Journal Name: Journal of Pediatrics and Infants
Article Type:Case Report
Received date: 14 October, 2019
Accepted date: 19 November, 2019
Published date: 26 November, 2019
Citation: Aygün E, Ertürk EY, Kaya H, Yalçın O (2019) Bilateral Breast Abscess in the Neonatal Period. J Pediat Infants Vol: 2, Issu: 2 (01-04).
Copyright: © 2019 Aygün E et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Background: In this study we wish to attract attention to mistaken interventions to the breast tissue of neonates and to increase awareness about this topic among personnel providing health services to neonates.
Case presentation: A fourteen-day male infant was brought to the pediatric emergency clinic with swelling, redness, hardness and discharge complaints in the region of both breasts. Ultrasonography of the breast tissue of the patient identified appearance compatible with a dense-content abscess in the form of hyperechoic or hypoechoic avascular mass. Bilateral breast abscess responded to surgical and medical treatment.
Conclusion: It is important to recognize physiological breast hypertrophy in newborns. In physiological hypertrophy, the breast bud is neither red nor soft and heals spontaneously. No intervention is required.
Keywords
Abbreviations: CRP: C-reactive protein, E2: Estradiol, FSH: FollicleStimulating Hormone, LH: Luteinizing hormone, MRSA: Methicillinresistant staph aureus.
Abstract
Background: In this study we wish to attract attention to mistaken interventions to the breast tissue of neonates and to increase awareness about this topic among personnel providing health services to neonates.
Case presentation: A fourteen-day male infant was brought to the pediatric emergency clinic with swelling, redness, hardness and discharge complaints in the region of both breasts. Ultrasonography of the breast tissue of the patient identi ied appearance compatible with a dense-content abscess in the form of hyperechoic or hypoechoic avascular mass. Bilateral breast abscess responded to surgical and medical treatment.
Conclusion: It is important to recognize physiological breast hypertrophy in newborns. In physiological hypertrophy, the breast bud is neither red nor soft and heals spontaneously. No intervention is required.
Key words
Breast Abscess, Newborn Baby, Pediatrics, Bilateral
Abbreviations: CRP: C-reactive protein, E2: Estradiol, FSH: FollicleStimulating Hormone, LH: Luteinizing hormone, MRSA: Methicillinresistant staph aureus.
Background
In both sexes, temporary neonatal breast hypertrophy is frequently observed due to the effect of maternal and placental hormones. This hypertrophy is thought to be triggered linked to prolactin release in the neonate caused by the fall in maternal estrogen levels after pregnancy [1]. This temporary breast growth generally begins a few days after birth in the neonate and regresses on its own in maximum 4-6 months. There is no erythema or temperature increase.
Mastitis and breast abscess are very rarely observed in the neonatal period [2]. Skin colonization of the neonate begins with birth. As the skin is thin and immunity is insufficient, compression of breast tissue and massage of the breast may cause mastitis and breast abscess [3]. Mastitis may ameliorate with antibiotherapy; however, if infection spreads and causes abscess in the breast, surgical drainage should be performed. Infection is frequently localized and may cause cellulitis, osteomyelitis, meningitis, brain abscess and sepsis [2,4-6]. In this study we wish to attract attention to mistaken interventions to the breast tissue of neonates and to increase awareness about this topic among personnel providing health services to neonates.
Case Presentation
A fourteen-day male infant was brought to the pediatric emergency clinic with swelling, redness, hardness and discharge complaints in the region of both breasts.
With no problems on antenatal follow-up, the case was the 38-year old mother’s first pregnancy, born weighing 3200 g at term and by cesarean. The patient was observed to have swelling of both breasts after birth and the mother massaged this region. Two days before, swelling, redness, hardness and discharge complaints were observed to develop in the region of both breasts.
