Operational Definitions:
- Quality antenatal care: - when clients get the component of antenatal care service, health care system has necessary and enough equipment and had qualified staffs that treat the client respectfully [13].
- Good quality – if the health institution provide ≥ 75% the necessary FANC content of services, provide education on danger sign, orient on birth preparedness, provide basic preventive and therapeutic care [14].
- Poor Quality: if the health institution provide ≤ 74% the necessary FANC services, not provide education on danger sign, orient on birth preparedness, did not provide basic preventive and therapeutic care [14].
- General examination: - includes examination of the skin, conjunctiva thyroid mouth and breast, Leg for edema, redness and varicose, and examined both fetal and maternal condition [13,15].
- Basic diagnostic service: - If health facilities perform diagnostic service for antenatal care (pregnancy test, Hg, or HCT, HIV test, urine for; sugar and albumin and vital sign equipment’s [13,15].
- Information received: - Means when a woman received information on danger sign, birth preparedness, Nutrition, Rest and exercise, Breast feeding, Birth spacing, place of birth [15].
Results
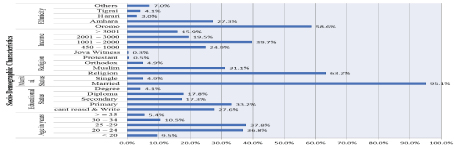
From 375 subjects enrolled, 370 women were interviewed which makes response rate 98.7%. Ages of the respondent range from 18 to 45 years. One third (33.2%) of the clients had attended primary school. Majorities (95.1%) of the clients were married. Of the total clients 63.2 % were Muslims. Almost half (50.8%) was house wives. The mean (± SD) of the average monthly income of the clients was 2308.58 ±1469.560 ranging from 500 to 9502 ETB. More than half of the respondent ethnic groups (58.6%) were Oromo followed by Amhara (27.3%) (Figure 1).
Figure 1: Socio-demographic characteristics of pregnant women attending ANC at selected Governmental Health Facilities in Harar town, Eastern Ethiopia 2017 (n= 370)
Maternal status on previous and current pregnancy: Out of total study subject 330 (89.2%) women had one up to eight children while the rest were nulliparous. Two hundred sixty-three (71.1%) of study subjects reported that their pregnancy was Planned. Majority of the participant (72.2%) gave alive birth. The frequency of ANC follow up ranged from 1 to 8 with mean and ± SD of (2.33 ±1.159).
Perception of clients with respect to time, distance and privacy of ANC service: The minimum waiting time before being seen by the health care provider immediately without waiting and the maximum was 90 minutes. About one third 143(38%) of the client reported that the time taken before having the service was short. Half of the client’s perceived distance from home to health facility was as average, and 30.3% as too far.
Client provider interaction at ANC service: Majority 321(86.8%) of women reported that health workers provide respectful care. Majority of clients were ranked the behavior of provider’s as good 217(58.6%) Regarding on time spent with the provider 250 (67.6%) said it was appropriate and 315 (85.1%) were fell happy. Around One - third of participant 127 (34.3%) replied their privacy was not maintain while counseling. Nearly half 179 (48.4%) of the client preferred to be seen by female provider as well as 214 (57.8%) preferred to be examined by General practitioners (Table 1).
