Journal Name: Journal of Gynecology and Cure
Article Type: Research
Received date: 7 July, 2018
Accepted date: 16 July, 2018
Published date: 20 July, 2018
Citation: Kathpalia SK, Mehrotra M, Sharma C, Anita Yadav, Jena PS (2018) Life Saving Hysterectomy – Five Years Experience in an Apex Referral Hospital in Remote Islands in India. J Gynecol Cure Vol: 1, Issu: 1 (01-6).
Copyright: © 2018 Kathpalia SK, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Introduction: Hysterectomy may be performed as an emergency procedure in obstetrics as a lifesaving measure; called emergency peripartum hysterectomy; performed as a last resort in cases of uncontrolled hemorrhage. Delaying or postponing the decision to perform hysterectomy may cause deterioration of maternal condition. A study was conducted about life saving hysterectomies performed at an apex referral hospital in Port Blair, India.
Material and Methods: This was a retrospective cohort study performed over a period of five years; from Aug 2012 to Aug 2017. The objective was to study the cases of emergency hysterectomy, the incidence, maternal and perinatal outcome and factors which lead to the procedure.
Results and Observations: There were total of 19 emergency hysterectomies performed during the period of study, two performed for gynecological and rest for obstetrical indications. The incidence was 1.21 per 1000 deliveries. The commonest indication was atonic hemorrhage (35%), second most common indication being morbidly adherent placenta (23%) in cases of post CS pregnancies.
Conclusion: Hysterectomy may have to be carried out as an emergency procedure to save the life of parturient mother; it may be required at the time of delivery, cesarean section or during puerperium. In recent years, abnormal placentation has become a more common indication due to the greater number of pregnant women with previous cesarean section. Whether hysterectomy should be total, or subtotal should be individualized. Universal increase in cesarean section will result in more cases of adherent placenta which will lead to a rise in emergency hysterectomies in future.
Keywords
Peripartum, Hysterectomy, Uncontrolled hemorrhage.
Abstract
Introduction: Hysterectomy may be performed as an emergency procedure in obstetrics as a lifesaving measure; called emergency peripartum hysterectomy; performed as a last resort in cases of uncontrolled hemorrhage. Delaying or postponing the decision to perform hysterectomy may cause deterioration of maternal condition. A study was conducted about life saving hysterectomies performed at an apex referral hospital in Port Blair, India.
Material and Methods: This was a retrospective cohort study performed over a period of five years; from Aug 2012 to Aug 2017. The objective was to study the cases of emergency hysterectomy, the incidence, maternal and perinatal outcome and factors which lead to the procedure.
Results and Observations: There were total of 19 emergency hysterectomies performed during the period of study, two performed for gynecological and rest for obstetrical indications. The incidence was 1.21 per 1000 deliveries. The commonest indication was atonic hemorrhage (35%), second most common indication being morbidly adherent placenta (23%) in cases of post CS pregnancies.
Conclusion: Hysterectomy may have to be carried out as an emergency procedure to save the life of parturient mother; it may be required at the time of delivery, cesarean section or during puerperium. In recent years, abnormal placentation has become a more common indication due to the greater number of pregnant women with previous cesarean section. Whether hysterectomy should be total, or subtotal should be individualized. Universal increase in cesarean section will result in more cases of adherent placenta which will lead to a rise in emergency hysterectomies in future.
Keywords
Peripartum, Hysterectomy, Uncontrolled hemorrhage.
Introduction
Hysterectomy is generally performed as an elective procedure for various indications and usually done in older patients who have completed their families. Rarely and mostly in ‘Obstetrics’ hysterectomy is performed as a lifesaving procedure; called Emergency Peripartum Hysterectomy (EPH) which is typically performed as a last resort in cases of uncontrolled hemorrhage; who are not responding to conservative methods [1]. First successful cesarean hysterectomy or EPH was performed in United States in 1869, immediately thereafter, Porro of Milan conducted the first cesarean hysterectomy where both baby and mother survived. As a mark of memory; the procedure is often referred to as the ‘Porro’ operation.
