Journal Name: Journal of Pediatrics and Infants
Article Type: Research
Received date: 25 June, 2018
Accepted date: 28 June, 2018
Published date: 30 June, 2018
Citation: Hsieh P, Frazier JP, Oholendt K (2018) Parental Education in Debunking Myths: Is Fever Still a Phobia? J Pediat Infants. Vol: 1, Issu: 1 (37-43).
Copyright: © 2018 Hsieh P, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Importance: Although researchers recognize that fever misperceptions exist, education about fever has not been neither implemented nor documented. An innovated fever guide was developed to educate caregivers about fever and its treatment. Post-test results documented improvements in education/knowledge about fevers.
Objectives: To examine caregivers’ perceptions about fever and educated them on fever by providing educational handouts.
Design: A questionnaire including a pre and post-test was administered in a pediatric clinic from October 2013 to March 2014. Participants completed a questionnaire concerning their knowledge about fever and its management. A “Fever Guide” was then given to caregivers to read on fever facts. After reading the guide and their doctor’s visit, a post-test was administered on the knowledge gained from the “Fever Guide”.
Setting: The questionnaire was administered in a pediatric clinic associated with the Department of Pediatrics, UTHealth McGovern Medical School at Houston, Texas. This clinic provides medical services to medically underserved, lower socioeconomic populations in the greater Houston area. The populations served at this site are predominately Hispanics and African Americans.
Participants: Using a convenience sample of families, a total of 500 caregivers voluntarily participated in this study.
Results: Data were collected on 500 caregivers in a general pediatric clinic associated with the Department of Pediatrics, UTHealth McGovern Medical School. Pre-test showed that 29% of the caregivers did not know what an average body temperature should be and 69% believed a child had a high fever if the body temperature was 101° F. In addition, 70% of caregivers indicated that they were very worried when their children had fever and 46% of the caregivers indicated that fever could cause several complications and could result in death. Through education (Fever Guide), post-test results indicated an increase in knowledge from 5% (pre-test) correct to 33% (post-test) correct fever knowledge questions.
Conclusions: Patient-centered care requires evaluating and treating the patient while providing patients and their caregivers’ accurate knowledge/education on methods for fever management. Caregivers may use the information to make sound decisions on proper fever management.
Keywords
Patient care, Pediatric clinic, Fever.
Abstract
Importance: Although researchers recognize that fever misperceptions exist, education about fever has not been neither implemented nor documented. An innovated fever guide was developed to educate caregivers about fever and its treatment. Post-test results documented improvements in education/knowledge about fevers.
Objectives: To examine caregivers’ perceptions about fever and educated them on fever by providing educational handouts.
Design: A questionnaire including a pre and post-test was administered in a pediatric clinic from October 2013 to March 2014. Participants completed a questionnaire concerning their knowledge about fever and its management. A “Fever Guide” was then given to caregivers to read on fever facts. After reading the guide and their doctor’s visit, a post-test was administered on the knowledge gained from the “Fever Guide”.
Setting: The questionnaire was administered in a pediatric clinic associated with the Department of Pediatrics, UTHealth McGovern Medical School at Houston, Texas. This clinic provides medical services to medically underserved, lower socioeconomic populations in the greater Houston area. The populations served at this site are predominately Hispanics and African Americans.
Participants: Using a convenience sample of families, a total of 500 caregivers voluntarily participated in this study.
Results: Data were collected on 500 caregivers in a general pediatric clinic associated with the Department of Pediatrics, UTHealth McGovern Medical School. Pre-test showed that 29% of the caregivers did not know what an average body temperature should be and 69% believed a child had a high fever if the body temperature was 101° F. In addition, 70% of caregivers indicated that they were very worried when their children had fever and 46% of the caregivers indicated that fever could cause several complications and could result in death. Through education (Fever Guide), post-test results indicated an increase in knowledge from 5% (pre-test) correct to 33% (post-test) correct fever knowledge questions.
Conclusions: Patient-centered care requires evaluating and treating the patient while providing patients and their caregivers’ accurate knowledge/education on methods for fever management. Caregivers may use the information to make sound decisions on proper fever management.
Keywords
Patient care, Pediatric clinic, Fever.
