Journal Name: Journal of Pediatrics and Infants
Article Type: Systemic Review
Received date: 09 February, 2021
Accepted date: 01 March, 2021
Published date: 08 March, 2021
Citation:Suzuki H, Kato M, Shinozaki K, Lopes KS, Ota E (2021) Systematic Review of the Effectiveness of Aromatherapy in Labor. J Pediat Infants Vol: 4, Issu: 1 (58-70).
Copyright: © 2021 Suzuki H et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Background: Clinical practice with aromatherapy has become an expanding area for nursing, and is considered one of the most popularly used complementary treatments. However, there is insufficient evidence about the benefits of aromatherapy for pain management and other related discomforts in labor. We aimed to evaluate the effects of aromatherapy for women during delivery particularly for pain relief.
Methods: AMED, ClinicalTrials.Gov, CINAHL, Cochrane Library, EMBASE, MEDLINE, PubMed, and WHO ICTRP were searched in August 2017. For updates, these databases were searched from July 2017 to July 2018. This study included randomized controlled trials (RCTs) and quasi-RCTs for normal pregnancy women who were experiencing labor onset, and compared aromatherapy with standard care or control.
Results: Six RCTs from six reports, and four quasi-RCTs from five reports were included (1238 pregnant women). The trials found significant difference between groups for the primary outcomes of pain relief on the latent (MD -1.56, 95%CI: -2.45 to -0.67, low certainty of evidence) and early active phase (MD -1.69, 95%CI: -2.50 to -0.89, low certainty of evidence). However, there were no significant differences for the primary outcomes of pain relief on the late active phase, and anxiety relief on the early and late active phases.
Conclusion: This meta-analysis found evidence that the use of inhalation aromatherapy for term pregnancy women is associated with reduction of labor pain. However, there is insufficient evidence to confirm pain relief on the late active phase, anxiety relief, and other outcomes following aromatherapy.
Keywords: Aromatherapy, Labor pain, Anxiety, Complementary Therapies.
List of Abbreviations
RCTs-Randomized control trials; MD-Mean difference; SMD-Standardized mean difference; CI-Confidence interval; SD-Standard deviation; RR-Risk ratio; ITT-Intention-to-treat; GIVMGeneral inverse variance method; RevMan-Review Manager; VAS-Visual Analogue Scale; NRS-Numerical Rating Scale; STAI-Spielberger’s StateTrait Anxiety Inventory; VASA-Visual Analog Scale for Anxiety
Background
Although labor and birth are considered to be a natural process, laboring women experience a significant amount of discomfort and pain as well as a variety of other challenging sensations [1]. Women in labor experience pain caused by uterine contractions, expansion of the lower uterus, and the dilation of the cervix. Moreover, pain is produced by the stretching of the vagina and pelvic floor to accommodate the baby. These complexes of pain can lead to complications such as a compromised immune system, reactive hypoglycemia, delayed wound healing, increased myocardial oxygen consumption, paralytic ileus, and reduced respiratory function [2]. This pain possibly exerts its effects in the form of psychological distress to both the mother and the baby. Perceptions of labor pain vary by the individual and are influenced by a variety of physiologic, psychologic, emotional, socio-cultural, and environmental factors [1]. Labor, without using drugs or invasive methods such as an epidural, is often sought by many women and they usually turn to complementary therapies such as aromatherapy to help reduce their pain perception [3].
Aromatherapy is the use of essential oils from plants such as flowers, trees or herbs. These essential oils improve physical, mental, and spiritual well-being. The clinical practice with aromatherapy has become an expanding area for nursing and is considered one of the most popularly used complementary therapies [4]. Aromatherapy during labor and delivery may provide relaxation and reduce pain [5]. Several essential oils used in aromatherapy have been suggested to have antistressor, antidepressive, and relaxation effects. In addition to reducing pain, aromatherapy may also decrease symptoms such as anxiety, nausea, vomiting and other labor-related conditions [6].
To date, there has been inconclusive evidence regarding the benefits of aromatherapy for the management of pain and other related discomforts in labor, as well as for the improvement of maternal and neonatal outcomes. A previous Cochrane systematic review on aromatherapy published in 2011 could not clearly show evidence of its effects on pain relief during deliveries [3]. The most recent systematic review, which was published in 2019, reported the anxiolytic effects of aromatherapy, and suggested positive effects on anxiety during the first stage of labor [7]. This 2019 review analyzed the efficacy of individual aroma essence oils in the first stage of labor, and it included studies of aromatherapy intervention using other care methods such as massage. We concluded that aromatherapy results may be influenced by other factors.
We believe that a meta-analysis is needed to definitively evaluate the efficacy of inhalation aromatherapy in terms of all its outcomes, particularly for pain management by excluding cointervention, which may affect its efficacy. The purpose of this systematic review is to evaluate the efficacy of aromatherapy for women in all stages of labor.
Methods
We followed the Cochrane Handbook and Cochrane’s MECIR for conducting the search, PRISMA guidelines for reporting the search, and PRESS guidelines for peerreviewing the search strategies [8-11]. We registered the study protocol with PROSPERO (CRD42017077617).
Selection criteria
We included all types of randomized controlled trials (RCTs) involving pregnant women of 37-42 gestation weeks and with labor onset. The included RCTs must be focused on inhalation of any kinds of aroma essence compared with the standard care or placebo. We included multiple arms and cointervention, which were available to compare the efficacy of aromatherapy. The primary outcomes were pain relief and anxiety relief during labor. The secondary outcomes were duration of delivery, duration of contraction, spontaneous or operative delivery, and Apgar score.
Search strategy
In August 2017, we searched AMED, ClinicalTrials.Gov, CINAHL, Cochrane Library, EMBASE, MEDLINE, PubMed, and WHO ICTRP with no date/time, language, document type, and publication status limitations. For the present review, these databases were searched from July 2017 to July 2018. We also hand searched Google scholar in August 2018.
Data extraction
KS, MK, and HS independently screened and confirmed study eligibility. When there were conflicts of eligibility, each study was discussed with HS and EO. We found several papers written in Persian, and we attempted to contact to the authors. However, we received no reply. From each study, KS extracted information on characteristics of participants, study design, numbers of participants, interventions, and outcome data. Data were extracted by HS and checked by MK. Risk of bias was assessed as recommended in the Cochrane Handbook, and MK and HS independently assessed each trial. Any discrepancies were resolved through discussion. MK and HS also contacted the authors of three RCTs to request unpublished outcome data, where trial reports implied that relevant data might be available. However, replies were not forthcoming [8,12-14].
