Journal Name: Journal of Pediatrics and Infants
Article Type: Case Report
Received date: 10 August, 2018
Accepted date: 20 August, 2018
Published date: 08 September, 2018
Citation: Kachyrina D, Litosh V, Kaukenbaeva G, Bulegenova M (2018) Clinical case of Bean’s syndrome J Pediat Infants. Vol: 1, Issu: 2 (01-02).
Copyright: © 2018 Kachyrina D. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Hemangioma is a benign tumor, refers to vascular malformations that occur during embryogenesis. There is a combination of skin cavernous hemangiomas and mucosal lesions of the gastrointestinal tract, called Bean syndrome. This syndrome was described by American hematologist W. B. Bean, (1909-1989) as a kind variant of blue nevus syndrome: congenital multiple cavernous hemangioma of the skin and gastrointestinal tract. Bean’s syndrome is a rare and we did not meet in the available literature data on the disease outcome, efficacy of surgical treatment, mortality.
Keywords
Hemangioma, Tumor, Bean syndrome.
Abstract
Hemangioma is a benign tumor, refers to vascular malformations that occur during embryogenesis. There is a combination of skin cavernous hemangiomas and mucosal lesions of the gastrointestinal tract, called Bean syndrome. This syndrome was described by American hematologist W. B. Bean, (1909-1989) as a kind variant of blue nevus syndrome: congenital multiple cavernous hemangioma of the skin and gastrointestinal tract. Bean’s syndrome is a rare and we did not meet in the available literature data on the disease outcome, efficacy of surgical treatment, mortality.
Keywords
Hemangioma, Tumor, Bean syndrome.
Introduction
Hemangioma is a benign tumor, refers to vascular malformations that occur during embryogenesis. Under the influence of disembriogenetic factors the excess of the initial capillary set is not reduced and forms the rudiment of angiodysplasia [1].
There is also disseminated hemangiomatosis - systemic disease with localized hemangiomas, not only the skin but also the internal organs, the nervous system, which is often associated with bleeding and blood disorders even death. A type of disseminated hemangiomatosis is a combination of skin cavernous hemangiomas and mucosal lesions of the gastrointestinal tract, called Bean syndrome. This syndrome was described by American hematologist W. B. Bean, (1909-1989) as a kind variant of blue nevus syndrome: congenital multiple cavernous hemangioma of the skin and gastrointestinal tract.
Bean’s syndrome is rare, and we did not meet in the available literature data on the disease outcome, efficacy of surgical treatment, mortality. We present a clinical case of a child with the Bean’s syndrome.
Child A, 12 days old, was admitted to our center with a preliminary diagnosis: “congenital malformations. Kasabach-Merritt syndrome. Congenital hemangioma. Severe post-hemorrhagic anemia, thrombocytopenia”.
Medical history: heredity is not burdened. Mother denied professional bad habits. First pregnancy, first childbirth. Mom: At the first trimester mom had respiratory viral infection. Urgent delivery. The girl was born with a weight - 3694 g, 7-8 Apgar score.
Visually: pale skin. Multiple hemangiomas are defined on the upper, lower limbs, face. Hemangiomas of a pink color, with a purple tint in the middle, a different diameter from 0.2-0.5-0.8-1.0 sm, turning pale when pressed (Figure 1).
Figure 1: The arrows mark a large hemangioma in the left thigh and small hemangiomas across the body.
St. Localis: Lesion of the soft tissue palpated in the upper third of the thigh, the skin is bluish or purple color, painless. There are areas of the seal protruding above the surrounding tissue, turn pale when pressed.
Gastrointestinal bleeding occurred in the maternity hospital, and as the result anemia - (hemoglobin-97g/l), thrombocytopenia (49 x10 9/l). The child was transferred Scientific center of pediatrics and children surgery for further diagnosis and treatment.
Blood test: RBC- 2.9 x109/ l, Hb-77 g/l, Ht – 22%, WBC- 21 x109/ l, PLT-81.0 x109/ l, sedimentation ratio-2 mm/h.
Biochemistry - all parameters within reference norms.
Coagulation: APTT – 37 min., PTI – 85%, Fibrinogen – 2.5 g/l. Impairment of platelet aggregation (reduced aggregation with adrenaline) - 12,5% (N :50-80%). Chest X-ray, ECG, EEG – normal.
MRI: Small-cystic formations of the left hip, gluteal, inguinal and left lumbar region. Vascular malformation?
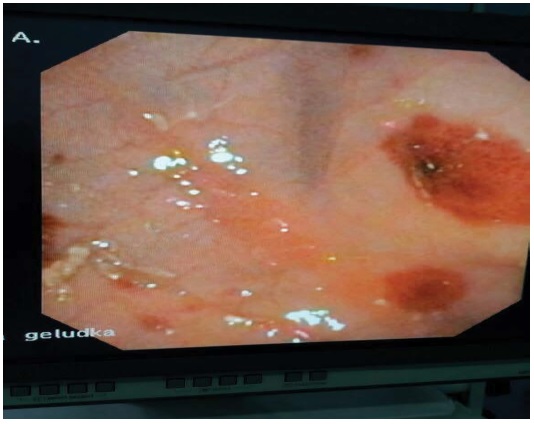
Fibro-esophagogastroduodenoscopy: hemangiomatous of the stomach and the jejunum (Figure 2).
Figure 2: Hemangiomatous of the stomach and the jejunum.
Colonofibroscopy - Hemangioma of the rectum and lower colon. Intestinal bleeding. (Figure 3).
Figure 3: Hemangioma of the rectum and lower colon.
During the time spent in the hospital, the child had repeated gastrointestinal bleeding in the form of hematemesis, melena and as a result the pronounced decrease in hemoglobin (60 g/l), platelets (18x109/l). For the health condition stabilization blood transfusions and transfusion of platelet concentrate have been performed.
The following treatment was prescribed: prednisolone (6 mg / kg / day) every other day + beta-blocker propranolol (3 mg / kg / day). gastrointestinal bleeding confined for a while that resulted in insignificant platelet increase. Improvement of the condition was observed for a week, but then relapses have repeated.
The active surgical interventions in the neonatal period was not appropriate. In 1.5 months, positive dynamics was observed. After stabilization of clinical and laboratory indicators the girl was discharged home. Currently child is an outpatient surgeon at the place of residence. According to the literature the main treatment of disseminated hemangiomatosis is combination of conservative treatment and surgical procedures, radiation therapy is available in older ages [2-4]. The prognosis is unfavorable.
There is no references