Introduction
The fear of fever is often due to a lack of understanding and knowledge. Several studies show that caregivers often have anxiety about fevers because of misperceptions of what it is and what it can do to the body [1-5]. Parents often view fever as a disease that can harm their children [1]. The term “fever phobia” was coined in 1980 by Dr. Barton Schmitt to describe the fears and misperceptions that parents hold about fevers [1]. As a result of the fear and misinformation, children are administered unwarranted fever reducers and it is the most common reasons for clinic and unnecessary pediatric emergency department visits [3,6]. As suggested by researchers in this area, healthcare providers may exacerbate fever phobia by holding misperceptions about fevers and its management, resulting in passing such misconceptions and treatment plans to caregivers [7]. In addition, physicians may also take unnecessary steps to reduce fever though literature might suggest otherwise [8].
Providing patient-centered quality care is critical in meeting the needs of patients in the clinical setting. Not only do patients need patient-centered care, the quality of communication and education received while at the clinic visit is also important. Sklar [9] suggest, it is important to provide materials for patients to enable families to make sound decisions when caring for their family members and themselves.
While it is evident that people still hold misperceptions about fever, resulting in fever phobia, merely identifying the myths without educating caregivers is doing the patients a disservice.
The purposes of this paper were to examine patient caregivers’ perceptions or misperceptions about fever, to educate them on fever by providing educational handouts, and to examine if caregivers have a more accurate knowledge about fever and fever management after reading the educational handout.
Methods
Participants
A cross-sectional questionnaire including a pre and posttest using a convenience sample of families was administered by medical staff between October 2013 and March 2014 in a general pediatric clinic associated with the Department of Pediatrics, UTHealth McGovern Medical School at Houston, Texas. This clinic provides medical services to medically underserved, lower socioeconomic populations in the greater Houston area. The populations served at this site are predominately Hispanics and African Americans. Verbal consents were obtained from caregivers before being asked to complete the questionnaire.
Upon receiving verbal consent from caregivers, families were asked to complete a 2-page questionnaire and pre-test concerning their knowledge, beliefs, and attitudes towards fever as well as fever management and demographic information. A “Fever Guide” was then given to the families to read on fever facts and management prior to the doctor’s visit. After the doctor’s visit, a post-test was given to test the knowledge gained from the “Fever Guide”.
The Committee for the Protection of Human Subjects Office of Research Support Committees reviewed this research and determined the project qualified and approved for exempt status.
Instrument
With permission from Crocetti et al [3]. who conducted the earlier fever studies, we adapted questions used on the 2-page questionnaire fever study. The first fourteen questions included demographic information: age, gender, type of visit, ethnicity, method of payment, highest education level completed, who brought the patient to the clinic visit, number of children in household, and the age of the oldest and youngest child in the household. In addition, questions about the visit and whether the patient had a fever complaint and if so; how the temperature was measured, how it was taken, and what type of fever measuring instrument was used. The pre-test questionnaire included 15 questions that gathered information on fever knowledge (7 questions) and steps caregivers would take to treat/manage a fever (8 questions). Upon completion of the pre-test, caregivers were given a one page “Fever Guide” handout to read. The “Fever Guide” handout detailed information as follows: What is the normal body temperature ranges? What temperatures constitute a fever (low-grade, common fever, high-grade fever)? When to call the doctor, and how to accurately manage a fever and care for a febrile child at home. Caregivers were asked to complete a post-test consisting of four questions to test their knowledge gained from reading the “Fever Guide” informational handout. The caregivers kept the “Fever Guide” and returned the questionnaire, pre- and post-test to the nursing staff before leaving the clinic visit.
Data Analysis
Descriptive statistics were conducted to summarize the frequencies and percentages for the demographics variables. MANOVA was also run to examine group differences. Data were analyzed using the Statistical Package for the Social Sciences (SPSS version 21).