Statistical analysis
We performed meta-analysis to analyze pooled outcome data. We estimated weighted mean difference (MD) when the outcomes were measured similarly between trials. We also used standardized mean difference (SMD) to combine trials that measured the same outcome with different methods, and 95% confidence interval (CI) for continuous outcomes. If multiple intervention arms were reported, we combined the data of aromatherapy intervention groups and calculated mean and standard deviation (SD). When cointervention was used, we analyzed the compared data of aromatherapy and controlled to avoid the effects of other interventions. For binary outcomes (e.g., response, remission, and dropouts), we estimated risk ratio (RR) and 95% CI for each comparison using the numbers randomly assigned and numbers of events. We used intention-to-treat (ITT) data in this analysis, as ITT data are less biased and address a more pragmatic and clinically relevant situation. To address missing data, we used the number randomized minus any participants for the denominator for each outcome in each trial. We used general inverse variance method (GIVM) when the included studies reported only the difference between the means for the two groups and the standard error of this difference. We included outcome data from quasi-RCTs. We carried out sensitivity analysis to explore the effect of trial quality assessed by quasi-RCTs, concealment of allocation and incomplete outcome data, or more than one, with quasiRCT studies being excluded from the analysis to assess whether this makes any difference in the overall result. Heterogeneity was assessed using I² statistic. We considered I² ≥ 60% as high, then we used random effects meta-analysis. For low to moderate heterogeneity (I² < 60%), we used fixed effects meta-analysis.
We performed all analyses using Review Manager (RevMan) [15]. We used GRADE to judge the certainty of evidence for the effectiveness of aromatherapy for the primary outcomes such as labor pain relief and anxiety relief through all the stages of labor [16].
Results
Trial characteristics
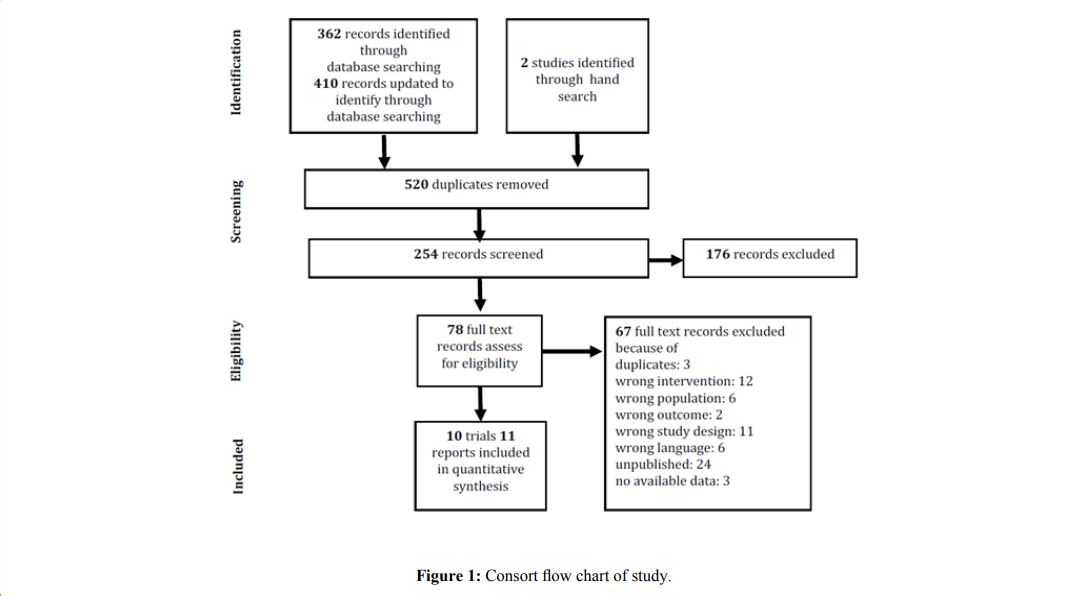
We screened 254 titles and abstracts (Figure 1), and identified six individual RCTs from six reports and four quasi-RCTs from five reports for inclusion in the final review [17-27]. We excluded the trials with massage and bathing as these have other effects. Eight studies that were included mentioned that blinding of participants was not possible because of the diffusion of oil molecules in the air [17,19-22,25-27]. For this reason, five reports had performed interventions on randomly allocated days with the aromatherapy days and the placebo days. Although we considered these four trials as quasi-RCTs, we included these four trials from the nature of the intervention [17,20,21,23,24].
Table 1 provides details of the included studies involving 1238 pregnant women at labor onset [17-27]. Eight trials included only nulliparous women (81.0%), one trial did not report parity (8.9%), and one trial showed the mean ± SD of the numbers of parity 1.31 ± 0.72 for the intervention group and 1.22 ± 0.91 for the control group (9.6%) [17-27]. All of the trials recruited participants with singleton pregnancy and full-term pregnancy, and did not report existing medical conditions. Most trials recruited predominantly adults (18- 35 years old) with cephalic presentation and 3-4 cm cervical dilatation. Nine trials were undertaken in Iran and only one was conducted in Thailand [26]. All of the trial settings were at hospitals [17-25,27].
For the measurement of outcomes, labor pain severity was measured using the Visual Analogue Scale (VAS) chart and the Numerical Rating Scale (NRS) [17-21,24,26,27]. Both scales have a score range of 0 to 10 [28,29]. One trial reported the pain score changes from baseline therefore we performed GIVM for the meta-analysis [26]. In three studies, Spielberger’s State-Trait Anxiety Inventory (STAI) was used to determine the level of anxiety of the participants [18,23,25]. STAI questionnaires consist of 40 questions in which the scores ranged from 20 to 80. Higher scores indicate greater anxiety [30]. The reliability of STAI has a Cronbach’s alpha of 0.90 [25]. One study used the Visual Analog Scale for Anxiety (VASA) [22]. The scale ranges from 0 to 10 with 0 indicating no anxiety and 10 greatest anxiety [31].
Figure 1:Consort flow chart of study.
Risk of bias for included studies
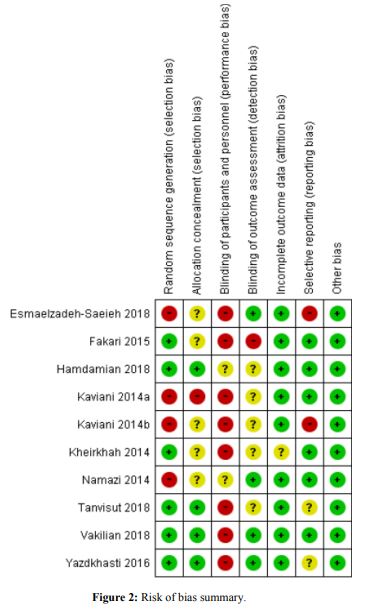
Of the 10 trials, most of the trials had a low risk of bias in random sequence generation (60%, 6/10), incomplete outcome data (90%, 9/10), selective reporting (60%, 6/10), and other bias (100%, 10/10). However, most of the trials had a high risk or unclear bias in allocation concealment (60%, 6/10), blinding of participants and personnel (100%, 10/10), and blinding of outcome assessment (60%, 6/10). Eight studies mentioned that blinding participants were not possible owing to the nature of aromatherapy [17,19- 22,25-27]. Four trials from five reports have performed interventions on randomly allocated days; thus, we considered these four trials as quasi-RCTs [17,20,21,23,24] (Figure 2).