Table 1: Interaction between service provider and ANC clients at selected Governmental Health Facilities in Harar town, Eastern Ethiopia 2017 (n= 370)
| Variable | Frequency | Percent | Variable | Frequency | Percent | |
|---|---|---|---|---|---|---|
| Respect full care Yes No |
321 49 |
86.8 13.2 |
Response to time spent with provider Happy Not Happy |
315 55 |
85.1 14.9 |
|
| Discussion on health related issues Yes No |
322 48 |
87 13 |
Privacy while counseling Yes No |
127 243 |
34.3 65.7 |
|
| Provider listen compliant Yes No |
324 46 |
87.6 12.4 |
Care provider sex preference Male provider Female provider No sex preference |
20 179 171 |
5.4 48.4 46.2 |
|
| Provider Behavior rank by the respondent Very Good Good Fair Bad |
34 217 99 20 |
9.2 58.6 26.8 5.4 |
Professional preference of the respondent Nurse Midwife General practitioner Specialist |
3 106 214 47 |
0.8 28.6 57.8 12.7 |
|
| perception of time spent with provider Very long Very short Appropriate I don’t know |
70 73 250 25 |
5.9 19.7 67.6 6.8 |
Respondent satisfaction from information received No Yes |
136 234 |
36.8 63.2 |
Components of Focused Antenatal Care provided: For computing the content of FANC service the women received: History taking, Physical examination, laboratory evaluations, Provision of therapeutics (supply). Information provided and advices on danger sign were asked each item had 1 point if performed while having 0 which was not performed. History taking had 7 items which had Personal history, Social History, Family history, Medical history, surgical history, Obstetric history, history for current pregnancy. Physical examination had 11 items whether the women had or not those are weight, height, Bp measurement, Eye conjunctiva and sclera evaluation, neck examination, Breast examination, abdominal examination, fetal heart rate recording, vaginal examination, leg examination for edema and varicose vein evaluation. Laboratory evaluation had 7 items: Hemoglobin/ Hematocrit, VDRL, Blood group, RH factor, Urine test, HIV test, Stool examination. Provision of therapeutics had 3 items: prophylactic iron/folate supplementation, Tetanus toxoid administration and Treated bed provision. Information provision on birth preparedness and complication readiness had 8 items those are birth preparedness, place of birth , Saving Funds , Potential blood donors in case of emergency, birth spacing, Nutrition, HIV/AIDS (PMTCT), Breast feeding. Advice on danger signs had 5 items: Severe headache, abdominal pain, vaginal bleeding, vaginal gush or fluid/ rupture mm, Blurred vision. The total FANC content was 41 among this if the health care provider provide ≥75% of the FANC component (which means approximately 31 out of 41 components) the quality is said to be good which was coded as 1 and if he/she was provide ≤ 74% of FANC component (which means 30 out of 41) it is said to be poor which was codded as 0 after computing each components for each study participants
History Taking, Physical examination, laboratory investigation, therapeutic provision, Information provision and advice about danger sign: Majority of respondent (96.2%) of the clients were asked personal history the least was surgical history which was (50.3%)
The four common routine examinations carried were BP Monitoring (93.5%), weight (89.2%), position of the baby (84.9%) and listening of fetal heart beat (80.5%).
Regarding on laboratory investigation the major evaluation was carried on blood group screening for 359(97%) clients while the least was stool examination for 48(13%) clients.
Majority of the women 323(87.3%) provided iron/folate by the care giver
The most frequent provided information during counseling of pregnant women were about birth preparedness (59.7%) while preparing potential blood donor (26.5%) was the least provided information. Severe headache (66.5%), vaginal bleeding (63%) and blurred vision (59.7%) were the most provided advice to the client (Table 2).
Table 2: History taking, general examination, laboratory investigation and therapeutic provision, Information provision and advice about danger sign to the pregnant women attending ANC at selected Governmental Health Facilities in Harar town, Eastern Ethiopia 2017 (n= 370).