Results
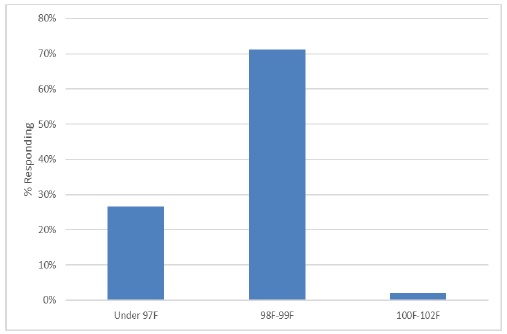
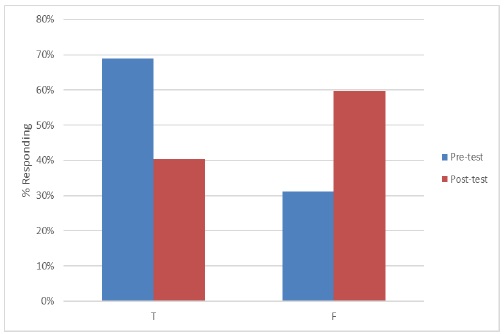
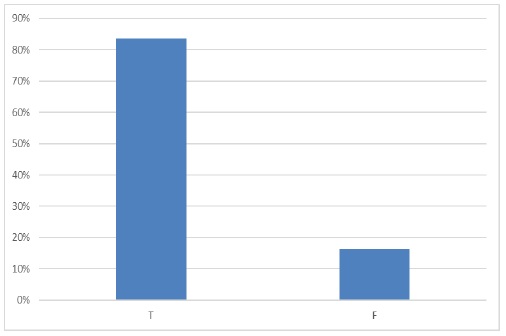
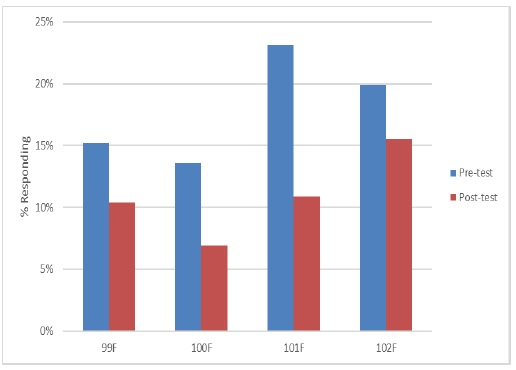
A total of 500 families participated in this study, with 430 mothers (90.5%), 27 fathers (5.7%), and 15 grandparents (3.2%). A majority of the participants was African American (70.1%), followed by Hispanic (20.2%), then Caucasian (6.6%), and Asian (.6%). Other demographic information is presented in Table 1. The pre-test questions (knowledge about fever) showed that 26.6% of the caregivers believed the average body temperature should be below 97° F and 2% believed it should be above 100° F (Figure 1). Most caregivers (68.9%) believed a child has a high fever if the body temperature was 101° F (Figure 2) and the majority of caregivers (83.7%) would take their child to an emergency room if the child’s body temperature was between 101° F and 103° F (Figure 3). Results indicated 16.2% of caregivers believed fevers could cause seizure, 8.8% believed fever could cause brain damage, and 46% of the caregivers indicated that fever could cause several complications at once (Table 2). In addition, 19.4% of caregivers reported that fever could last up to a week. When asked about treatment of fever, 41.9% of the caregivers would take their child’s temperature every two hours and 34% of caregivers would take their child’s temperature every hour. The most common method participants took their child’s temperature was under the arm (29.6%) and 68.3% would awaken their child at night to administer fever reducing medicine (Table 3).
Table 1: Demographic Information.
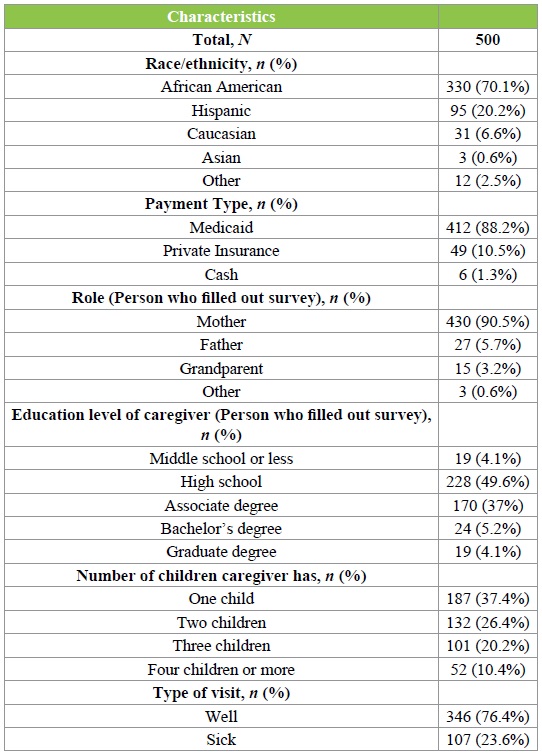
Table 2: Harmful Effects of Fever (Pre-test).