Figure 2:Risk of bias summary.
Aromatherapy interventions
Table 1 presents details of the aromatherapy interventions administered in each trial. All trials evaluated inhalation of aroma essence in labor. Two studies had a three-arm design with intervention arms [21,22]. One study used two kinds of aroma essence (Jasmin and Salvia essence), and we combined them into one group and used the calculated data which is the combined mean ±SD [21]. Another study carried out interventions by inhalation of aroma essence using a footbath, only footbath, and routine care [22]. We included inhalation of aroma essence with footbath as the intervention group, and only footbath as the control group to exclude the effect from footbath. Moreover, one study performed inhalation of aroma essence with breath technique as the intervention, and breath technique alone as the control [19].
Various aroma essences were used in the included trials. Lavender was the most used aroma oil in four trials, and it is also commonly used in practice settings [19,20,26,27]. The second most used aroma essences were C. aurantium essence, Geranium rose essence, Jasmin, and R. damascene essence in two trials each, and Salvia essence and Boswellia carterii essence were used in single trials each [17,18,21-26].
Primary outcomes
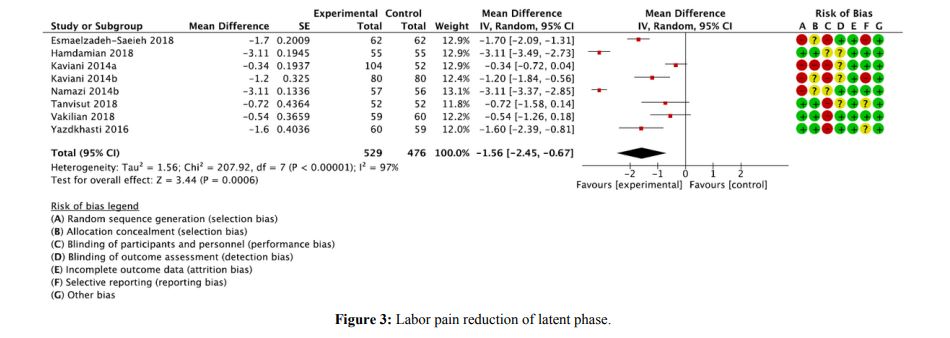
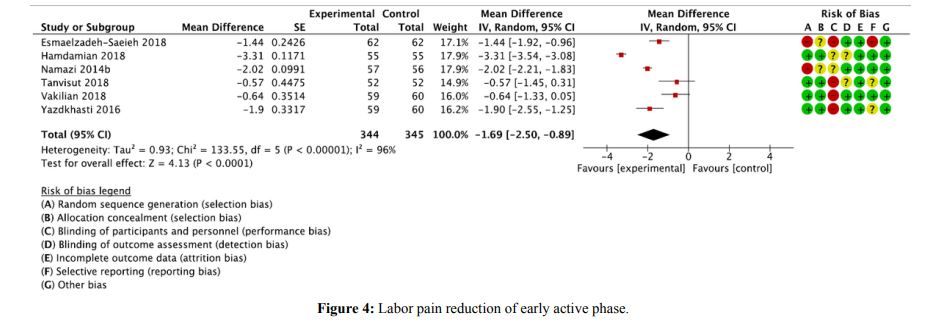
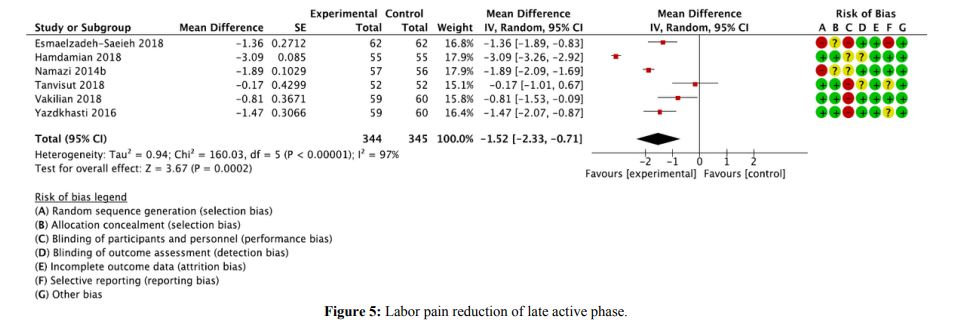
Labor pain relief: For the measurement of labor pain, all of the studies used VAS or NRS [17-21,24,26,27]. As one trial reported interquartile range we used score change reports [26]. For this reason, we calculated MD with GIVM for the analysis of labor pain. Eight studies found that aromatherapy significantly reduced labor pain intensity compared with control in the latent phase (MD -1.56, 95% CI -2.45 to -0.67, p = 0.0006, I2 =97%, eight trials, 1,005 women, low certainty of evidence; Figure 3). Six studies reported that aromatherapy intervention significantly reduced labor pain compared with control in the early active phase (MD -1.69, 95% CI -2.50 to -0.89, p < 0.0001, I2 = 96%, six trials, 689 women, low certainty of evidence; Figure 4). These studies also reported that aromatherapy significantly reduced labor pain in the late active phase (MD -1.52, 95% CI -2.33 to -0.71, p = 0.0002, I2 = 97%, six trials, 689 women, very low certainty of evidence; Figure 5).