The decision to perform EPH is difficult as the patients are young and they will lose their future fertility along with loss of menstrual function and may develop many long term psychological problems and complications. Delaying or postponing the decision may cause deterioration of maternal condition and at times result in maternal mortality. Probably this is one of the most difficult decisions an obstetrician has to make hence it requires prompt assessment of patient’s condition and good clinical judgment.
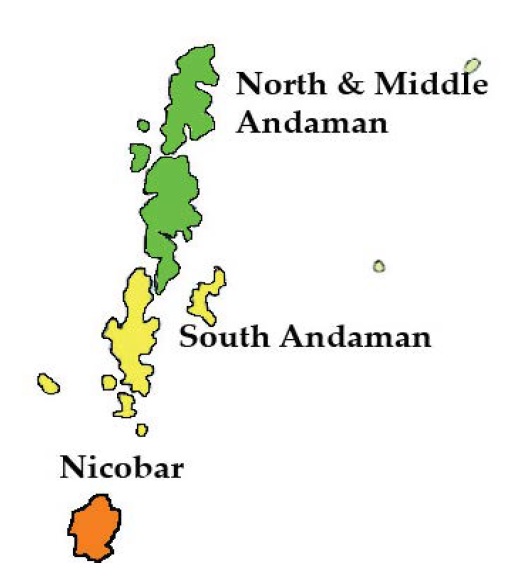
A study was conducted about life saving hysterectomies performed over a period of five years at an apex referral hospital in Port Blair; India. This is the only referral hospital in whole of Andaman and Nicobar Islands (Figure 1), all high risk and emergency cases are referred to this hospital. The terrain is difficult; many islands have water ways as the only mode of transportation and air evacuation is difficult especially after the last light. This cohort study performed over a period of five years; from Dec 2012 to Dec 2017.
Figure 1: Andaman and Nicobar Islands, India.
Materials and Methods
Our objective was to study the cases of emergency hysterectomy, the incidence, maternal and perinatal outcomes and factors which led to the emergency procedure performed over a period of five years. This descriptive study was conducted to analyze all the cases that had undergone emergency hysterectomy as a lifesaving procedure; was conducted at GB Pant Hospital and Andaman Nicobar Islands Institute of Medical Sciences, Port Blair, India. The cases performed during the current year and previous four years were included in the study. Operation theatre records too were checked, and it was found that the documents of all the cases that underwent emergency hysterectomy during the study period were available and these documents were obtained from medical record section. Demographic data, clinical variables, admission like direct admission or referral, mode of transport before admission and all available clinical data including duration of hospital stay, both maternal and perinatal outcomes were recorded and analyzed; the data collected was compared with the data available in literature.
Results and Observations
There were total of 19 emergency hysterectomies performed during the period of study of five years, two performed for gynecological reasons and rest for obstetrical indications (Table 1). During this five-year period there were 14,028 deliveries; and 17 obstetrical hysterectomies there by indicating the incidence of EPH in our study to be 1.21 per 1000 deliveries. The incidence of EPH has been quoted by different authors as varying from 0.2 to 8.5 per 1000 deliveries [2].
Table 1: Indications of emergency hysterectomy.
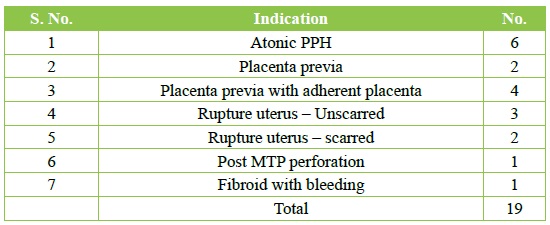
The age varied from 24 to 32 years, there was one case of 42 years of age who was nulligravida with multiple fibroids and had undergone emergency hysterectomy for uncontrolled bleeding with hypotension. The patients who undergo EPH are in reproductive age group and young as reported in one study where 62.5% belonged to the 26-30 years age group and 31% belonged to the 20-25 years age group [3].