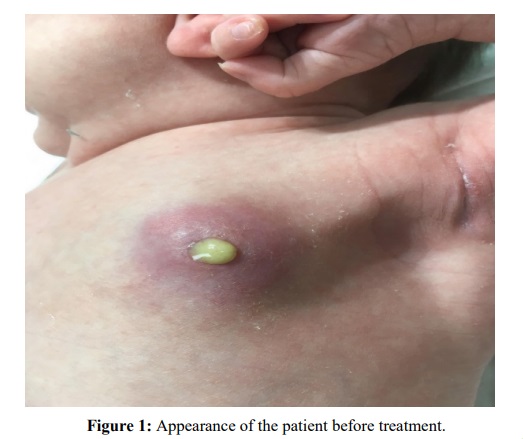
Physical examination found general status good, with vibrant neonatal reflexes, body temperature 36.5℃, peak heart rate 140/min, respiratory rate 38/min, and blood pressure 78/44 mmHg. Both breasts had clear hyperemia, hardness, fluctuations causing swelling and temperature increase, with breast dimensions 3 x 3 cm, with other system aspects assessed as normal (Figure 1).
Figure 1: Appearance of the patient before treatment.
The patient had Hb: 16 gr/dl, leukocyte: 14.680/mm³ (45% Neutrophil, 40% Lymphocyte), Platelet: 244.000/ mm³, and CRP: 22 gr/L. Biochemical parameters were within normal limits.
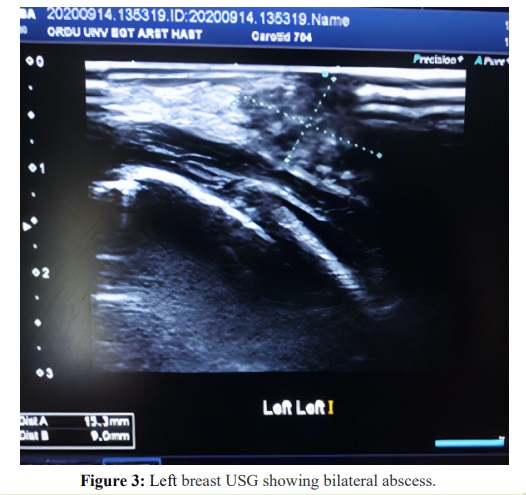
Ultrasonography of the breast tissue of the patient identified appearance compatible with dense-content abscess in the form of hyperechoic or hypoechoic avascular mass (Figures 2 and 3).
Figure 2: Appearance of the patient before treatment.
Figure 3: Left breast USG showing bilateral abscess.
With breast abscess identified, the patient had drainage performed and sent for culture and antibiogram. Empirical vancomycin and cefotaxime treatments were begun intravenously. The abscess content was observed to have gram positive cluster cocci on gram staining. Culture produced methicillin-susceptible Staphylococcus aureus. The patient had cefotaxime treatment stopped on the 3rd day and continued with vancomycin.
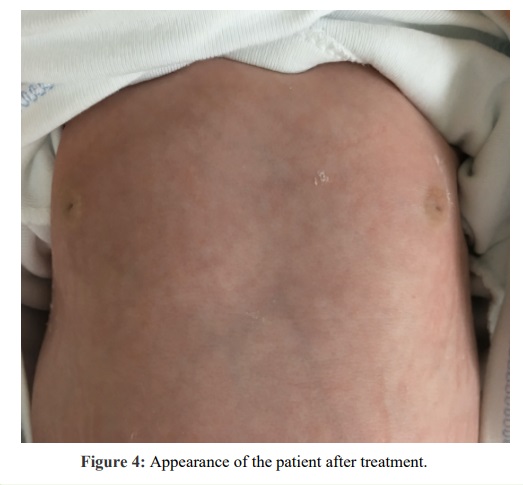
On follow-up, swelling of both breasts appeared to be fully ameliorated by the 10th day (Figure 4). There was no proliferation in blood culture. Repeated tests identified amelioration in CRP elevation.
With no additional problem during follow-up, the case completed antibiotherapy in 10 days and was discharged.
Figure 4:Appearance of the patient after treatment.
Discussion and Conclusion : The breast tissue infection of mastitis and association with abscess is very rare in the neonatal period. Generally, it is observed in term infants. The rarer observation in preterm infants is thought to be linked to less development of breast tissue [2,4,7].