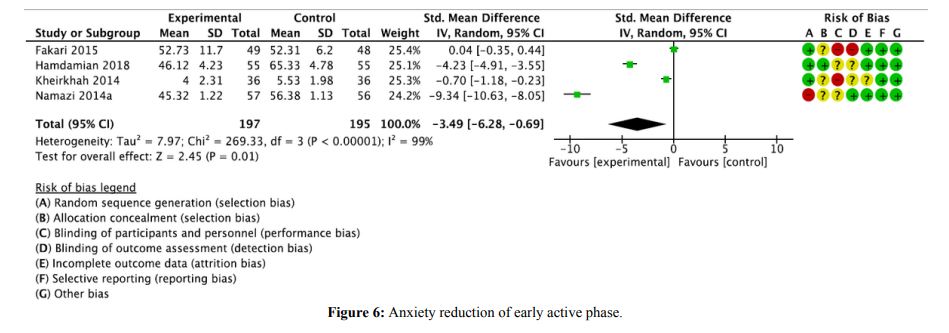
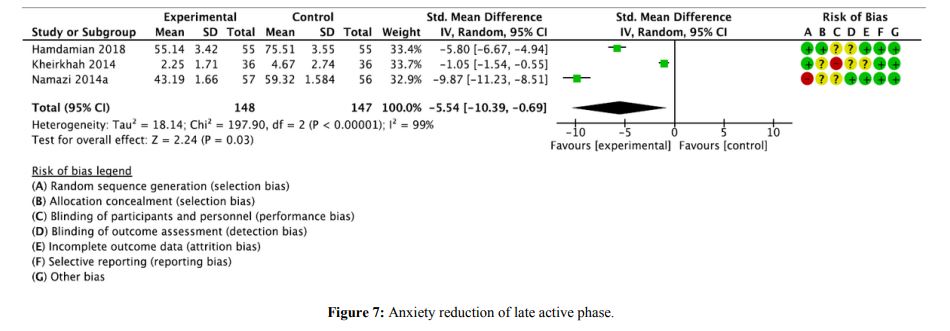
Anxiety relief: Three studies used STAI and one study used VASA to measure the outcome of anxiety [18,23,22,25]. Therefore, we calculated SMD for the analysis of anxiety. Aromatherapy intervention reduced anxiety compared with the control in the early active phase (SMD -3.49, 95% CI -6.28 to -0.69, p = 0.01, I2 = 99%, four studies, 392 women, very low certainty of evidence; Figure 6). Three studies reported that aromatherapy significantly reduced anxiety in the late active phase. (SMD -5.54, 95% CI -10.39 to -0.69, p = 0.03, I2 = 99%, three studies, 295 women, very low certainty of evidence; Figure 7).
Secondary outcomes
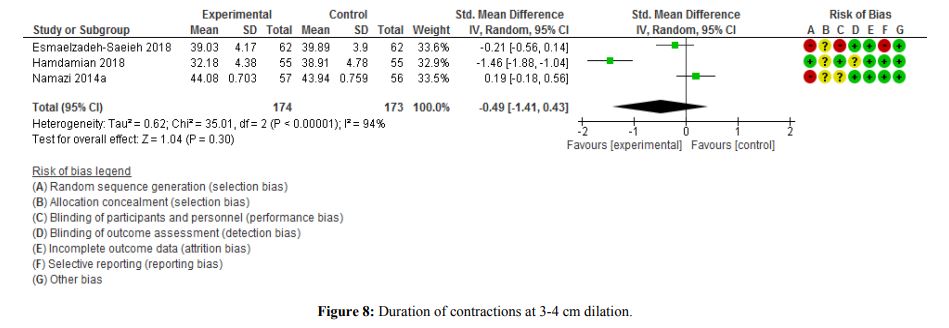
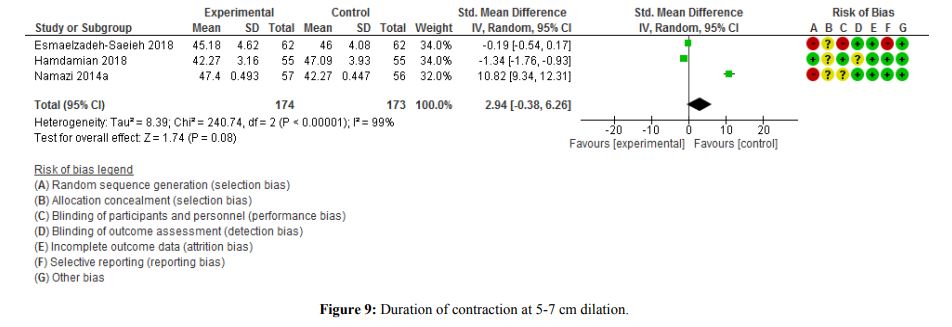
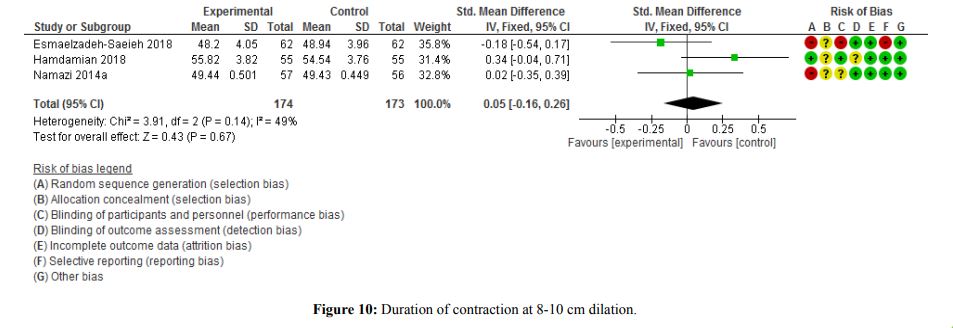
Duration of contraction: We used SMD for the analysis of duration of contraction because the time unit of the included studies was unclear [17,18,23]. Three studies found that aromatherapy did not significantly affect the duration of contractions at 3-4 cm, 5-7 cm, and 8-10 cm dilatation (3-4 cm; SMD -0.49, 95% CI -1.41 to 0.43, p = 0.30, I² = 94%, 347 women), (5-7 cm; SMD 2.94, 95% CI -0.38 to 6.26, p = 0.08, I² = 99%, 347 women), (8-10 cm; SMD 0.05, 95% CI -0.16 to 0.26, p = 0.67, I² = 49%, 347 women).
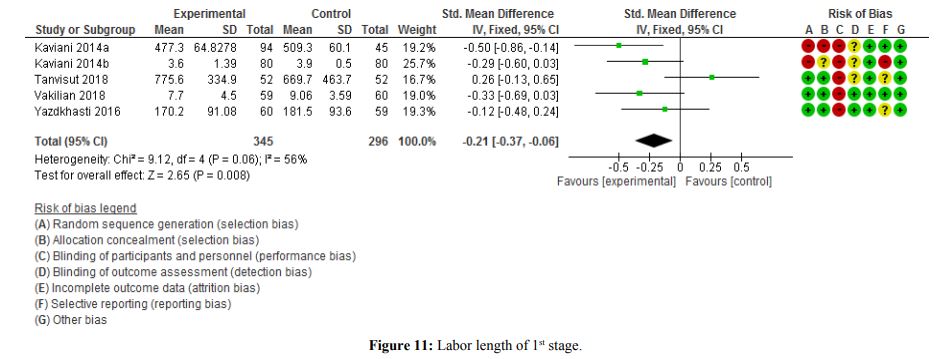
Labor length: We also used SMD for the analysis of labor length as the time unit was unclear [19-21,26,27]. Five studies showed that aromatherapy significantly reduced the 1st stage labor length compared with the control (SMD -0.21, 95% CI -0.37 to -0.06, p = 0.008, I2 = 56%, five studies, 641 women). By contrast, aromatherapy did not significantly reduce the 2nd stage labor length (SMD 0.14, 95% CI -0.36 to 0.63, p = 0.59, I2 = 86%, four studies, 481 women).