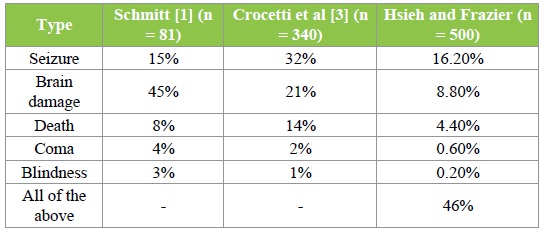
Table 3: Responses to how caregivers treat children with fever.
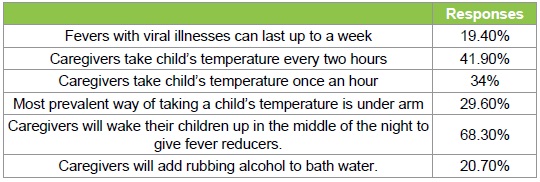
Figure 1: Caregivers’ perception of body’s average temperature.
Figure 2: Caregivers’ perception of what constitutes a high fever. (Your child has a high fever if his/her body temperature is 101°F).
Figure 3: Caregivers’ perception of when to bring child to emergency room. (You should bring your child to the emergency room if his/her body temperature is between 101°F and 103°F).
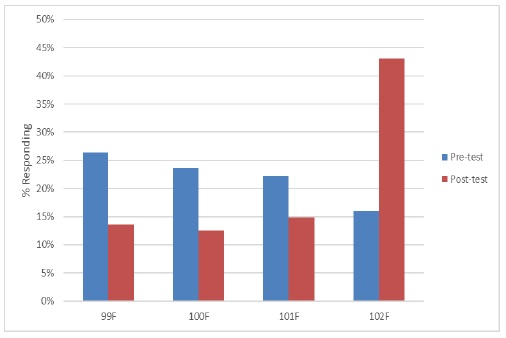
Caregiver’s responses to knowledge about fever before and after reading the fever guide is compared in Table 4 and illustrated in Figures 4,5 and 6. Prior to reading the fever guide, 72.2% of caregivers would administer fever reducers when the child’s temperature was between 99° F and 101° F. After reading the fever guide, 40.9% of caregivers would administer fever reducers when child’s temperature was below 101° F (Figure 4). Prior to the Fever Guide education, 51.9% of caregivers would call their pediatrician when the child had a temperature between 99 and 101° F. After the Fever Guide education, 28.2% would call their pediatrician when their child had a temperature below 101° F (Figure 5).
Table 4: Responses to knowledge about fever questions (Pre and Post-test differences).
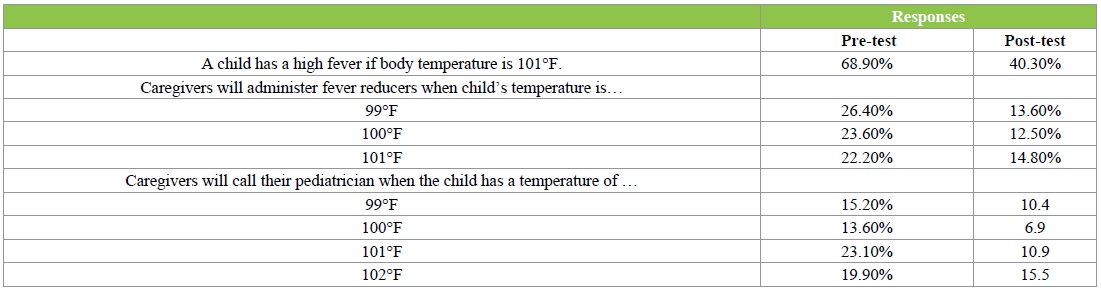
Figure 4: At what temperature should you give your child Acetaminophen?
Figure 5: At what temperature should you call your child’s doctor?