It is observed in the first 1-6 weeks of life, with incidence increasing in the 2nd-3rd weeks [5,8-11]. Mostly unilateral, there are cases with bilateral mastitis developing in the literature, as in our case [12,13]. Generally, it is observed 2 times more in girls; however, no sex difference was determined for the first two weeks of life. This situation is thought to be linked to the physiological breast growth in girls being observed more after the second week.
The pathogenesis of mastitis is not fully known. However, infection is thought to develop mostly from skin flora entering the nipple with retrograde spread via the ductal canals [2,7]. In the literature, there are cases reporting mastitis and breast abscess in the infants of breastfeeding mothers with postpartum breast abscess. In these cases, the mastitis vector is the mother was identified to be the same as in the infant. It is thought that microorganisms in breastmilk cause bacteremia in the infant leading to mastitis and breast abscess. Among vectors identified in reported cases are methicillin-resistant Staphylococcus aureus and group B streptococci [14,15]. When our patient is assessed in terms of the mother, there were no symptoms or findings leading to consideration of mastitis or abscess in the mother. Abscess formation is reported in 40-70% of infants with mastitis and generally is observed in cases with insufficient treatment [2,4,7].
Initially breasts are identified to have growth, erythema, induration, tension and temperature increase. The skin around the affected breast tissue changes and axillary lymph node growth may be observed. If abscess formation develops, fluctuation may be taken [7]. In our case, 2 days before admission, erythema and swelling had begun in the breasts and bilateral breast abscess was identified. Elevated fever, restlessness and toxic appearance is present in 30% of patients. Leukocytosis and CRP elevation is observed in 50-70% of cases [2,8]. In 83-88% of cases, the vector is Staphylococcus aureus [2,4,8,12]. Other vectors are gram negative organisms like Escherichia coli, Klebsiella, Shigella, Salmonella and Pseudomonas [4,7,11,14,16]. Infections formed by anaerobic peptostreptococci, Staphylococcus epidermis, Group D and B streptococci are reported [12,14]. Anaerobic vectors are identified in 40% of cases; however, the place in the etiology is controversial and it is not recommended to start direct antibiotherapy for these vectors [8,9]. Abscess linked to Staphylococcus aureus may be observed especially in the periumbilical and perineal regions on the trunk as pustular and bullous lesions [4]. Symptoms, onset age and clinical findings are similar to infections linked to gram negative basilar and anaerobic vectors and staphylococcic infections. Cases infected with salmonella strains may have gastrointestinal findings observed [11]. Infants with subclinical mastitis may be restless and cry excessively and be diagnosed with infantile colic [17]. In our cases, the initial symptoms noticed by the family were redness and swelling of the two breasts. The patient was assessed in terms of galactorrhea due to discharge from the left breast. FSH, LH, E2 and prolactin levels were within normal limits.
Clinical assessment is the first stage of diagnosis. Ultrasonography is important for assessment of cases developing abscess especially. Abscess diagnosis may be made in the presence of fluctuation; however, fluctuation may not be observed in the presence of induration. The finding for mastitis on ultrasonography is increased echogenicity. Abscess provides findings of hyperechoic or hypoechoic avascular mass [18,19].
Gram staining and culture results direct treatment. If fluctuation is present, the abscess should definitely be drained. In situations without abscess, antibiotherapy alone is curative. Warm compresses may be beneficial. Initially, β lactamase-resistant anti-staphylococcal antibiotics should be chosen; however, in locations with high incidence of MRSA infection, vancomycin or clindamycin may be started. If gram negative basilar is observed on gram staining or if no microorganism is observed, and the infant has septic appearance, initial treatment should have aminoglycoside or cefotaxime added. In our case, due to the bilateral abscess and high infection symptoms, empirical vancomycin and cefotaxime treatment was begun intravenously. Cefotaxime treatment was stopped according to culture and antibiogram results and vancomycin continued. In most cases, 5-7 days of treatment is sufficient; however, treatment may be extended to 10-14 days according to the isolated vector, patient’s clinical status and presence of bacteremia.