Figure 3:Labor pain reduction of latent phase.
Figure 4: Labor pain reduction of early active phase.
Figure 5: Labor pain reduction of late active phase.
Apgar score: Aromatherapy intervention did not significantly affect the Apgar score at 1 min after delivery (MD -0.25, 95% CI -0.84 to 0.35, p = 0.41, I² = 98%, five studies, 652 women) [17,18,20,21,27]. These five studies also report that aromatherapy was not significantly associated with the Apgar score at 5 min (MD 0.03, 95% CI -0.02 to 0.08, p = 0.25, I² = 0%, five studies, 652 women).
We calculated RR for dichotomous results. Only one study reported Apgar score < 7 at 1 min; however, there was no significant association with aromatherapy (RR 0.51, 95% CI 0.05 to 5.45, p = 0.58, one study, 103 women). An Apgar score < 7 at 5 min was not reported [26].
Types of delivery: Three studies reported that aromatherapy intervention did not increase spontaneous delivery (RR 1.05, 95% CI 0.96 to 1.15, p = 0.27, I² = 0%, three studies, 370 women) [18,21,26]. Aromatherapy did not significantly reduce operative delivery (RR 0.58, 95% CI 0.24 to 1.42, p = 0.24, I² = 0%, two studies, 214 women), or C-sections (RR 0.83, 95% CI 0.47 to 1.49, p = 0.54, I² = 0%, four studies, 483 women) [18,21,23,26].
Labor augmentation: Only one study reported the ratio of labor augmentation [26]. Aromatherapy did not significantly reduce labor augmentation (RR 0.97, 95% CI 0.68 to 1.37, p = 0.84, one study, 104 women).
Sensitivity analysis
Due to the high heterogeneity, we performed sensitivity analysis by excluding quasi-RCTs and high risk of random sequence [17,20,21,23,24]. For labor pain relief, it still showed significant differences during the latent and early active phase. However, there were no significant differences in pain relief during the late active phase, and anxiety relief during all of the active stages. For secondary outcomes, there was no significant difference in the labor length of the 1st stage.
Discussion
We found evidence that using inhalation aromatherapy for term pregnancy women was associated with reduction of labor pain on the latent and early active phase. This is most likely the first review showing evidence of pain relief with the use of aromatherapy in labor, and the first study to evaluate the efficacy of aromatherapy in all the stages of labor. The Cochrane systematic review included two RCTs [32,33]. However, the researchers could not perform a meta-synthesis owing to the differences in the comparison methods, and they reported each trial result individually. This previous review could not identify any evidence of the effects of aromatherapy on pain relief in labor because the number of included studies were not sufficient. Furthermore, the searches were conducted in 2010 [3]. In the present review, there was insufficient evidence regarding the effect of reducing anxiety of the participants using inhalation aromatherapy during labor. Ghiasi et al. reported the systematic review on the anxiolytic effect of aromatherapy during the first stage of labor [7]. They suggested a positive effect on anxiety with an analysis of the benefit from individual aroma essence oils in the first stage of labor qualitatively. This previous review also did not perform meta-analysis, thus this review was not conclusive [7]. Moreover, Ghiasi et al. included trials of aromatherapy intervention with massage. In the present review, we excluded data that may exert any effect on the evaluation of the genuine efficacy of aromatherapy.
Thus, our hypothesis that the use of aromatherapy during labor reduces labor pain was found to be effective in pregnant women on the latent and early active phase, and we considered a low certainty of evidence from the GRADE assessment (Table 2). The Cochrane review reported outcomes of assisted vaginal delivery, cesarean delivery, spontaneous delivery, augmentation, and admission to NICU, and there was no evidence of effect due to the lack of power [3]. Taken together, there were no significant differences in the secondary outcomes, such as duration of contraction, labor length, Apgar score, types of delivery, labor augmentation in our present review. Moreover, there was no report about adverse events of aromatherapy in the included studies. However, people have different preferences of smell, and pregnant women are particularly more sensitive. The choice of essential oils depends on the women’s preference.
Overall, the risk of bias about blinding allocation of the included studies were high. Blinding allocations of the participants and care providers are difficult because of the smell of the aroma essence. This setting downgrades the level of evidence. Four trials of random sequence also had a high risk of bias. We conducted sensitivity analysis to adjust for the effects of this high risk of bias of randomization. The results showed high heterogeneities overall in the outcomes of pain as well as reduction of anxiety. In another review, labor pain intensity was also reported with high heterogeneity [34]. Pain and anxiety are subjective senses, and these outcomes were assessed by self-report questionnaires. Additionally, it is predictable that there are various individual differences in sensitivity to labor pain. These various differences may provoke a high heterogeneity status.
We did not specify the kinds of aroma essence although eight kinds of essences were used in the included studies. We cannot define the specific efficacy of aromatherapy in this present review. It is possible that what influenced the reduction in the subjective labor pain was the efficacy of relaxation brought about by the inhalation of pleasant smells of the aroma essence. A women’s internal experience of labor pain is affected by the environment, and this factor includes the person’s verbal and nonverbal communications [35]. Relaxation may have a role in reducing pain, increasing satisfaction with pain relief, and reducing the rate of assisted vaginal delivery [36]. Creating an environment with less stress and providing relaxation to parturient women are needed to reduce pain intensity.
Moreover, there is a strong association between anxiety and pain in the latent phase of labor [37]. Although we could not find sufficient evidence of reducing anxiety by aromatherapy, the results showed a tendency for aromatherapy to be slightly more effective than the control group. From this point of view, even if we could not reach definitive evidence of anxiety relief in this present review, there were still benefits of using aromatherapy in labor.
For women, natural pain and anxiety interventions are more demanding than medical intervention. Aromatherapy is a noninvasive method with a low risk and low cost for reducing labor pain.
Figure 6: Anxiety reduction of early active phase.