Of the 17 cases of peripartum hysterectomy 3 were primigravida and rest were multiparous. Four had history of one previous Cesarean Section (CS) and two had history of previous two CSs. The commonest indication was atonic post-partum hemorrhage (PPH - 6/17), most of the studies have reported atonic PPH as the commonest indication for EPH [1,3-5]. Of the six cases who underwent hysterectomy for atonic PPH, three had a normal delivery and developed PPH which did not respond to conservative treatment like uterotonic drugs, intravenous fluid therapy including multiple blood transfusions and intrauterine tamponade. Two cases had uncontrolled bleeding at the time of CS (both emergency CSs) and one case had bleeding in the immediate post-operative period in the operation theatre and underwent re-exploration followed by hysterectomy.
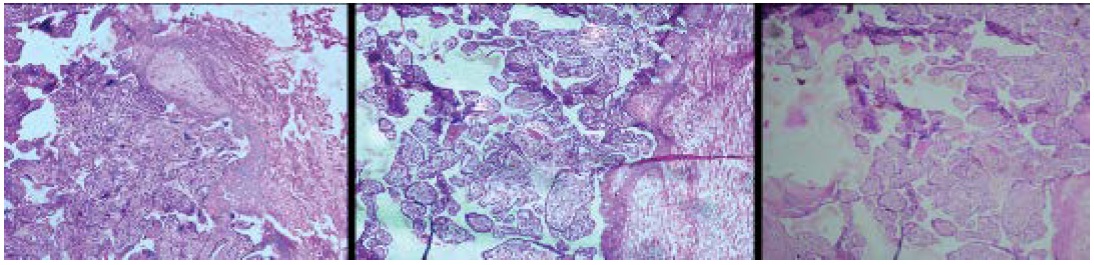
Second most common indication for EPH was morbidly adherent placenta in cases of post CS pregnancies. Five cases underwent hysterectomy for anteriorly located placenta praevia with accreta (Figure 2 and Figure 3). In four cases the decision to perform hysterectomy was undertaken on the operation theatre table as bleeding was uncontrolled at the time of removal of placenta. Diagnosis of placenta accreta was known preoperatively in all cases; which was suspected on transabdominal sonography and confirmed on Magnetic Resonance Imaging (MRI). Adherent placenta was removed with difficulty in one case, but the patient had severe bleeding with hypotension in post-operative period and hysterectomy was performed as lifesaving procedure. Incidence of abnormal attachment of placenta [2,6] in cases of previous cesarean pregnancy causing morbidly adherent placenta has been escalating. The frequency of EPH in patients with a history of previous cesarean has increased remarkably over the past few years [7]. Many studies have reported marked increase in the incidence of placenta accreta over the last few years; which has accounted for almost 50% of EPH [6,8]. These days the most prevalent cause for morbidly adherent placenta is previous cesarean section. Incidence increases directly proportional to the number of previous CSs.
Figure 2: Adherent placental bits in lower segment.
Figure 3: Adherent and infiltrating placenta.