The most common complication of neonatal mastitis is cellulitis observed at rates of 5-10%. Generally, itis localized; however, it may rarely spread to the shoulder and abdomen [2,10]. Other rare complications are fasciitis, osteomyelitis, meningitis, cerebral abscess and sepsis [2,4-6]. There is no definite data related to late period complications, but even in cases treated appropriately some cosmetic problems like scar development, hypoplasia and asymmetry may occur. It may cause problems with breast development in adolescent girls.
As a result, families should be informed about physiological breast hypertrophy and galactorrhea and mistaken interventions should be prevented.
Ethics Approval and Consent to Participate
Ethics approval not applicable but family consent obtained for the images.
Consent for Publication
Not applicable.
Availability of Data and Materials
Availability of data and material at Ordu University Training and Research Hospital.
Competing Interests
The authors declared no conflicts of interest with respect to the authorship and/or publication of this article.
Funding
The authors received no financial support for the research and/or authorship of this article.
Authors’ Contributions
EA planned the study, EA and EYE collected the data, patient follow up, HK Radıologıcal İmaging, O Abscess drainage and patient follow up. EA and EYE was a major contributor in writing the manuscript study.
Sainsbury R (2008) Mastitis of infants. Edward Arnold Ltd, UK. [ Ref ]
Walsh M, Mclntosh K (1986) Neonatal mastitis. Clin Pediatr 25: 395-399.[ Ref ]
Ramachandraiah A (2000) Neonatal mastitis. Indian paediatr 37: 1021.[ Ref ]
Rudoy R, Nelson JD (1975) Breast abscess during the neonatal period. A review. Am J Dis Child 129: 1031-1034. [ Ref ]
Bodemer C, Panhans A, Chretien-Marquet B, Cloup M, Pellerin D, et al. (1997) Staphylococcal necrotizing fasciitis in the mammary region in childhood: A report of ive cases. J Pediatr 131: 466-469.[ Ref ]
Manzar S (2001) Brain abscess following mastitis in a 3-month-old infant. J Trop Pediatr 47: 248-249. [ Ref ]
Efrat M, Mogilner JG, Iujtman M, Eldemberg D, Kunin J, et al. (1995) Neonatal mastitis diagnosis and treatment. Isr J Med Sci 31: 558-560. [ Ref ]
Stricker T, Navratil F, Sennhauser FH (2005) Mastitis in early infancy. Acta Paediatr 94: 166-169.[ Ref ]
Brook I(2002) Cutaneous and subcutaneous infections in newborns due to anaerobic bacteria. J Perinat Med 30: 197-208.[ Ref ]
Nelson JD (1973) Suppurative mastitis in infants. Am J Dis Child 125: 458-459. [ Ref ]
Brook I (1991) The aerobic and anaerobic microbiology of neonatal breast abscess. Pediatr Infect Dis J 10: 785-786.[ Ref ]
Dollberg S, Hurvitz H, Klar A, Engelhard D (1988) Group D streptococcal neonatal mastitis. Pediatr Infect Dis J 7: 362.
Arunagirinathan A, Duraipandian J, Rangasamy G, Shivekar S, Saban P, et al. (2011) Bilateral breast abscess in a neonate: A case report. IJCRI 2: 26-28.[ Ref ]
McKiernan J (1990) Breast enlargement in infants and children. Ir Med J 83: 88.[ Ref ]
Montalto M, Lui B (2009) MRSA as a cause of postpartum breast abscess in infant and mother. J Hum Lact 25: 448-450.[ Ref ]
Burry VF, Beezley M (1972)Infant mastitis due to gram-negative organisms. Am J Dis Child 124: 736-737. [ Ref ]
Rench MA, Baker CJ (1989Group B streptococcal breast abscess in a mother and mastitis in her infant. Obstet Gynecol 73: 875-877.) [ Ref ]
Brown L, Hicks M (2001) Subclinical mastitis presenting as acute, unexplained, excessive crying in an afebrile 31 day old female. Pediatric Emerq Care 17: 189-190. [ Ref ]
Borders H, Mychaliska G, Gebarski KS (2009) Sonographic features of neonatal mastitis and breast abscess. Pediatr Radiol 39: 955-958.[ Ref ]