Figure 7: Anxiety reduction of late active phase.
| Authors | Location | Study Type | Sample Size Intervention/ Control |
Subject | Oil | Intervention Methods |
Control | Outcome Reported |
|---|---|---|---|---|---|---|---|---|
| Namazi.2014a | Iran | Quasi-RCT | 113 57/56 | Iranian primiparous women, 18-35 years old, term, singleton pregnancy, cephalic presentation, spontaneous contractions |
C. aurantium | Gauze squares were soaked in 4ml of C. aurantium distillated water was attached to the respective patient’s collar. | Gauze squares were soaked in 4ml of normal saline was attached to the respective patient’s collar | Pain score before intervention, 3-4cm dilatation 5-7cm dilatation 8-10 cm dilatation |
| Namazi.2014b | Iran | Quasi-RCT | 113 57/56 | Iranian primiparous women, 18-35 years old, term, singleton pregnancy, cephalic presentation, spontaneous contractions | C. aurantium | Gauze squares were soaked in 4ml of C. aurantium distillated water was attached to the respective patient’s collar. | Gauze squares were soaked in 4ml of normal saline was attached to the respective patient’s collar. | Contraction length (3-4cm/ 5-7cm/ 8-10cm dilatation) Contraction frequency during 10 min (3-4cm/ 5-7cm/ 8-10cm dilatation) Anxiety score before intervention, 3-4cm/ 6-8cm dilatation |
| Fakari. 2015 | Iran | RCT | 97 49/48 | Nulliparous, full term pregnant, 18-35years of age | Geranium | Two drops of 2% concentrated geranium essential oil were used, the essences were dropped onto similar odorless nonabsorbent pieces of fabric attached to the participant's collar. | Two drops of distilled water were used, the essences were dropped onto similar odorless non-absorbent pieces of fabric attached to the participant's collar. | STAI Systolic blood pressure(mmHg) Diastolic blood pressure (mmHg) Pulse rate Respiration rate (before intervention, after 20min intervention) |
| Kaviani. 2014a | Iran | Quasi-RCT | 156 52/52/52 Jasminium/ Salvia/ control | Nulliparous women, physically healthy aged 18-30 years singleton pregnancy cephalic pregnancy 37th week of pregnancy or higher in the active phase no methods of analgesia, anesthesia, or sedation during labor | Jasminium Officinale, Salvia Officinale | The incense had a mask with a height of 20 cm on which the person was asked to keep her face (the distance between the face and the device was 20 cm). Use 3ml of the extract. | Water had a mask with a height of 20 cm on which the person was asked to keep her face (the distance between the face and the device was 20 cm). Use 5ml of water | Pain: Before, 30 min/ 60 min after intervention Duration of Labor First stage, Second stage Labor type Normal vaginal delivery, Cesarean Section APGAR Score 1 min, 5 min |
| Yazdkhasti. 2016 | Iran | RCT | 119 59/60 | Nulliparous pregnant women, singleton pregnancy, gestational age over 37 weeks, cephalic presentation, receiving no analgesia during labor | Lavender angustifolia | Drop the essence on to the patient's palm, then rub their hands together and inhale the scent for 3 min while the hands were 2.5-5 cm distance from the nose. The pain intensity of the subjects was measured 30 min after the contraction ended. The intervention was carried out in 3 phases (dilatation 5-6, 7-8, and 9-10cm). | In the control group were treated with distilled water as a placebo in a similar way. | Pain intensity; VAS before the intervention (dilatation 3-4cm, 5-6 cm, 7-8 cm, 9-10cm). Apgar score first and fifth minutes |
| Kheirkhah. 2014 | Iran | RCT | 108 36/ 36/ 36 | Nulliparous women, gestational age of 38-42weeks, cephalic presentation, 3 cm dilatation | Rose | In the first case, inhalation and footbath with essential oil, rose essential decrease of 1%, which was evaporated for 10 minutes, simultaneously a footbath with rose essential oil with 1% water, 40°C for 10 minutes was performed. In the second group, mothers placed their feet for 10 minutes in a footbath containing 40°C water. Interventions were performed once at the beginning of the active phase (cervical dilatation 4cm) and secondly at the beginning of the transition phase (8cm dilatation) | The control group received routine care of the delivery room. | Anxiety before and after each intervention. after: active and transitional phase. |
| Tanvisut. 2018 | Thailand | RCT | 104 52/52 | Primigravida, singleton pregnancy, term pregnancy (gestational age between 37 and 41 weeks), cephalic presentation, spontaneous true labor, defined by regular uterine contraction more than three times in 10 min with cervical progression. | Lavender, Geranium rose, Citrus, Jasmine (four options) | Aromatherapy group was offered four options of the aroma favors to choose (lavender, geranium rose, citrus and jasmine). Aroma oil was diffused continuously by aroma diffusers using standard concentration at four drops of aroma oil per 300 ml of diffused water. The aromatherapy was started when the participants were admitted for going on labor until the end of first stage of labor. | standard care | Pain score baseline: pain scores on admission latent phase: cervical dilatation of 3-4 cm early active phase: cervical dilatation of 5-7 cm late active phase: cervical dilatation of 8-10 cm Length of labor Route of delivery Apgar score |
| Hamdamian.2018 | Iran | RCT | 110 55/ 55 | No history of allergy, a singleton, full term, noncomplicated, cephalic pregnancy | R. damascena | During treatment, 10×10 cm cotton gauze pad was attached to each participant's collar. This pad, was dosed with 2 drops of treatment compound, either essence of R. damascena. | During treatment, 10×10 cm cotton gauze pad was attached to each participant's collar. This pad, was dosed with 2 drops of treatment compound, either essence of normal saline. | Pain score baseline: on admission latent phase: cervical dilatation of 3-4 cm early active phase: cervical dilatation of 5-7 cm late active phase: cervical dilatation of 8-10 cm Labor augmentation Length of labor Route of delivery Apgar score |
| Vakilian. 2018 | Iran | RCT | 119 59/ 60 | Singleton pregnancy, planned normal delivery without any complications, gestational age more than 37 weeks, cervical dilatation greater than 4 cm without using oxytocin | Lavender | At the beginning and end of each contraction, the participants were reminded to take a deep, cleansing and relaxing breath. Breathing was done through the mouth in fast shallow breaths at a rate of 15 to 20 breaths during each contraction. Mothers inhaled lavender via nebulizer connected to a mask. | In the control group, the breathing technique was used only with saline water. | Pain: using VAS cervical dilatation 4-6 cm, 7-8 cm, 9-10 cm |
| EsmalzadehSaeieh. .2018 | Iran | Quasi-RCT | 124 62/ 62 | Iranian nationality, nulliparity, term pregnancy, singleton pregnancy, cephalic presentation, spontaneous uterine contractions, cervical dilatation of 6-4 cm, no obstetric complications, receiving no pain medications during the last 8h before the study | Boswellia carteii (BC) oil | A piece of gauze was soaked with 0.2ml of 0.2% BC essential oil diluted in 2 ml if normal saline, and then, it was attached to the collar of each woman. The intervention was repeated for each woman every 30 min up to a cervical dilatation of 10cm. | In the control group, the gauze was soaked just with 2 ml of normal saline. | Pain intensity before the intervention, cervical dilatation of 3-4 cm, 5-7 cm, 8-10 cm. Apgar score |
| Kaviani. 2014b | Iran | semiexperimental clinical trial | 160 80/ 80 | Primiparous pregnant women at 36 weeks or more gestation, singleton pregnancy, 3-4cm dilatation | Lavender officinalis | In the aroma group, 15 ×15 cm tissues containing 0.1ml of lavender essence mixed with 1 ml of distilled water were used. In addition, cotton fabrics were used in order to maintain the aromas. | The control group inhaled 2ml of distilled water under the same conditions. | Pain severity before intervention, after 30min, 60 min intervention Frequency of contentment test Apgar score |
| RCT: Randomized Controlled Trials; STAI: state-trait anxiety inventory; VAS: Visual Analogue Scales | ||||||||
Table1: Characteristics of included studies.