| Performed | Not performed | |||
|---|---|---|---|---|
| Antenatal care services | Frequency | % | Frequency | % |
| History taking | ||||
| Personal history | 356 | 96.2 | 14 | 3.8 |
| Social history | 199 | 53.8 | 171 | 46.2 |
| Family history | 180 | 48.6 | 190 | 51.4 |
| Medical history | 163 | 44.1 | 207 | 55.9 |
| Surgical history | 184 | 49.7 | 186 | 50.3 |
| Past obstetric history | 329 | 88.9 | 41 | 11.1 |
| current obstetric history | 353 | 95.4 | 17 | 4.6 |
| Physical Examination | ||||
| Weight | 330 | 89.2 | 40 | 10.8 |
| Height | 185 | 50 | 185 | 50 |
| Blood pressure | 346 | 93.5 | 24 | 6.5 |
| Eye conjunctiva/sclera | 240 | 64.9 | 130 | 35.1 |
| Neck examination | 128 | 34.6 | 242 | 65.4 |
| Breast examination | 156 | 42.2 | 214 | 57.8 |
| Position of the baby | 314 | 84.9 | 56 | 15.1 |
| Listen FHB | 298 | 80.5 | 72 | 19.5 |
| Vaginal examination | 24 | 6.5 | 346 | 93.5 |
| Edema | 237 | 64.1 | 133 | 35.9 |
| Varicose vein | 172 | 46.5 | 198 | 53.5 |
| Laboratory Evaluation | ||||
| Hemoglobin/ hematocrit | 342 | 92.4 | 28 | 7.6 |
| VDRL for syphilis | 308 | 83.2 | 62 | 16.8 |
| Blood group | 359 | 97 | 11 | 3 |
| RH factor | 352 | 95.1 | 18 | 4.9 |
| Urine analysis | 278 | 75.1 | 92 | 24.9 |
| HIV test | 351 | 94.9 | 19 | 5.1 |
| Stoll examination | 48 | 13 | 322 | 87 |
| Provision of therapeutics | ||||
| Supply of iron/foliate | 323 | 87.3 | 47 | 12.7 |
| Provide tetanus Toxoid (TT) | 320 | 86.5 | 50 | 13.5 |
| Provision of ITN | 49 | 13.2 | 321 | 86.8 |
| Information provision and counseling | ||||
| Birth preparedness | 221 | 59.7 | 149 | 40.3 |
| Place of birth | 199 | 53.8 | 171 | 46.2 |
| Saving funds | 106 | 28.6 | 264 | 71.4 |
| Potential blood donors | 98 | 26.5 | 272 | 73.5 |
| Birth spacing | 167 | 45.1 | 203 | 54.9 |
| Balanced diet | 206 | 55.7 | 164 | 44.3 |
| HIV/AIDS (PMTCT) | 202 | 54.6 | 168 | 45.4 |
| Breast feeding | 144 | 38.9 | 226 | 61.1 |
| Advice about Danger sign | ||||
| Severe headache | 246 | 66.5 | 124 | 33.5 |
| Severe abdominal cramp pain | 175 | 47.3 | 195 | 52.7 |
| Vaginal bleeding | 233 | 63 | 137 | 37 |
| Premature rupture of membrane | 175 | 47.3 | 195 | 52.7 |
| Blurred vision | 221 | 59.7 | 149 | 40.3 |
Quality of ANC service: on this study 90 (24.3%) of the client had get quality ANC service while the rest 280(75.7%) had not get quality ANC service.
Factor associated with Quality of ANC service: Relationship between quality of ANC service and socio demographic variable
On multiple logistic regressions Age, Educational status and occupation of the pregnant women were independently associated with quality of ANC service. Those pregnant women whose age group 25-29 were 2 times (AOR = 2.045, 95% CI: 1.147- 3.647) and women whose age > = 35 were 5 times (AOR = 5.302, 95% CI: 1.908 – 14.734) more like having quality of ANC service than age group less than 24.
Pregnant women whose education level diploma and above, secondary and primary were 3.5 times (AOR = 3.576, 95% CI: 1.397 – 9.154), 2.8 times (AOR = 2.860, 95% CI: 1.217 – 6.718),
and 2.4 times (AOR = 2.465, 95% CI: 1.210 – 5.019) more likely having quality of ANC service than uneducated. Pregnant women who had governmental workers were 10 times (AOR = 10.552, 95% CI: 1.309-85.07) more likely having quality of ANC service than house wife (Table 3).