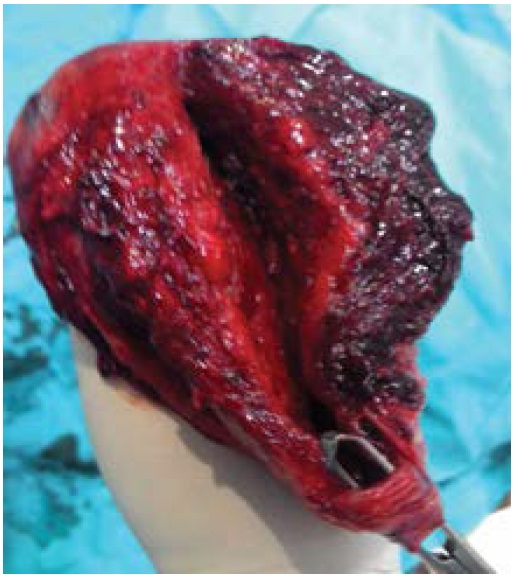
There were five cases of rupture uterus where EPH was performed. Three ruptures occurred in unscarred uterus (Figure 4) and two in scarred uterus due to previous CS. All rupture cases were referred cases, one case had rupture of both anterior and posterior walls of uterus (Figure 5) and she was referred as a diagnosed case of obstructed labour with rupture uterus. Other four cases were referred with diagnosis of prolonged labour and were diagnosed as rupture uterus at this hospital. The three rupture cases of unscarred uterus were in labour in the peripheral places where the labour was prolonged; hence they were transferred to our hospital. The average time taken for them to reach the hospital was 7.2 hours and they had to be transported by road and ferry since the terrain is difficult. The reason for rupture resulting in hysterectomy was delay in reaching the referral hospital. The hospital where study was conducted is the only hospital in the islands where facilities for CS and anesthesia are available. Two cases were evacuated by air. Incidence of rupture uterus as the indication for EPH in the western world has reduced greatly but it remains to be a common indication in third world countries like ours due to grand multiparity, lack of antenatal care and unsupervised labour at home. Hysterectomy was performed in two cases of placenta praevia who had uncontrolled bleeding at the time of CS and decision to perform hysterectomy was undertaken on operation theatre table. These two cases did not have history of CS and neither of them had morbidly adherent placenta.
Figure 4: Uterus showing lateral wall rupture.
Figure 5: Anterior and posterior rupture of uterus.
There were two cases where emergency hysterectomy was resorted to due to non-obstetrical indications. One multiparous case had undergone induced abortion at 12 weeks of gestation outside in a private clinic and continued to have excessive and uncontrolled bleeding. Laparotomy revealed hemoperitoneum and large uterine perforation. The second case; 42 years old, was nulliparous with multiple fibroids admitted with severe bleeding and signs of hypovolemic shock. She was to undergo elective hysterectomy the coming week but in view of severe bleeding she underwent emergency hysterectomy (Figure 6).
Figure 6: Uterus with multiple fibroids.
Two out of seventeen cases underwent subtotal hysterectomy while in all other cases total hysterectomy was performed. The cases who had undergone subtotal hysterectomy; were cases of post CS pregnancies where bladder was markedly adherent and could not be separated completely. Two patients could not be saved and expired; both expired within 24 hours of surgery indicating an incidence of 11.7% of maternal mortality. The cause of hysterectomy the coming week but in view of severe bleeding she underwent emergency hysterectomy (Figure 6). Two out of seventeen cases underwent subtotal hysterectomy while in all other cases total hysterectomy was performed. The cases who had undergone subtotal hysterectomy; were cases of post CS pregnancies where bladder was markedly adherent and could not be separated completely. Two patients could not be saved and expired; both expired within 24 hours of surgery indicating an incidence of 11.7% of maternal mortality. The cause of death in the two cases was irreversible shock; one case had shown evidence of Disseminated Intravascular Coagulation (DIC). Both the cases who expired were referred cases with diagnosis of obstructed labour and were found to have rupture uterus on laparotomy. Both the cases were evacuated by road and ferry and took six hours to reach the hospital after the decision for transfer was taken. All cases were kept in ICU after surgery. Duration of stay in Intensive Care Unit (ICU) varied from 3 to 6 days. There were four perinatal deaths (three stillbirths and one neonatal death).
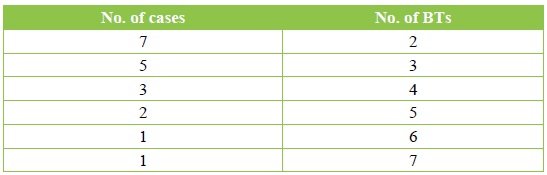
Post-operative complications are shown in Table 2, one case of placenta accreta developed vesico-vaginal fistula but recovered after prolonged catheterization. There was no case of ureteric injury. All the cases required blood and blood component transfusion. Maximum number of packed cells transfused was seven in one case; the details of blood transfusion are shown in Table 3. There was one case that developed DIC.