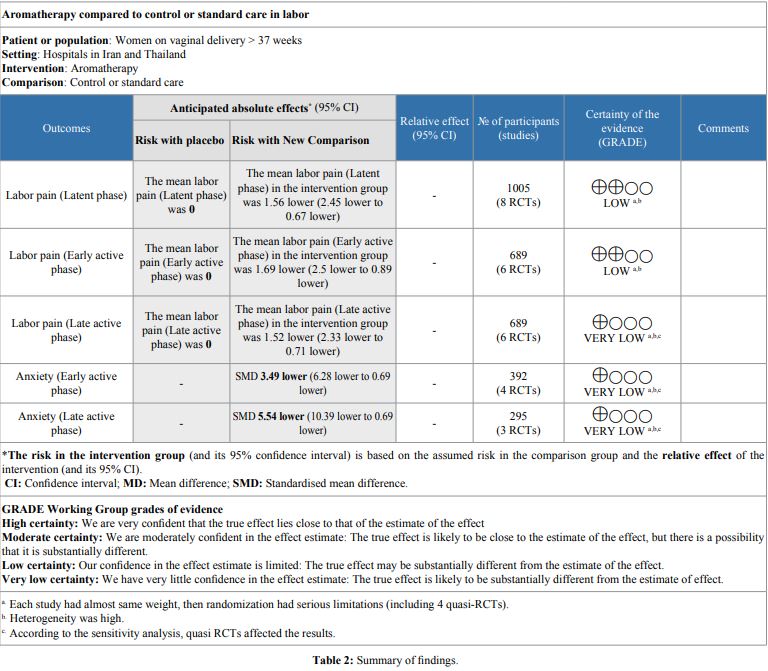
Figure 8: Duration of contractions at 3-4 cm dilation.
Figure 9: Duration of contraction at 5-7 cm dilation.
Figure 10: Duration of contraction at 8-10 cm dilation.
Figure 11: Labor length of 1st stage.
Strength and Limitations
This present review has several strengths. Almost all included studies used genuine branded aroma oils for women in labor, thus it is sufficient to say that most of the outcomes are reliable in terms of their efficiency. Only one study had an unclear attrition bias [22]. This included study reported the number of assigned participants, but not the number of randomized participants. However, other included reports all had a low risk of bias in incomplete outcome data, and also other bias was low in this review. From this status, we considered that the quality of evidence in the present review was kept from attrition bias. This systematic review provides the results of all outcomes following aromatherapy in all stages of labor. Although we could not assess the differences in the efficacies of individual essential oils, Ghiasi et al. reported the efficacy of aromatherapy on anxiety for each aroma oil [7]. Investigating differences in the effectiveness of essential oils on labor pain should also be considered.
Despite these strengths, several limitations were found in the present review. Firstly, the nine studies out of the 10 reports for inclusion in the final review were conducted in Iran. The results of these studies might be impacted by its bias. Secondly, all studies could not keep the blinding of participants because the essential oil fragrance naturally spreads in the air and prevents from complete blinding of the participants. Additionally, this study was able to examine the effectiveness of aromatherapy, and found a possible effect for reducing women’s labor pain. Although there was a positive result on pain relief, it is very difficult to evaluate this objectively because the perception of pain is very subjective and results from various internal experiences. Women in labor experience a significant amount of discomfort rather than labor pain, but the included studies were not focused on those unpleasant symptoms such as nausea, excessive physical sensitivity, vomiting, and other discomforts.
Future research is needed not only in terms of physiological labor pain but also psychological efficacy (e.g., stress response changes or anxiety). The former Cochrane review concluded that the efficacy and effectiveness of aromatherapy have not yet been established owing to the limited the number of trials [3]. Our included studies were comparatively new, and we updated the efficacy for pain reduction.
Further research of the evaluation of aromatherapy about these three points are needed. Firstly, the included studies were concentrated in Iranian settings, and future research should be investigated in other various settings. Secondly, the types of aroma essence were not specified in this review, and future research should assess the efficacy of the specific kinds of aroma oils. Thirdly, future research should investigate additional outcomes such as nausea, excessive physical sensitivity, vomiting, and other discomforts. Anxiety and discomforts, which are experienced during labor, may be related to psychological status. Future research is needed to focus on the psychological efficacy of aromatherapy.
Conclusion
The use of aromatherapy during labor and delivery has continued to expand in practice settings. There was a low certainty of evidence of subjective labor pain reduction by inhalation aroma essence on the latent and early active phase. However, other outcomes such as pain relief on the late active phase, anxiety relief, duration of contraction, labor length, types of delivery, labor augmentation, and the Apgar score of infants could not reach the level of evidence indicating the definitive effectiveness of aromatherapy. Some discomforts during child birth are related to pain, and this feeling of pain may be reduced following aromatherapy.
Acknowledgement
We thank Dr. Farhad Shokraneh for assistance in the study search. We also thank Dr. Edward F. Barroga and Dr. Sarah E. Porter for advice in writing the paper.
Trial Registration
We registered the study protocol with PROSPERO (CRD42017077617).