Table 3: Multivariate analysis of quality ANC service and socio-demographic variables of mother attending ANC at selected Governmental Health Facilities in Harar town, Eastern Ethiopia 2017 (n= 370).
| Quality level | Adjusted OR (95%) CI | ||||
| Characteristics | Poor Quality | Good Quality | Crude OR (95%) | P value | |
| No (%) | No (%) | ||||
| Age in years | |||||
| < 24 | 140 (50) | 31 (34.4) | 1 |
0.006 |
|
| 25- 29 | 101 (36.1) | 39 (43.3) | 1.744 [1.020 – 2.982] * | 0.015 |
2.045[1.147-3.647]* |
| 30 – 34 | 29 (10.4) | 10 (11.1) | 1.557 [0.688 – 3.526] | 0.213 |
1.740[0.728-4.163] |
| >= 35 | 10 (3.6) | 10 (11.1) | 4.516 [1.731 – 11.783]* | 0.001 |
5.302[1.908-14.734]* |
| Educational Status | |||||
| Can’t read and write | 86 (30.7) | 16 (17.8) | 1 |
0.027 |
1 |
| Primary | 91 (32.5) | 32 (35.6) | 1.890 [0.969 – 3.689] | 0.013 |
2.465[1.210- 5.019] * |
| Secondary | 48 (17.1) | 16 (17.8) | 1.792 [0.823 – 3.900] | 0.016 |
2.860[1.217-6.718] * |
| Diploma and above | 55 (19.6 | 26 (28.9) | 2.541 [1.251 – 5.162]* | 0.008 |
3.576[1.397-9.154] * |
| Marital Status | |||||
| Married | 264 (94.3) | 88 (97.8) | 1 |
0.194 |
1 |
| Others | 16 (5.7) | 2 (2.2) | 2.500[0.561 –11.148] | 0.359[0076-1.683] | |
| Occupational status | |||||
| House wife | 139 (49.6) | 49 (54.4) | 1 |
0.019 |
1 |
| Government employed | 75 (26.8) | 30 (33.3) | 7.050 [0.922 -53.929] | 0.027 |
10.552[1.309-85.070]* |
| Merchant | 46 (16.4) | 10 (11.1) | 8.000 [1.027 – 62.299] * | 0.117 |
5.317[0.657-43.056] |
| Others | 20 (7.1) | 1 (1.1) | 4.348 [0.521 – 36.280] | 0.204 |
4.074[0.466-35.640] |
| Average monthly | |||||
| income | 75 (26.8) | 17 (18.9) | 1 |
0.583 |
1 |
| 450 -1000 | 111 (39.6) | 36 (40) | .665 [0.310 – 1.462] | 0.414 |
1.326[0.673-2.613] |
| 1001 – 2000 | 50 (17.9) | 22 (24.4) | .951 [0.460 – 1.909] | 0.177 |
1.747[0.778-3.926] |
| 2001 – 3000 | 44 (15.7) | 15 (16.7) | 1.291[0.597 – 2.791] | 0.644 |
0.644[0.510-2.970] |
| > 3001 | |||||
Relationship between quality of ANC service, current and previous pregnancy status, maternal perception and provider interaction variables: Multivariate logistic regression analysis was done to determine the independent effect of current and previous pregnancy status, maternal perception and provider interaction variables. Still birth history, frequency of visit, response to the time stayed before checkup, provider behavior rank, privacy during counseling, provider sex preference, professional preference, respondent satisfaction form information received were independent variable associated with quality of ANC service.
Pregnant women who had history of still birth were 2 times more likely having quality of ANC service than those who had no history of still birth (AOR = 2.936, 95% CI: 1.177 -7.320). Women who had four or more ANC visit were 4.5 times more likely having quality service than women who had less than four ANC visits (AOR = 4.592, 95% CI: 1.318 - 12.996) .Those women whose respond waiting time was short were 2.9 times more likely having quality of service than who stay for long time (AOR= 2.906, 95% CI: 1.227 - 6.881).