Table 2: Postoperative complications.
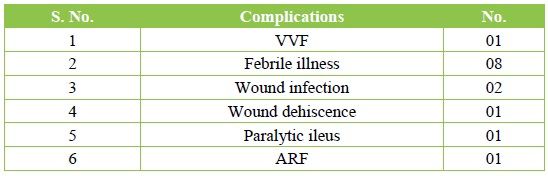
Table 3: Blood transfusion.
Discussion
Hysterectomy is a planned gynecological surgical procedure performed electively. At times uterus is removed as a preplanned procedure at the time of CS; classified as cesarean hysterectomy done for incidental diseases like premalignant lesions of cervix or multiple uterine fibroids etc. Hysterectomy may have to be carried out as an emergency procedure to save the life of expectant woman. EPH may be required at the time of delivery, CS or during puerperium. It is more commonly performed at the time of operative delivery than normal vaginal delivery as reported by many studies including this study [9,10].
Uterine atony was the commonest indication for EPH in past followed by uterine rupture. Our study too indicated uterine atony as the commonest indication for EPH as reported by many other studies [1,3-5]. Postpartum hemorrhage continues to be the leading cause of maternal death all over the world. Uterine artery embolization [11] is the latest and most advanced method of controlling this hemorrhage but this may not be available in most of the places hence EPH remains an easier and more practical option in cases where all conservative methods have failed.
These days; abnormally adherent placenta is responsible for EPH more than atonic uterus as more and more women are having history of previous operative delivery [4,12]. Studies have shown where placenta accreta following previous CS has accounted for almost 50% of peripartum hysterectomies [12]. The incidence of EPH occurring with a history of previous CS has increased remarkably over the last few decades. Many reports have revealed association between abnormal placentation and previous CS which accounts for the high incidence of EPH [7]. Incidence of adherent placenta increases proportionately with the number of previous CSs. The likelihood of undergoing EPH is much more in placenta praevia with accreta than in placenta praevia alone.
Underlying risk factors can be predicted to a great extent by performing antenatal ultrasound with color doppler studies and magnetic resonance imaging (MRI). Whether EPH should be total or subtotal has been a subject of controversy and discussion. Total hysterectomy is better as risk of developing cervical cancer is abolished. Subtotal hysterectomy has some advantages like reduction in blood loss and shorter duration of surgery and fewer chances of intra and postoperative complications. Some advocate subtotal hysterectomy as first choice because it takes less time especially when these patients have hemodynamic instability. Subtotal hysterectomy may not be effective in management of placenta accreta in lower segment of uterus. Both subtotal and total hysterectomy; have their own advantages and disadvantages hence decision to perform total or subtotal should be individualized. Total hysterectomy should however be performed when active bleeding occurs from lower uterine segment as the blood supply to the lower segment may remain intact.
Incidence of EPH has been increasing all over the world as one meta-analysis reported annual rise of 8% [13]. Operative difficulty as well as chances of injury to the ureter, urinary bladder are much more in the post CS group because of much higher incidence of placenta praevia and morbidly adherent placenta. Chances of urinary tract injury at the time of EPH are higher. Incidence of maternal mortality of 8% has been reported due to various causes like acute renal failure, cardiac arrest and DIC [3].
EPH is a risky and dramatic operation; at times with disastrous consequences and decision to perform EPH is undertaken when conservative measures have failed to control hemorrhage or uterus is not repairable like in rupture uterus. EPH has been aptly named as a near miss event [14]. A near miss event is the one where a parturient woman suffered a potentially fatal condition but survived.
There are occasions when conservative measures are not likely to succeed; there should be no further procrastination in performing EPH as delay may lead to further blood loss, increased transfusion requirements, operative time, DIC, and increased possibility of maternal mortality. These patients are usually in poor general condition as they are hemodynamically unstable after severe blood loss. Surgery must be performed quickly without compromising the patient’s safety. EPH performed by an experienced and senior consultant will considerably reduce the operating time, number of blood transfusions and hospital stay. EPH is not a common surgery; hence the experience of performing this difficult operation is limited among the young specialists.