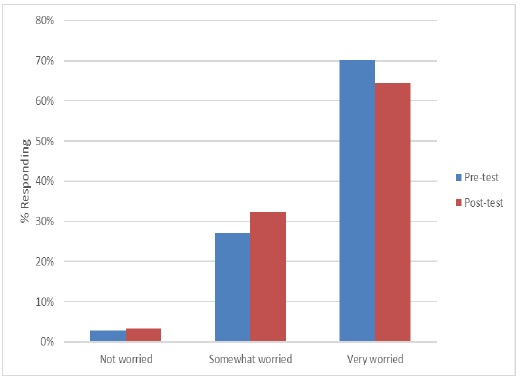
Figure 6: Caregivers’ anxiety over fever.
Additionally, before participants were given the Fever Guide, 70.1% indicated they were very worried when their child had a fever, 27.1% indicated that they were somewhat worried, and only 2.8% indicated that they were not worried at all. Although post-test indicated that after reading the fever guide, caregivers were still very worried about fever (64.4%), their knowledge about fever improved and the steps they took to manage a fever was more accurate. Caregivers’ perception of “high fever” changed as a result of the education. Prior to Fever Guide education, 68.9% of caregivers believed that a child had a high fever if their body temperature was 101° while only 40.3% held that belief after education. Overall, results indicated that there was an increase in knowledge about fever, from 5% of the participants answering the pre-test questions on fever knowledge to 33% of participants after reading the “Fever Guide” and answering the post-test questions.
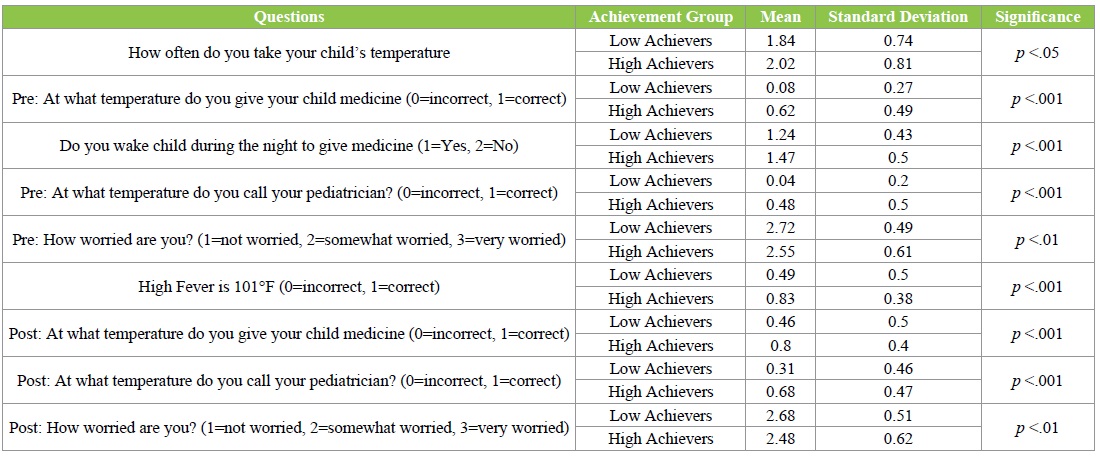
MANOVA was run for “high” and “low” achievement groups (the independent variable) based on how well participants scored on the seven pre-test questions regarding their knowledge about fever. The groups were identified using median split. Significant differences were found in the steps they took to treat/manage fevers, F (10, 350) = 33.32, p <.001, partial η² =.49. No significant differences were found between caregivers’ levels of education.
Results indicated that caregivers who scored lower on the pre-test took child’s temperature significantly more often than caregivers, who scored higher on the pre-test, F (1, 359) = 4.49, p <.05, partial η² =.01. The caregivers who scored lower on the pre-test also held significantly more myths about fever and managed fever incorrectly. This included administering fever reducers when it was not necessary, F (1, 359) = 182.02, p <.001, partial η² =.34, waking the child up to give medication during the night, F (1, 359) = 20.90, p <. 001, partial η² =.06, and calling the child’s doctor when the fever is considered a low-grade fever, F (1, 359) = 140.20, p <.001, partial η² =.28. Results indicated that caregivers who scored lower on the pre-test were more prone to worry when their child had a fever, F (1, 359) = 8.62, p <.01, partial η² =.02. In addition, there were statistically significant differences in accuracy of the posttest questions between high and low achievers. Means and standard deviations are included (Table 5).