Women who responded the provider behavior as fair were 89.3% less likely having quality of ANC service than who respond behavior of provider as good (AOR = 0.107, 95% CI: 0.027 - 0.424). Women whose privacy maintain while counseling were 4 times more likely having quality of ANC service than their privacy was not maintain while counseling. (AOR = 4.110, 95% CI: 1.753 -9.637). Regarding on professional sex preference pregnant women whose prefer to have a care from female provider were 4 times more likely having quality of ANC service than those who preferred male provider (AOR = 4.650, 95% CI: 1.026 -21.083).
Pregnant women whose prefer to have the service from specialists were 75.7% less likely having quality of ANC service than who prefer nurses. (AOR = 0.243, 95% CI: 0.084 -0.705). Women who were not satisfied from the information received from the provider were 88% less likely having quality of ANC service than who had satisfied. (AOR = 0.12, 95% CI: 0.002-0.068) (Table 4).
Table 4: Multivariate analysis of quality ANC service and maternal status perception of clients variables of mother attending ANC at selected Governmental Health Facilities in Harar town, Eastern Ethiopia 2017 (n= 370).
| Characteristics | Quality level | Crude OR (95%) CI | P | Adjusted OR (95%) CI | |
| Poor Quality | Good Quality | value | |||
| No (%) | No (%) | ||||
| Still birth history | |||||
| No | 206 (73.6) | 61 (67.8) | 1 | 0.021 | 1 |
| yes | 74 (26.4) | 29 (32.2) | 1.323[0.790 – 2.271] | 2.936[1.177 -7.320]* | |
| Planed pregnancy | |||||
| No | 86 (30.7) | 21 (23.3) | 1 | 0.501 | 1 |
| yes | 194 (69.3) | 69 (76.7) | 1.457[0.840 – 2.526] | 0.730[0.292-1.825] | |
| Frequency of visit | |||||
| 1 up to 3 | 261 (93.2) | 67 (74.4) | 1 | 0.012 | 1 |
| > = 4 | 19 (6.8) | 23 (25.6) | 4.716 [2.427-9.163] | 4.592[1.318-12.996]* | |
| Waiting time | |||||
| Long | 74 (26.4) | 20 (22.2) | 1 | 0 | 1 |
| Short | 128 (45.7) | 65 (72.2) | 1.879 [1.055 –3.346] * | 0.015 | 2.906 [1.227 –6.881] * |
| A bought Right | 74 (26.4) | 5 (5.6) | 0.250 [0.089 – 0.701] * | 0.051 | 0.278 [0.077 – 1.004] * |
| Respect full care | |||||
| Yes | 233 (83.2) | 88 (97.8) | 1 | 0.085 | 1 |
| No | 47 (9.6) | 2 (2.2) | 0.113[0.27 – 0.474]* | 0.210[0.036 – 1.237] | |
| Discussion on health | |||||
| related issues | |||||
| No | 31(22.1) | 17 (7.4) | 1 | 1 | |
| Yes | 109 (77.9) | 213 (92.6) | 5.553[1.682 – 18.332]* | 0.227 | 2.928 [0.513-16.712] |
| Provider listen compliant | |||||
| No | 45 (16.1) | 3 (3.3) | 1 | 0.305 | 1 |
| Yes | 235 (83.9) | 87 (96.7) | 17[2.314– 125.498] * | 3.380[0.330-34.632] | |
| Provider Behavior rank | |||||
| Good Fair Bad | 166 (59.3) | 85 (94.4) | 1 | 0.004 | 1 |
| 95 (33.9) | 4 (4.4) | 0.028[0.029 -0.231] * | 0.001 | 0.107[0.027-0.424] * | |
| 19 (6.8) | 1 (1.1) | 0.103[0103 - 0.781] * | 0.263 | 0.146[0.005-4.224] | |
| perception of time spent | |||||
| with provider | |||||
| Very long | 17 (6.1) | 5 (5.6) | 1 | 0.11 | 1 |
| Very short | 64 (22.9) | 9 (10) | 0.478 [0.142 -1.615] | 0.449 | 1.850[0.377- 9.087] |
| Appropriate | 175 (62.5) | 75 (83.3) | 1.457[0.519 - 4.094] | 0.106 | 3.323[0.774-14.274] |
| I don’t know | 24 (8.6) | 1 (1.1) | 0.294 [0.15 -1.324] | 0.413 | 0.319[0.021- 4.924] |
| Privacy of counseling | |||||
| No | 168 (60) | 75 (83.3) | 1 | 0.001 | 1 |
| Yes | 112 (40) | 15 (16.7) | 3.333 [0.182 – 0.594]* | 4.110[1.753-9.637]* | |
| sex preference | |||||
| Male provider | 10 (3.6) | 10 (11.1) | 1 | 0.088 | 1 |