Risk assessment should be done during antenatal period and patients who are at risk for undergoing EPH like placenta praevia especially anterior and in post CS cases; should be referred to higher centers to avoid maternal morbidity and mortality. Consent for hysterectomy should be obtained in advance. One may consider performing hysterectomy as a planned procedure in cases of placenta accreta in multiparous women after extracting the fetus from upper segment without making any attempt at removal of adherent placenta. Universal increase in CS rate will result in more cases of morbidly adherent placenta which will give rise to increased number of EPH in future.
Limitations: The number of cases of hysterectomies was small as the incidence of EPH is not very common.
Disclosure
Authors report no conflict of interest in this work
Bhattacharyya R, Mukherjee K (2016) Emergency Peripartum Hysterectomy: Indications and Obstetrical Outcome (A 5 years Review). Int Education Res J 5: 58-60. [ Ref ]
De la Cruz CZ, Thompson EL, O’Rourke K, Nembhard WN (2015) Cesarean section and risk of emergency Peripartum hysterectomy in high income countries: a systematic review. Arch Gynecol Obstet 292: 1201-1215. [ Ref ]
Halesha B, Raju VS, Chandrashekar K, Sahana KP (2013) Emergency Peripartum Hysterectomy: A Retrospective Study at a Tertiary Care Hospital in Karnataka. Indian J Public Health Res Development 4: 103- 106. [ Ref ]
Sahin S, Guzin K, Eroqlu M, Kayabasoqlu F, Yasartekin MS (2014) Emergency peripartum hysterectomy: our 12-year experience. Arch Gynecol Obstet 289: 953-958. [ Ref ]
Tapisiz OL, Altinbas SK, Yirci B, Cenksoy P, Kaya AE, et al. (2012) Emergency peripartum hysterectomy in a tertiary hospital in Ankara, Turkey: a 5-year review. Arch Gynecol Obstet 286: 1131-1134. [ Ref ]
Allam IS, Gomaa IA, Fathi HM, Sukkar GF (2014) Incidence of emergency peripartum hysterectomy in Ain-shams University Maternity Hospital, Egypt: a retrospective study. Arch Gynecol Obstet 290: 891-896. [ Ref ]
Yucel O, Ozdemir I, Yucef N, Somunkiran A (2006) Emergency peripartum hysterectomy: 9-year review. Arch Gynecol Obstet 274: 84-87. [ Ref ]
Korejo R, Nasir SBA, Yasmin H (2012) Emergency Obstetric Hysterectomy. JPMA 62: 1322-1325. [ Ref ]
Agrawal S, Yadav R, Raghunandan C, Dhingra S, Kaur H (2013) Peripartum Hysterectomy in a teaching hospital in India. Asian J Med Sci 4: 5-9. [ Ref ]
D’Arpe S, Franceschetti S, Corosu R, Palaia I, Didonto V, et al. (2015) Emergency peripartum hysterectomy in a tertiary teaching hospital: a 14-year review. Arch Gynecol Obstet 291: 841-847. [ Ref ]
Singhal S, Singh A, Raghunandan C, Gupta U, Dutt S (2014) Uterine artery embolization: exploring new dimensions in obstetric emergencies. Oman Med J 29: 217-219. [ Ref ]
Korejo R, Nasir A, Yasmin H, Bhutta S (2012) Emergency obstetric hysterectomy. J Pak Med Assoc 62: 1322-1325. [ Ref ]
Tunçalp O, Hindin MJ, Souza JP, Chou D, Say L (2012) The prevalence of maternal near miss: a systematic review. BJOG 119: 653-661. [ Ref ]
Chawla J, Arora D, Mohini P, Sangita N (2015) Emergency Obstetric Hysterectomy: A Retrospective Study from a Teaching Hospital in North India over Eight Years. Oman Med J 30: 181-186. [ Ref ]