Table 5: Differences in the responses for high and low achievement groups.
Discussion
Fever is defined as “a rise of body temperature above the normal” [10]. However, without educating parents and other caregivers, the definition of “normal” temperature may lead to misinterpretation among caregivers. Our study result shows 26.8% caregivers did not have knowledge of what value was a “normal “temperature. May et al [11] reported the definition of high fevers was never discussed during sickchild visits by 10% of the providers. Frequently, there may be parental/physician mixed messages when a child with fever is seen for a sick visit. The parental priority is focused on the fever symptom and fears of the harm that fever may cause, which initiates the clinic visit. On the other hand, the priority for the physician is often to establish the cause/diagnosis for the fever in determining if this is a viral or more serious bacterial infection [12,13]. Because of these divergent focus points, educating parents on fever physiology, the body’s responses to fever, mechanisms to fight against infection, and the beneficial effects of fever often gets lost in the translation of the illness and the visit in a busy pediatric practice setting [14-16]. Parental fears prevail when caregivers are caring for a sick/febrile child. Emphases are placed on the interventions required to relieve the fever symptom. As a result of this mindset, for many parents, lowering a child’s body temperature by giving fever reducers becomes the first step to take and the initiation of an antibiotic may become the expectation when visiting the treating physician [17]. The discussion on fever physiology and what is a normal temperature and when and how to manage fever becomes marginalized or presumed to be understood. At this point, when more emphasis has been placed on management of a diagnosis (viral vs. bacterial) instead of a fever symptom the parent or caregiver assumes the fever will get better and resolve because an antibiotic was given. Caregivers may believe fever is a sign of serious infection and many may demand treatment with an antibiotic. Parents or caregivers leave the visit with instructions on treating the diagnosis and less often educational materials on what is a normal vs. an abnormal temperature, fever management and fever control measures. Many of the parents (68.9%) in this study believed a high fever was a body temperature of 101° F and 83.7% would take their child to an emergency room if the temperature was between 101° F and 103° F. Anxious caregivers managing a febrile child are often fearful and react by rushing to the emergency center [7]. There is continued confusion in the literature and lack of consensus among physicians regarding the optimal approach to management of young febrile infants [18-21].
Many caregivers are unaware of the beneficial effect of fever and believe fevers will continue to rise or persist if left untreated. Almost 20% of the caregivers in our study believed fevers lasting up to a week could result in seizures (16.2%) or lead to brain damage (8.8%). Overall, in our study, caregivers believed that fever could cause neurological life-threatening harmful events (25.8%) and even death (4.4%). Caregivers need education to be aware that the human body responses do not allow temperatures to rise to dangerous levels unless there are conditions that exist in the body to damage or short circuit the regulatory hyperthermic body controls [14]. Fever phobia continues to evoke a powerful response from caregivers to do something. This unwarranted anxiety usually leads to over-monitoring and /or over-use of antipyretics with possibly other modes (alcohol baths) for reducing fevers.
The caregivers in our study have the perception that a rise in body temperature warrants a visit to the emergency department and that fever can do harm to the body. Over 75% of caregivers would check temperature every 2 hours or less when their child had a fever, 72.2% would administer fever reducers when their child’s temperature was 101° F or less, 26.4% would even administer fever reducers when the child’s temperature was merely 99° F, 68.3% would awaken their children at night to administer fever reducers and 20.7% caregivers also report adding rubbing alcohol to bath water. The fact that alcohol can lead to hypoglycemia in young children must be conveyed to caregivers so that children will not be harmed by ineffective treatments used for fever control.
Pre-test, fifty-two percent of caregivers would call their pediatrician when their child had a temperature from 99° F to 101° F; however, 19.9% would wait until the temperature was 102° F. This signifies the level of anxiety caregivers have with the symptom fever and calling their physician at any time may help to relieve some of their fears. Caregivers who were surveyed say most of their after hour calls visits and calls were often to pediatric emergency departments [22]. Demonstrated in this study, poor management of fever and anxiety secondary from fever may be avoided when education is provided to caregivers.