| Female provider | 147 (52.5) | 32 (35.6) | 2.563[0.84 -0.566] * | 0.046 | 4.650[1.026 -21.083]* |
| No sex preference | 123 (43.9) | 48 (53.3) | 0.558[0.153 – 0.997] * | 0.15 | 1.844[0.801 -4.248] |
| Professional preference | |||||
| Nurse | 2 (0.7) | 1 (1.1) | 1 | 0.009 | 1 |
| Midwife | 71(25.4) | 35 (38.9) | 0.568 [0.048 – 6.703] | 0.227 | 0.150[0.007- 3.249] |
| General practitioner | 182 (65) | 32 (35.6) | 0.560 [0.278 – 1.130] | 0.709 | 0.800[0.253-2.594] |
| Specialist | 25 (8.9) | 22 (24.4) | 1.200 [0.101 – 0.396]* | 0.009 | 0.243[0.084 -0.705]* |
| Respondent satisfaction | |||||
| from information received | |||||
| Yes | 146 (52.1) | 88 (97.8) | 1 | 1 | |
| No | 134 (47.9) | 2( 2.2) | 025[0.06 – 0.103] * | 0 | 0.12 [0.002-0.068]* |
Result from Qualitative Study
To supplement the quantitative finding and ascribe the issue which cannot address by the quantitative assessment qualitative study was conducted through observational assessment and in depth interview.
Observational assessment of providers: Performance observation of ANC service session was done in all selected governmental health MCH Units. Among 21 provider 18 providers who were volunteers to be observed and gave their consent was participated. Assessment was conducted based on 42 observation points and 37 clients.
History Taking: Among the observed findings personal and present obstetric history had taken in 94.6 %. However, majority 78.4% of the ANC clients were not greeted respectively and called by their name.
Physical examinations: The frequency of carrying out specific physical examination was similar conjunctiva, breast examination and hand washing done less regularly whereas fundal height measurement, fetal lie, position and listening of fetal heart beat were done more frequently.
Laboratory investigation: On laboratory investigations, observational findings revealed that health care provider screen the clients for HIV test (100%) hemoglobin (94.6%), urinalysis (89.2 %) and VDRL for syphilis which was (78.4%).
Preventive measures and Health education: Out of the total observed clients (78.4%) were received tetanus toxoid vaccination and (62.2%) were supplemented iron/folic acid. Regarding on health education birth preparedness plan and balanced diet were advice for 56.7% and 72.9% of the client.
Communications b/n provider & clients: Majority of the observed (72.9%) cases health care provider were not communicating throughout the procedure. A bought (89.2%) were informed about next appointment. Only few health provide (27%) thanks clients for coming to their health facilities
Results from in depth interview: Majority of informants had similar understanding about quality of health services. Explained quality of health services if it satisfying clients with clean, safe, and standardized services shortly, respectfully without any obstacle and timely……. If the service fulfills the standards and having sufficient equipment as well as sufficient health care provider and well organized health facilities with full set up”….( midwives working for the last 8 years at MCH)
A 34 years Bsc nurse who are working at MCH for 11 years said that “the quality of the service provided in our organization was good and it was improved because of the health facility expansion and new buildings but our main challenge was the huge number of students who come to make a practice from different health science college were affects as in order not to provide the service as we need this is compromise the service quality”.