Lowdermilk DL, Perry SE, Cashion K, Alden KR, Olshansky EF (2016) Maternity & women’s health care. Elsevier. [ Ref ]
Miller RD, Eriksson L, Fleishr L, Wiener-Kronish J, Young W (2010) Miller’s Anesthesia. Elsevier, Philadelphia.[ Ref ]
Smith CA, Collins CT, Crowther CA (2011) Aromatherapy for pain management in labour. Cochrane Database Syst Rev 7: CD009215.[ Ref ]
Domingos Tda S, Braga EM (2015) Massage with aromatherapy: effectiveness on anxiety of users with personality disorders in psychiatric hospitalization. Rev Esc Enferm USP 49: 453-459.[ Ref ]
Lakhan SE, Sheafer H, Tepper D (2016) The effectiveness of aromatherapy in reducing pain: a systematic review and meta-analysis. Pain Res Treat 2016: 1-13.[ Ref ]
Go GY, Park H (2017) Effects of aroma inhalation therapy on stress, anxiety, depression, and the autonomic nervous system in high-risk pregnant women. Korean J Women Health Nurs 23: 33-41.[ Ref ]
Ghiasi A, Bagheri L, Haseli A (2019) A systematic review on the anxiolytic effect of aromatherapy during the first stage of labor. J Caring Sci 8: 51-60.[ Ref ]
Lefebvre C, Manheimer E, Glanville J (2011) Chapter 6: Cochrane handbook for systematic reviews of interventions. The Cochrane Collaboration.[ Ref ]
Higgins J, Lasserson T, Chandler J, Tovey D, Churchill R (2016) Methodological expectations of cochrane intervention reviews. Cochrane, London.[ Ref ]
Moher D, Liberati A, Tetzlaff J, Altman DG, Group TP (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Medicine 6: 1-6.[ Ref ]
McGowan J, Sampson M, Salzwedel DM, Cogo E, Foerster V, et al. (2016) PRESS peer review of electronic search strategies: 2015 guideline statement. J Clin Epidemiol 75: 40-46.[ Ref ]
Nourbakhsh S, Taavoni S (2012) P-910 - Effect of aromatherapy on labor pain: a randomized control trial study in bandarabbas, year 2010. Eur Psychiatry 27: 1.[ Ref ]
Nourbakhsh S, Darsareh F (2012) Randomized trial evaluating the aroma inhalation on the duration of labor. J Gynecol & Obstet 119S3: S531-S867.[ Ref ]
Tabatabaeichehr M, Rashidi-Fakari F, Mortazavi H (2015) The effect of aromatherapy by essential oil of orange on anxiety during labor: a randomized clinical trial. Iran J Nurs Midwifery Res 20: 661.[ Ref ]
Review Manager (RevMan) (2014) Copenhagen: The Nordic Cochrane Centre. The Cochrane Collaboration.[ Ref ]
GRADE pro GDT: GRADE pro Guideline Development Tool (2015) McMaster University (developed by Evidence Prime, Inc.).[ Ref ]
Esmaelzadeh-Saeieh S, Rahimzadeh M, Khosravi-Dehaghi N, Torkashvand S (2018) The effects of inhalation aromatherapy with Boswellia carterii essential oil on the intensity of labor pain among nulliparous women. Nurs Midwifery Stud 7: 45-49.[ Ref ]
Hamdamian S, Nazarpour S, Simbar M, Hajian S, Mojab F, et al. (2018) Effects of aromatherapy with Rosa damascena on nulliparous women’s pain and anxiety of labor during first stage of labor. J Integr Med 16: 120-125.[ Ref ]
Vakilian K, Keramat A, Gharacheh M (2018) Controlled breathing with or without lavender aromatherapy for labor pain at the first stage: a randomized clinical trial. Crescent J Med Biol Sci 5: 172-175.[ Ref ]
Kaviani M, Azima S, Alavi N, Tabaei MH (2014b) The effect of lavender aromatherapy on pain perception and intrapartum outcome in primiparous women. Br J Midwifery 22: 125-128.[ Ref ]
Kaviani M, Maghbool S, Azima S, Tabaei MH (2014a) Comparison of the effect of aromatherapy with Jasminum officinale and Salvia officinale on pain severity and labor outcome in nulliparous women. Iran J Nurs Midwifery Res 19: 666-672.[ Ref ]
Kheirkhah M, Vali Pour NS, Nisani L, Haghani H (2014) Comparing the effects of aromatherapy with rose oils and warm foot bath on anxiety in the first stage of labor in nulliparous women. Iran Red Crescent Med J 16: e14455.[ Ref ]
Namazi M, Amir Ali Akbari S, Mojab F, Talebi A, Alavi Majd H, et al. (2014a) Aromatherapy with citrus aurantium oil and anxiety during the first stage of labor. Iran Red Crescent Med J 16: e18371.[ Ref ]
Namazi M, Akbari SAA, Mojab F, Talebi A, Majd HA, et al. (2014b) Effects of citrus aurantium (bitter orange) on the severity of first-stage labor pain. Iran J Pharm Res 13: 1011-1018.[ Ref ]
Rashidi Fakari F, Tabatabaeichehr M, Kamali H, Rashidi Fakari F, Naseri M (2015) Effect of inhalation of aroma of geranium essence on anxiety and physiological parameters during first stage of labor in nulliparous women: a randomized clinical trial. J Caring Sci 4: 135-141.[ Ref ]
Tanvisut R, Traisrisilp K, Tongsong T (2018) Efficacy of aromatherapy for reducing pain during labor: a randomized controlled trial. Arch Gynecol Obstet 297: 1145-1150.[ Ref ]
Yazdkhasti M, Pirak A (2016) The effect of aromatherapy with lavender essence on severity of labor pain and duration of labor in primiparous women. Complement Ther Clin Pract 25: 81-86.[ Ref ]
McCormack H, Horne D, Sheather S (1988) Clinical applications of visual analogue scales: a clinical review. Psychol Med 18: 1007-1019.[ Ref ]
Farrar JT, Troxel AB, Stott C, Duncombe P, Jensen MP (2008) Validity, reliability, and clinical importance of change in a 0-10 numeric rating scale measure of spasticity: a post hoc analysis of a randomized, doubleblind, placebo-controlled trial. Clin Ther 30: 974-985.[ Ref ]
Quek KF, Phil M, Low WY, Razack AH, Loh CS, et al. (2004) Reliability and validity of the Spielberger State-Trait Anxiety Inventry (STAI) among urological patients: a Malaysian study. Med J Malaysia 59: 258-267.[ Ref ]
Hornblow AR, Kidson MA (1976) The visual analogue scale for anxiety: a validation study. Aust N Z J Psychiatry 10: 339-341.[ Ref ]
Burns E ZV, Panzeri D, Oskrochi R, Regalia A (2007) Aromatherapy in childbirth: a pilot randomised controlled trial. British Journal of Obsetrics and Gynaecology 114: 838-844.[ Ref ]
Calvert I (2005) Ginger: an essential oil for shortening labour? Practising Midwife 8: 30-34.[ Ref ]
Smith CA, Levett KM, Collins CT, Dahlen HG, Ee CC, et al. (2018) Massage, reflexology and other manual methods for pain management in labour. Cochrane Database Syst Rev 15: CD009290.[ Ref ]
Pirdel M, Pirdel L (2009) Perceived environmental stressors and pain perception during labor among primiparous and multiparous women. J Reprod Infertil 10: 217-223.[ Ref ]
Smith CA, Levett KM, Collins CT, Armour M, Dahlen HG, et al. (2018) Relaxation techniques for pain management in labour. Cochrane Database Syst Rev 2018: CD009514.[ Ref ]
Floris L, Irion O (2013) Association between anxiety and pain in the latent phase of labour upon admission to the maternity hospital: a prospective, descriptive study. J Health Psychol 20: 446-455.[ Ref ]