Our study provided fever knowledge pre-test for parents to take at the beginning of the clinic visit. Afterward, a one-page “Fever Guide” was given to caregivers with information on normal /abnormal body temperatures, what temperatures constitute a fever, what temperatures may warrant antipyretics and finally helpful hints on measures to help take care of the febrile child. Also, general information on fever control included advice such as offering lots of fluids, wearing less clothing, limiting medicines if temperature is less than 102° F and the child is comfortable. Avoid aspirin and rubbing alcohol and finally when to call the doctor. After reading the “Fever Guide” and at the end of the visit a fever knowledge test was administered as a post-test. Caregiver’s post-test responses to a child with a high fever of 101° F were (40.3%) vs pre-test response of (68.9%). Caregivers would administer fever reducers when a child’s temperature was from 99-101° F post-test (40.9%) vs. pre-test (72.2%).
The current study is a descriptive trend analysis of caregivers’ perception about and management of fever. From the results of this study, it is evident that parental behaviors have not changed significantly since reported by Crocetti et al [3] 14 years ago. This is alarming because while emphasis is placed on a child’s temperature when obtaining a history about child’s sickness, not enough emphasis is placed on defining high fever. The reason it is important to understand fever is because “fever phobia” is common, leading to unnecessary anxiety, treatments, and doctors’ visits. Caregivers need to be educated that fever may benefit a sick child, as the rise in body’s temperature stimulates the immune system and is a way for the body to fight infection [23].
The question arises why these behaviors persist. Are outside pressures in a busy pediatric clinic limiting the time physicians have in educating caregivers on fever and general fever control information? Because of these and probably other unforeseen reasons caregivers have expectations fueled from fever phobia that leads to not only aggressive, unwarranted treatment of the febrile child but many disruptive nights for the child, child’s caregivers as well for the physician.
For more than 30 years since the study conducted by Schmitt [1], physicians have developed the awareness that fever phobia exits. However, there has neither been documentation of patient education on fever nor research on increasing knowledge about fever through education. Therefore, the present study offers several strengths. With the realization that fever phobia exists and as reported by Poirier [7] poor management of fever is frequent, we have provided education to caregivers through the Fever Guide created. Results indicated that overall, there was an increase in caregivers’ knowledge about fever and fever is more accurately managed, despite continued concerns about fever harming children. More education on what fever is and on its management is crucial. The Fever Guide was a valuable educational tool for the caregivers, however direct medical counseling provided to caregivers on the definition of fever and fever management are warranted.
This study is especially innovative because in addition to surveying caregivers’ beliefs, and treatment of fever, we made an attempt to educate the caregivers by giving them an educational handout in which describes what constitutes a fever, high fever, and ways to manage children with fever. With this information, it is hoped that caregivers will gain knowledge on the topic and manage fevers appropriately instead of possibly giving excessive fever reducing medicines or making unnecessary trips to the emergency room. It is important to remind caregivers that a child’s symptoms and not merely a temperature above “normal” is worrisome.
Conclusion
This study post-test “Fever Guide” education handout shows that caregivers would reduce administering fever reducers by 31.3% and increase ability to identify what is a high fever by 28.6%. Caregivers will continue to be concerned and frightened when their children are sick. However, with proper education of what is a fever, guidance on the proper steps to take in managing a fever, and guidelines on when to notify the physician the caregivers will have some knowledge and possibly gain some level of comfort. Physicians need to continue to provide those clinic opportunities to inform, educate, and deliver real time information at the time of the visit with long term educational, meaningful tools. Whereby, caregivers’ anxiety about the potential harmful effects of fever can be decreased through education, as seen in this study.
In conclusion, patient-centered care is not only showing respect by putting patients’ and caregivers’ needs paramount in a busy clinical setting. Patient-centered care is also educating patients and their caregivers so that they have a better understanding of fevers in order to make sound decisions on properly recognizing and managing fevers.
Author Contributions
Dr. Hsieh had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analyses. All authors read and approved the final manuscript.
Dr. Hsieh conceptualized and designed the study, questionnaire, and fever guide. She also carried out the statistical analyses and drafted the manuscript.