There are positive changes in most of health facilities like Securing client’s record and getting services at any time by clients preparing convenient toilet, having necessary material except ultrasound and also there are some changes which was also affecting the service. Regarding on changes through time
…. in the previous time basic necessary supply, medication and drug were not available in the MCH unit because of this we was send the mother to the pharmacy and so on but now a days everything is in our hand in the MCH room except ultrasound machine…
…“now a day’s clients were dissatisfied because of the change in our facility. in the previous time the client will put only 6 birr to the card room for having laboratory service but now a days the money they put it to the card room become 50 birr these makes them disappointed and reduce the client flow towards the health facilities”
Informants reported the major challenges that affect quality of ANC services in their health facilities. Those are limited resources, mainly human resources, lack of up to date training for provider, increased number of clients, workload, and absence of separate rooms to provide services properly
….“we are providing EPI and Antenatal care in the same room while I was provide ANC service another health care worker also provide immunization in the same room this may affect the safety and privacy of our clients”.
measures to be taken to improve quality of reproductive health (ANC) services majority of informants mentioned a need for addressing to major challenges, continuous monitoring and evaluation system should be established, staff encouragement mechanism should be established, caring out experience sharing form and maintaining clients privacy is fundamental to improving quality of ANC services
… All stake holders should have to work for the benefit of their population rather than their interest and benefit and also they should have to identify what was the major service the people need and need to work on It”
……“Regional health office should have to make a continuous follow up and regular supportive supervision and timely corrective measure rather than conducting annual review meting every 6 months. In addition to this another health care provider also stated that “ the one who will assigned as a leader to the health institution should be better to be professional person who had a back ground knowledge of health rather a politician which was far knowledge for health and full of low and ethics”.
Discussion
On this study the overall prevalence of quality of ANC service was 24.3%. This is in line with the finding of study conducted in Tigray which was 24.5% [15]. On this study personal history was asked for 96.2% of clients and in Jimma and Sudan study also 94.6% and 98% which was higher. Past obstetric history, medical and surgical history were asked among 88.9%, 44.1% and 49.7% pregnant women while in other study on Jimma past obstetric history 94.2% medical history 93.8% as well surgical history were asked 94.2% which was higher than this study finding this may be due to inconsistent history taking habit of the health provider because of client over load [8,14].
On this study the four common routine examinations carried were BP monitoring, weight, abdominal examination and listening of fetal heart beat this finding is similar to the finding in Bangladesh, Pakistan, Nigeria, Sudan and Bahir- Dar [8-11,16,17]
On this study hemoglobin/hematocrit evaluation (92.4%) and HIV test (94.9%) evaluation were higher than studies conducted in Sudan (62.3%) Bahir -Dar (30.6% and (82.3%), and Jimma (32.2% and 52.1%) this may be due to the continuous availability of laboratory service with full access of reagent provision with un interrupted supply [8,10, 14]
Regarding on provision of theraputics on this study iron and Tetanous toxid provision was higher (87.3 and 86.5%) than study conduced in jimma (34.3% and 78.5%) this is may be due to consistence supply of iron and TT Vaccine from regional health office [14].
Information provision on birth preparedeness (59.7%) and place of birth (53.8%) were higer on this study than study conducted in Gonder which was (50.6%) and (54.1%) but information on saving fund (28.6%) , blood donor preparation (26.5%) and PMTCT (54.9%) were also lower on this study than Gonder which was (45.2%) , (37.5%) and (70.1%). This may be due to inconsistence provision of information by the health care provider due to work over load and shortage of staffs [18].
Information provision on danger sign is higher (72.9%) in this study than study conducted in Gonder (52.2%) and Jimma (34.3%) this may be due to health care provider give more emphasis for danger sign information provision. [14,18].
Pregnant women who had history of still birth were 2 times more likely having quality of ANC service than those who had no history of still birth. (AOR = 2.936, 95% CI: 1.177 -7.320). This may be because of history of still birth women may have more frequent visit and having a comprehensive care.
Women who had four or more ANC visit were 4.5 times more likely having quality service than women who had less than four ANC visits. (AOR = 4.592, 95% CI: 1.318 - 12.996). This may be due to having repeated service and frequent contact with FANC Components and having the service in familiar approaches.
Women whose respond waiting time was short had 2.9 times more likely having quality of service than who stay for long time. (AOR= 2.906, 95% CI: 1.227 - 6.881). This may be due to the women having the service as soon as she wants to have or immediately without long stay.
Women who responded the provider behavior as fair were 89.3% less likely having quality of ANC service than who respond behavior of provider as good (AOR = 0.107, 95% CI: 0.027 - 0.424). This may be due to respectful treatment of the health care provider which perceived the women as not having the necessary service.
Women whose privacy maintain while counseling were 4 times more likely having quality of ANC service than women’s whose privacy not maintain (AOR = 4.110, 95% CI: 1.753 - 9.637). This may be due to privacy is the major factor that affect quality service.
Women who were not satisfied from the information received from the provider were 76 % less likely having quality of ANC service than those who had satisfied. (AOR = 0.243, 95% CI:
1.84 -0.705). This is due to client satisfaction is one of the major factor that indicate quality service and having of quality services.
STRENGTH AND LIMITATION OF THE STUDY
Strength of the study
- The questioner was pretested on similar setting and a necessary modification was made to minimize the difficulty during the data collection.
- Data collectors had exposure before this time and were experienced for exit interview
- Full information was given about the objective of the study and agreement was obtained from clients, before data collection, and daily checkup made for the completeness of the questionnaire at field level and during data collection time
- The study has assessed quality of ANC service through client interview and observed health providers performance.
- It has also assessed basic equipment’s and materials in health facilities and use of these different assessments tools to verify quality of ANC service in through triangulation of the methods.
- Using of both qualitative and quantitative methods together
- There is lack of adequate literatures in our country, this study has identified the level of quality ANC service in Harari and I hoped this study would be an input in this regard.
Limitation of the study
- The study lacks enough literature on quality ANC relevant to Ethiopia and study area in particular as focusing with factor associated ANC service.
- Providers show the best behavior responses during client-provider interaction while there are observed
- Large confidence interval was observed due to small sample size in some variables
- As it was a cross sectional study it’s impossible to make causal reference for population under investigation
Conclusion
Generally, the studies showed that majority of clients were not received quality ANC service. Quality ANC service was higher; among women age 25 -29 and ≥ 35years, educational status, occupation, history of still birth, frequency of ANC visit, Waiting time, provider behavior rank, provider sex preference, privacy while counseling and client satisfaction from the provider advice.
This study also revealed that the factor which precludes the provider in order not to provide quality service those are: limited staff, lack of private room, lack of up-to-date training, large number of clients and work load on the staffs.
Recommendation
- Stressed should be put on health providers to focus on FANC component for client’s to have quality ANC service by the health facility leaders.
- Early implementation of the new 2016 WHO recommendations visits.
- Health facilities should have work on to shorten client waiting time before having the service
- Privacy maintaining strategy must be implemented by the health facilities in collaboration with regional health office.
- Additional female staff should be recruited as to reduce the work load among staffs and to be assigned in specific place at a time.
- Guide line on provision of ANC should have to be prepared by the responsible body either by FMOH or Regional health office
- Regular supportive supervision has to be considered by Regional health office frequently
- Separate, ANC room and other service provision like EPI and Family planning must established as it was the major factor which affect clients privacy
- Clients’ vital signs should be measured at regular bases
- Stakeholders (governmental and non-governmental organization) should be providing up to date in service training majorly on skill improvement like BEmONC and others.
- Professional encouragement mechanism should have to be established by the organization.
There are no references