Dr. Frazier designed the questionnaire and modified the fever guide. Dr. Frazier also coordinated and supervised data collection, assisted in drafting the initial manuscript, and reviewed the final manuscript. Dr. Frazier was the content expert on the team.
Dr. Oholendt was responsible for acquisition of data, data entry, in addition to critically revising and approving the manuscript.
Funding Source
No funding was secured for this study.
Financial Disclosure
Authors have no financial relationships to disclose.
Conflict of Interest
Authors have no conflicts of interest to disclose.
Schmitt BD (1980) Fever phobia: Misconceptions of parents about fevers. Am J Dis Child 134: 176-181. [ Ref ]
Kramer MS, Naimark L, LeDuc DG (1985) Parental fever phobia and its correlates. Pediatrics 75: 1110-1113. [ Ref ]
Crocetti M, Moghbeli N, Serwint J (2001) Fever phobia revisited: have parental misconceptions about fever changed in 20 years? Pediatrics 107: 1241-1246. [ Ref ]
Al-Nouri L, Basheer K (2006) Mothers’ perceptions of fever in children. Journal of Tropical Pediatrics 52: 113-116. [ Ref ]
Wallenstein MB, Schroeder AR, Hole MK, Ryan C, Fijalkowski N, et al. (2013) Fever literacy and fever phobia. Clinical Pediatrics 52: 254-259. [ Ref ]
Adam D, Stankov G (1994) Treatment of fever in childhood. Eur J Pediatr 153: 394-402. [ Ref ]
Poirier MP, Davis PH, Gonzalez-del-rey JA, Monroe KW (2000) Pediatric emergency department nurses’ perspectives on fever in children. Pediatr Emerg Care 16: 9-12. [ Ref ]
Klugar MJ, Ringler DH, Anver MR (1975) Fever and survival. Science 188: 166-168. [ Ref ]
Sklar DP (2013) Delivery system reform: Visualizing the future. Academic Medicine 88: 905-906. [ Ref ]
Mackowiak PA (2000) Physiological rationale for suppression of fever. Clin Infect Dis 31: S185-S189. [ Ref ]
May A, Bauchner H (1992) Fever phobia: The pediatrician’s contribution. Pediatrics 90: 851-854. [ Ref ]
Caviness AC, Demmler GJ, Almendez Y, Selwyn BJ (2008) The prevalence of neonatal herpes simplex virus infection compared with serious bacterial illness in hospitalized neonates. J Pediatr 153: 164-169. [ Ref ]
Byington CL, Enriquez FR, Hoff C, Tuohy R, Taggart EW, et al. (2004) Serious bacterial infections in febrile infants 1 to 90 days old with and without viral infections. Pediatrics 113: 1662-1666. [ Ref ]
Adam HM (1996) Fever and the host responses. Pediatr Rev 17: 330- 331. [ Ref ]
Kluger MJ (1992) Fever revisited. Pediatrics 90: 846-850. [ Ref ]
Kluger MJ (1991) Fever.Role of pyrogenes and cryogenes. Physiol Rev 71: 93-127. [ Ref ]
Kramer MS (1997) Management of the young febrile child. a commentary on recent practice guidelines. Pediatrics 100: 128-134. [ Ref ]
Goldman RD, Scolnik D, Chauvin-Kimoff L, Farion KJ, Ali S, et al. (2009) Practice variations in the treatment of febrile infants among pediatric emergency physicians. Pediatrics 124: 439. [ Ref ]
Bergman DA, Mayer ML, Pantell RH, Finch SA, Wasserman RC (2006) Does clinical presentation explain practice variability in the treatment of febrile infants? Pediatrics 117: 787-795. [ Ref ]
Pantell RH, Newman TB, Bernzweig J, et al. (2004) Management and outcomes of care of fever in early infancy. JAMA 291: 1203-1212. [ Ref ]
Baraff LJ (2000) Management of fever without source in infants and children. Ann Emerg Med 36: 602-614. [ Ref ]
Poirier MP, Collins EP, McGuire E (2010) Fever phobia: a survey of caregivers of children seen in a pediatric emergency department. Clin Pediatr 49: 530-534. [ Ref ]
Roberts NJ (1991) Impact of temperature elevation on immunologic defenses. Rev Infect Dis 13: 462-472. [ Ref ]